Congenital heart malformations are the most common cause of fetal and infant mortality, with an incidence of 4-13 per 1000 live births. Antenatal ultrasound evaluation of the fetal heart has developed over the past 30 years, and has allowed the detection of many abnormalities in the first trimester of pregnancy. Prenatal screening for fetal malformations is mandatory, allowing a better pregnancy counseling and greatly improving the neonatal prognosis. According to the Romanian Society of Obstetrics and Gynecology (SOGR), the evaluation of the fetal heart starting from the first trimester of pregnancy is mandatory. Due to technological advances, the fetal heart can be assessed in detail as early as the first trimester, which allows for adequate counseling of the couple facing a malformative heart pathology in their fetus, allows the termination of pregnancy at a legally optimal gestational age, or, when the ultrasound assessment does not reveal any fetal malformation, it assures the couple about the normal course of the pregnancy. The evaluation of the fetal heart using standard plans of examination is performed in each trimester of pregnancy. We present a series of cardiac malformations detected antenatally in our clinic, using standard assessment views. The purpose of this study is to emphasize that most lesions involving the ejection tracts of the arteries at the base of the heart are associated with varying degrees of disruption of the alignment, arrangement, size, or number of the three vessels, thus with an abnormal appearance of the standard cross-section of three vessels. In all cases, the three-vessel view of the heart revealed an abnormal appearance, helping us to diagnose major cardiac malformations. This plan can be easily obtained in all trimesters of pregnancy, providing sufficient information to detect many major conotruncal malformations.
Three-vessel and trachea view – important marker in the diagnosis of great vessels anomalies
Imaginea de 3 vase şi trahee – marker important în anomaliile de vase mari
First published: 28 martie 2024
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.43.1.2024.9416
Abstract
Rezumat
Malformaţiile cardiace congenitale reprezintă cea mai frecventă cauză de mortalitate fetală şi infantilă, cu o incidenţă de 4-13 la 1000 de născuţi vii. Evaluarea ecografică antenatală a cordului fetal s-a dezvoltat în ultimii 30 de ani şi a permis detectarea multor anomalii în primul trimestru de sarcină. Screeningul prenatal al malformaţiilor fetale este obligatoriu, permiţând o consiliere mai bună asupra sarcinii şi îmbunătăţind considerabil prognosticul neonatal. Potrivit Societăţii Române de Obstetrică şi Ginecologie (SOGR), evaluarea cordului fetal începând cu primul trimestru de sarcină este obligatorie. Datorită progreselor tehnologice, cordul fetal poate fi evaluat în detaliu încă din primul trimestru, fapt ce permite o consiliere adecvată cuplului care se confruntă cu o patologie cardiacă malformativă a fătului lor, permite întreruperea sarcinii la o vârstă gestaţională optimă din punct de vedere legal sau, atunci când evaluarea ecografică nu evidenţiază nicio malformaţie fetală, asigură cuplul cu privire la parcursul normal al sarcinii. Evaluarea cordului fetal cu ajutorul planurilor standard de examinare se face în fiecare trimestru de sarcină. Prezentăm o serie de malformaţii cardiace detectate antenatal în clinica noastră, prin utilizarea planurilor standard de evaluare. Scopul acestui studiu este de a sublinia faptul că majoritatea leziunilor care implică tracturile de ejecţie ale arterelor de la baza cordului sunt asociate cu diferite grade de perturbare a alinierii, aranjamentului, mărimii sau numărului celor trei vase, deci cu un aspect anormal al secţiunii standard de trei vase. În toate cazurile, imaginea de trei vase a cordului a evidenţiat un aspect anormal, ajutându-ne la diagnosticarea unor malformaţii cardiace majore. Acest plan poate fi obţinut cu uşurinţă în toate trimestrele de sarcină, oferind suficiente informaţii pentru a detecta malformaţiile conotruncale majore.
Introduction
According to the literature, congenital heart disease (CHD) represents the most common congenital malformation, a leading cause of fetal and infant mortality, with an incidence of 4-13 per 1000 live births. Fetal heart assessment by using ultrasound techniques has advanced in the last 30 years, and it triggered the detection of many anomalies in the first trimester of pregnancy. CHD prenatal diagnosis is mandatory, allowing better pregnancy counseling and an improved neonatal outcome. During the last decades, efforts have been made to standardize the approach to the sonographic assessment of the fetal heart by elaborating clear guidelines that are regularly updated and reviewed constantly. It is, therefore, important for healthcare providers to refer to the most recent version of these national and international guidelines to be up-to-date with the latest information.
Consequently, it is crucial to have clear definitions of various terms used in practice to uniformize the language of all personnel performing ultrasound examinations, standardize the examination, reduce variations in practice, and provide a rational basis for study referral.
According to the Romanian Society of Obstetrics and Gynecology (SOGR), it is mandatory to assess the fetal heart starting with the first trimester of pregnancy during the nuchal scan at 11-13(+6) weeks of pregnancy. Due to technological advancements, such as high-frequency transvaginal scanning, the fetal heart assessment has shifted from the second trimester of pregnancy to the first trimester, at a level in which fetal heart development can be evaluated in detail. Still, in most countries, the fetal anatomy is evaluated during the mid-trimester of pregnancy. In all trimesters of pregnancy, there can be used a basic protocol – using standard planes, and an extended protocol – using additional planes, dependent on the sonographer’s skills and the equipment used to assess the fetal anatomy.
The main goal of the fetal ultrasound assessment is to provide accurate information to offer the mother and the fetus the best antenatal care and to obtain the best outcomes for the pregnancy. Early detection of fetal heart anomalies offers the couple a safer termination of pregnancy within the legal term, or in cases of normal scan, and it reassures the families that a major anomaly is unlikely to be present. Some anomalies, such as cardiac tumors, complete heart block, cardiomyopathies, coarctation of the aorta, total anomalous pulmonary venous return and aortic or pulmonary stenosis, are not evident until later in pregnancy, some of them going undetected even at the mid-trimester scan. The detection rates of fetal heart anomalies can be optimized by performing a comprehensive ultrasound evaluation, recognizing that the four-chamber view accounts for more than a simple count of cardiac chambers, understanding that some anomalies may be detected later in pregnancy, some may not be evident in the four-chamber plane alone, and should be complemented with the outflow tracts views which play a crucial role in the detection of the congenital heart defects. Accordingly, the fetal heart should be assessed in all trimesters of pregnancy. The detection of these anomalies can be lifesaving, as it can provide optimal perinatal and perioperative management.
We are presenting a number of prenatal cardiac malformation detected in our clinic by using standard planes of assessment, especially the three-vessel and trachea (3VT) view. The purpose of this study is to emphasize that the majority of lesions involving the ventricular outflow tracts and great arteries are associated with various degrees of disturbance in alignment, arrangement or size or number of the three vessels. Moreover, adding new planes, such as left and right ventricular outflow tracts and three-vessel and trachea view, compensates the weakness of the four-chamber view alone in the antenatal detection of cardiac malformations.
The evaluation of the great vessels in the upper thorax in axial planes was first described almost 40 years ago, in the mid-1980. The three-vessel view is an axial plane showing the main pulmonary artery, the ascending aorta and the superior vena cava. The three-vessel and trachea view (3VTV) is a slightly oblique plane describing the transverse main pulmonary artery and ductal arch, the aortic arch and its isthmic region, the cross-section of the superior vena cava and the trachea.
Chaoui et al.(1) consider the 3VTV an important plane for the evaluation of great vessels and upper venous system, as well as the upper-mediastinum anatomic structures. In comparison with the left and right outflow tracts, planes that are not easy to learn and are time consuming, the three-vessel view plane is as simple as the four-chamber view to obtain and as the normal three vessels are arranged in a straight line, subtle distortions of the normal anatomy can be easily recognized.
Materials and method
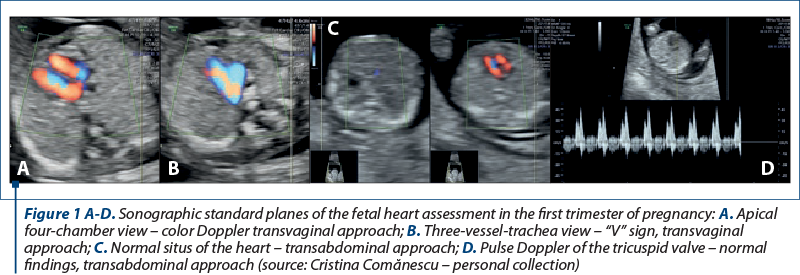
The approach to ultrasound assessment of the heart in the first trimester of pregnancy
Regarding the first trimester scan, the scanning principles of the fetal heart resemble those of the second and third trimesters of pregnancy, but color flow mapping has a definitely more important role in the first trimester.
According to the Romanian Society of Obstetrics and Gynecology (SOGR), a systematic approach should be used to assess the heartbeat, the heart position and orientation, the size of the four chambers, the tricuspid valve, and the assessment of the atrioventricular inflows and the aortopulmonary convergence (the “V/Y” sign), when the logistics allow.
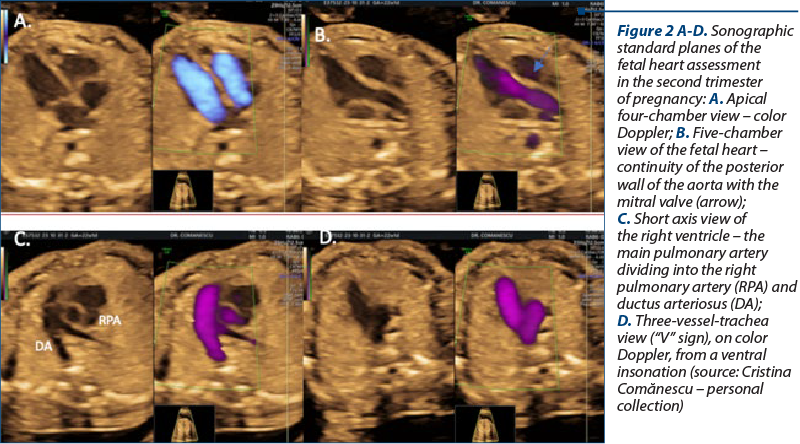
The approach to ultrasound assessment of the heart in the second trimester of pregnancy
According to international and national guidelines, fetal heart screening ultrasound should be optimally performed between 18 and 22 weeks of gestation, as earlier evaluation requires high-resolution equipment and special expertise of the sonographers. The mid-trimester scan may confirm the anomalies suspected in early pregnancy, and it may also detect new anomalies that emerge.
The fetal cardiac ultrasound examination includes the upper abdomen, the assessment of the fetal visceral situs, the fetal cardiac axis and position, the four-chamber view, the cardiac outflow tracts (the five-chamber view – LVOT, the short axis view – RVOT), the three-vessel view (“V” sign), and the three-vessel and trachea view.
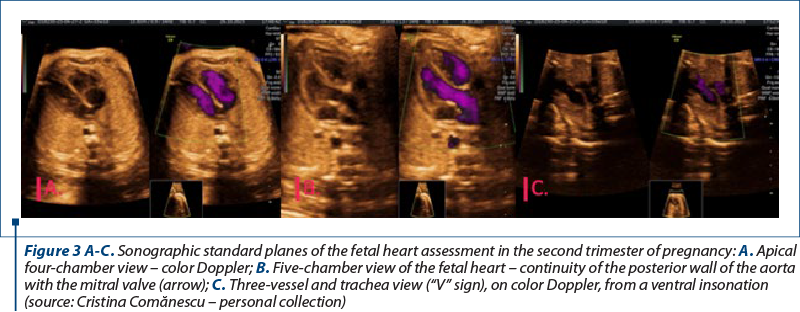
Despite its diagnostic value, the use of color flow Doppler is not considered mandatory. However, the guidelines recommend that the sonographer should become familiar with its use, as it can highlight abnormal blood flow patterns.
The approach to ultrasound assessment of the heart in the third trimester of pregnancy
The third-trimester cardiac scan is the most valuable assessment for the evaluation of the fetal heart function. Still, it may also detect anomalies that appear in late pregnancy, such as coarctation of the aorta, premature constriction of the ductus arteriosus, or hypoplastic left heart syndrome. The third-trimester scan offers a reassessment of the normal cardiac structure, and it can also detect defects that may have been missed in the first and second trimesters of pregnancy, such as aortic stenosis, ventricular septal defects, and total anomalous pulmonary venous return, or defects that develop only in the third trimester of pregnancy.
Results
We present six cases of cardiac anomalies detected in our department – Prenatal Diagnosis Unit of the County Emergency Hospital Craiova, Romania, by using standard planes of assessment, especially the three-vessel and trachea view. The malformations were detected as follows: three cases of anomalies detected in the first trimester of pregnancy – one case of right aortic arch (RAA), one case of transposition of the great arteries (TGA), and one case of hypoplastic left heart syndrome (HLHS); three cases detected in the second trimester of pregnancy – one case of TGA, one case of ARSA (aberrant right subclavian artery), and one case of RAA; and one case of coarctation of the aorta detected in the third trimester of pregnancy. In all cases, the 3VT was useful in detecting the malformations involving the ventricular outflow tracts and great arteries.
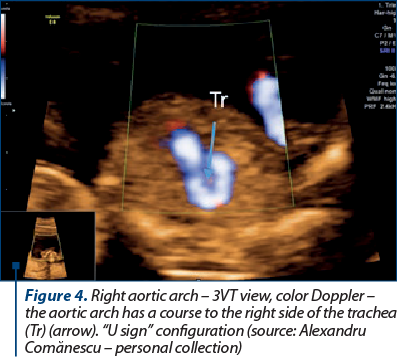
Cases detected during the first-trimester anomaly scan – 11-13+6 weeks
A right aortic arch occurs in about 1 in 1000 of the general population, and is defined by the aortic arch that crosses the right bronchus instead of the left bronchus. This anomaly is detected by ultrasound scanning when the transverse aortic arch is located to the right of the trachea on the three-vessel and trachea view. There are three cases of right aortic arch: RAA with right ductus arteriosus (right “V” sign) – the aorta and the pulmonary artery merge in a “V” configuration on the right of the trachea; RAA with left ductus arteriosus (“U” sign) – the aortic arch is right-sided and the pulmonary trunk and ductus arteriosus are to the left of the trachea, surrounding it in a “U” shaped configuration; and double aortic arch (“l” sign) – the aortic arch is coursing to the left side of the trachea but it bifurcates at the level of the trachea in one arch to the right and one arch to the right in a “lambda’’ configuration. The differentiation between the “U” sign RAA and “l” sign RAA may be difficult in the first trimester of pregnancy(1-4).
In our case, we diagnosed RAA with left ductus arteriosus by detecting an abnormal “U” shaped three-vessel view. The karyotype was normal.
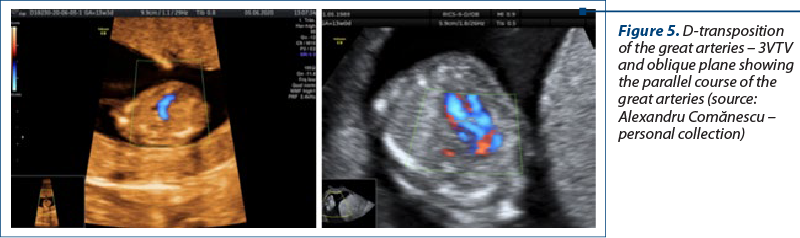
Transposition of the great arteries (TGA) is a major cardiac anomaly defined as an atrioventricular concordance with a ventriculoarterial discordance. This implies a normal connection between the two atria and the two ventricles, and a switched connection of the great arteries: the pulmonary trunk arises from the left ventricle, and the aortic arch arises from the right ventricle. The arteries array a parallel course, the aorta being placed anterior and to the right of the pulmonary artery, which explains the term D-transposition of the great arteries (D-TGA). The prenatal diagnosis of D-TGA is challenging, as the four-chamber view is typically normal in fetuses with D-TGA. The visualization of LVOT will show a vessel arising from the left ventricle that bifurcates at the base of the heart into two branches, which is the pulmonary artery. Due to the parallelism of the vessels, in most TGA cases, a transverse view in the upper thorax will show a single large vessel (the aortic arch), with superior vena cava on the right, instead of a normal three-vessel and trachea view. This anomaly can be easily missed in the first trimester of pregnancy. In this case, the abnormal three-vessel view suggested TGA malformation. The parallel course of the vessels can be demonstrated by rotating the transducer to an oblique plane of the chest. The abnormal 3VT determined us to evaluate the heart using additional oblique planes(4,5).
Hypoplastic left heart syndrome (HLHS) is a group of complex cardiac malformations characterized by an underdevelopment of the left ventricle and the left ventricular outflow tract. All the cases of HLHS have in common a severe obstruction of the aorta, with various degrees of ventricular dysfunction. Regarding the ultrasound findings, in HLHS, the four-chamber view is abnormal, with a small left ventricle, and the right ventricle forms the apex of the heart. The size of the left ventricle can vary, but in all cases there is a contractility disorder with a decreased function. In the five-chamber view, the aorta is visualized with difficulty due to its small size, and at the level of the 3VT, a compensatory dilated pulmonary trunk is detected adjoining a normal superior vena cava and an absent or hypoplastic aortic arch(1,4).
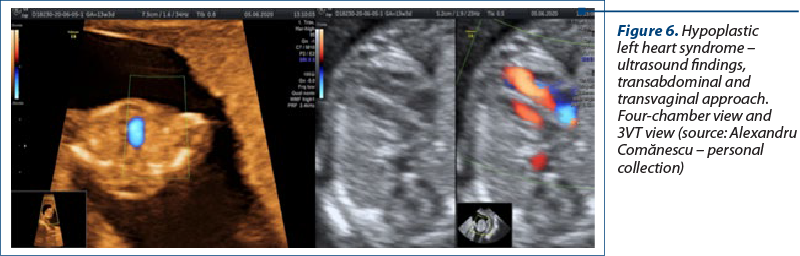

By using the color Doppler, we detected a discordance in the perfusion of heart chambers with a minimal filling of the left heart on the four-chamber view. The assessment of the LVOT failed to demonstrate forward flow across the aortic valve, and the Doppler interrogation of the three-vessel view showed an antegrade pulmonary artery flow and no flow across the narrow aortic arch.
Cases detected during the second-trimester scan – 18-22 weeks
D-transposition of the great arteries (D-TGA). The diagnosis of this case was made by using 2D ultrasound and color Doppler imaging. The anomaly was detected by using standard views according to the national guidelines and additional oblique views to demonstrate the parallel course of the vessels. In our case, the most reliable clues to diagnose this cardiac defect were a branching great artery arising from the left ventricle, as well as two vessels rather than three seen at the level of the 3VT view(5).
The detection of this kind of anomaly in the second and third trimesters can improve the outcome of these pregnancies, as the fetuses should be referred to cardiovascular centers immediately after birth. The prognosis of such neonates is excellent, provided that the child is born in a tertiary center with pediatric cardiology intensive care services.
D-TGA is usually well tolerated in utero. Further serial ultrasound evaluation should focus on the detection of an associated VSD and the subsequent development of pulmonary stenosis. The latter finding is not usually detected in the second trimester of pregnancy.
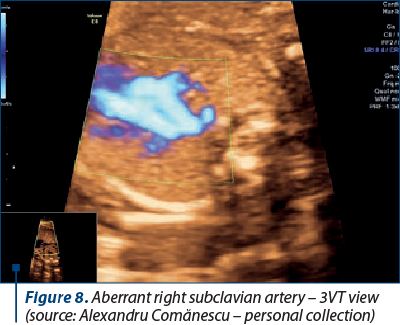
Aberrant right subclavian artery (ARSA) is diagnosed during the second trimester. ARSA is the most common anomaly of the aortic arch. In normal conditions, three vessels arise from the aortic arch: the brachiocephalic artery, the left common carotid artery, and the left subclavian artery. In this disorder, four vessels arise from the aortic arch: the right common carotid artery, the left common carotid artery, the left subclavian artery, and the ARSA.
Imaging of ARSA is typically achieved by using color Doppler techniques. The 3VT view is the most optimal plane for detecting ARSA, as it highlights the rise from the junction of the aortic arch and ductus arteriosus of a vessel coursing behind the trachea toward the right shoulder(6,7). In our case, ARSA was an isolated finding with a normal karyotype. Due to its association with genetic disorders, it is recommended to perform karyotyping.
Cases detected during the third-trimester scan
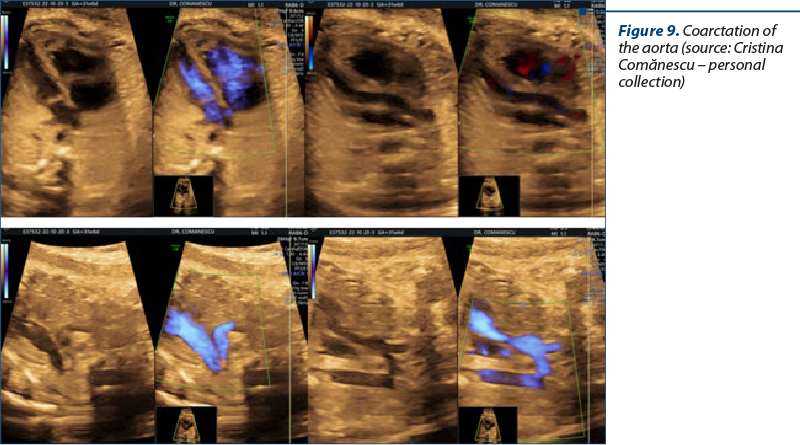
Coarctation of the aorta (CoA) is frequently detected during the third-trimester scan. The patient presented in our department for her first scan at 32 weeks of gestation.
CoA involves the narrowing of the aortic arch, typically located at the isthmic region, between the left subclavian artery emergence and the ductus arteriosus confluence. Coarctation of the aorta is one of the most difficult malformations to diagnose antenatally.
The leading sign for the suspicion of such malformation is the ventricular disproportion in the four-chamber view. The ratio of right-to-left ventricular width is greater than 1.69 in these fetuses. In normal fetuses, this ratio is about 1.19. In contrast to HLHS, in CoA the contractility of the left ventricle is normal. The evaluation of the LVOT shows the ascending aorta with a normal diameter. The 3VT view depicts a narrow aortic arch in comparison with the main pulmonary artery. This narrowing is most evident in the isthmus region. The 3VT view illustrates the great vessel disproportion, which is more specific than the ventricular disproportion alone outlined in the four-chamber view. Once the coarctation of the aorta is suspected by using standard views, additional planes, such as a longitudinal view of the aortic arch, should be assessed. The aortic arch may appear narrow and sometimes tortuous, called a contraductal shelf. The “shelf sign” is seen at the junction between the ductus arteriosus and the descending aorta. The detection of this sign makes the diagnosis of CoA most likely(6,7).
Discussion
The significance of the three-vessel view in prenatal diagnosis of fetal heart anomalies cannot be overstated. This particular perspective offers a unique insight into the intricate workings of the fetal heart, allowing for a more comprehensive evaluation of potential abnormalities. By examining the three key vessels – the aorta, the pulmonary artery, and the superior vena cava –, healthcare providers are able to assess the structural integrity and functionality of the fetal cardiovascular system with higher precision. This comprehensive approach to fetal heart evaluation is essential in ensuring early detection and appropriate management of cardiac defects, ultimately leading to improved outcomes the unborn child. The three-vessel view plays a critical role in the prenatal diagnosis of fetal heart anomalies, offering healthcare providers a detailed and nuanced perspective on the developing cardiovascular system. By incorporating this essential imaging technique into routine prenatal care, we can enhance our ability to identify and address potential cardiac issues in a timely and effective manner.
Conclusions
It is important to have a thorough evaluation of the fetal heart in all trimesters of pregnancy. Most major cardiac malformations can be detected using standard views, such as four-chamber view, LVOT, RVOT, and 3VT view. The three-vessel and trachea view is a plane that can be easily acquired in the first, second and third trimesters of pregnancy. Two-dimensional ultrasound assessment of 3VT view provides enough information to detect major conotruncal malformations. The addition of color Doppler increases the certainty of such a diagnosis.
Corresponding author:
Alexandru-Cristian Comănescu
E-mail: alexcom8000@yahoo.com
Conflict of interest: none declared.
financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.

Bibliografie
- Abuhamad A, Chaoui R. First trimester ultrasound diagnosis of fetal abnormalities, 1st Ed. Philadelphia, PA: Wolters Kluwer Heath; 2017.
- Vigneswaran TV, Jabak S, Syngelaki A, et al. Prenatal incidence of isolated right aortic arch and double aortic arch. J Matern Fetal Neonatal Med. 2021;34(18):2985-90.
- Yerlikaya G, Efetürk T, Springer S, Reischer T. Prenatal detection of right aortic arch. Arch Gynecol Obstet. 2019;299(4):933-8.
- McBrien A, Hornberger LK. Early fetal echocardiography. Birth Defects Res. 2019;111(8):370-9.
- Martins P, Castela E. Transposition of the great arteries. Orphanet J Rare Dis. 2008;3(1):27.
- Bravo-Valenzuela NJ, Peixoto AB, Araujo Júnior E. Prenatal diagnosis of congenital heart disease: A review of current knowledge. Indian Heart J. 2018;70(1):150-64.
- Chaubal NG, Chaubal J. Fetal echocardiography. Indian J Radiol Imaging. 2009;19(01):60-8.