Ovulation induction is the first line of treatment for infertility in women diagnosed with polycystic ovary syndrome and with no other cause of infertility. Clomiphene citrate is the most frequently used pharmacological agent. A prospective study was conducted to evaluate different ovulation induction agents (clomiphene citrate, letrozole, recombinant FSH) outcomes in 60 patients diagnosed with this syndrome. The study showed similar results from letrozole and clomiphene citrate in ovulation induction and pregnancy, but recombinant FSH had the best results.
Inducerea monoovulaţiei la pacientele cu sindromul ovarelor micropolichistice – rezultatele terapiilor disponibile
Mono ovulation in women with polycystic ovary syndrome - outcomes of different therapies
First published: 22 mai 2017
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.16.2.2017.763
Abstract
Rezumat
Inducerea ovulaţiei reprezintă prima linie de tratament în cazul pacientelor diagnosticate cu sindromul ovarelor polichistice şi infertilitate. Cel mai des utilizat agent este citratul de clomifen. S-a efectuat un studiu prospectiv cu scopul de a evalua diversele opţiuni de stimulare ovariană existente (citrat de clomifen, letrozol, FSH recombinat) în cazul pacientelor cu sindromul ovarelor polichistice. Conform rezultatelor obţinute, letrozolul şi citratul de clomifen au înregistrat randamente asemănătoare în inducerea ovulaţiei, cât şi în obţinerea unei sarcini, însă FSH-ul recombinat a fost cel mai eficient agent.
Introduction
Polycystic ovary syndrome (PCOS) is an important cause of anovulation infertility in women, and affects 5-12% of women of reproductive age(1,2). The incidence depends of the diagnosis criteria used, the most used criteria by gynecologists being the Rotterdam ones(3,4). This syndrome, according to Rotterdam criteria, is characterized by two or three of the following items: clinical or biochemical hyperandrogenism, anovulation and polycystic ovary morphology on ultrasound(5). The last criterium is one of the most controversial between gynecologists and endocrinologists(6). The latter consider that ultrasound criteria has low specificity and increases the prevalence(6).
The infertility management of these women can range from medical therapy (ovulation induction), surgical techniques (laparoscopy ovarian drilling) to the use of assisted reproduction techniques (ART)(2,7).
For these patients, the first recommendation is lifestyle changes(2,7,8). Because most of the patients are overweight, a 5 percent of weight loss can improve the outcome.
The first line of the treatment is the pharmacological ovulation induction. The most frequently used therapy in ovulation induction is clomiphene citrate(7,8,9). When this therapy fails, metformin and gonadotropins are used. Good results were also obtained after the use of letrozole, an aromatase inhibitor(10).
Objective
The purpose of this study was to compare the efficiency of different pharmacological agents, used for ovulation induction and to establish if the second-line drugs gave better results.
Materials and methods
A study was conducted in Columna Medical Center Bucharest to compare the results of different ovulation induction therapies in infertile patients with PCOS. The patients enrolled had no other cause of infertility except chronic anovulation.
Diagnosis of PCOS was based on the Rotterdam criteria, and all patients accused signs of anovulation and had polycystic ovary aspect on ultrasound (at least 12 follicles per ovary). A total of 60 women were included between October 2015 and October 2016. They were divided into 3 groups in the stimulation protocol used: 1 - induction with clomiphene citrate 50 mg for 5 days (days 3-7); 2 - induction with letrozole 2.5 mg for 5 days (days 3-7), 3 - induction with gonadotropins (recombinant FSH 37.5 UI for 10 days). Before allocation, all participants signed an informed written consent form.
Starting from day 10, follicular development was monitored using transvaginal ultrasound scan. All patients also underwent ultrasound scan on the second day, to exclude ovarian cysts and to evaluate the endometrial thickness. When ultrasound scan revealed a mature follicle with a diameter ≥17 mm, the patient was sent for hormonal testing (LH, progesterone and estradiol). The hCG (6500 IU) was given when LH peak was demonstrated. A LH of 30 mIU/ml was minimum needed for trigger administration.
Pregnancy was diagnosed using beta-hCG levels. An hCG level less than 25 mIU/ml was considered negative for pregnancy, and anything above 25 mIU/ml was considered positive for pregnancy. The endometrial thickness, mature follicles, ovulation and pregnancy rates were compared between the groups. The age, the body mass index (BMI), the infertility history and the years attempting to get pregnant were also recorded for all patients.
The data were analysed using Microsoft Excel™ 2016.
Results
From a total of 60 women who were enrolled into the study, 20 received clomiphene citrate, 20 received letrozole and 20 received recombinant FSH (R-FSH). The three groups had insignificant differences in their characteristics. In letrozole group, women had smaller BMI. All groups had appropriate middle ageand infertility years.
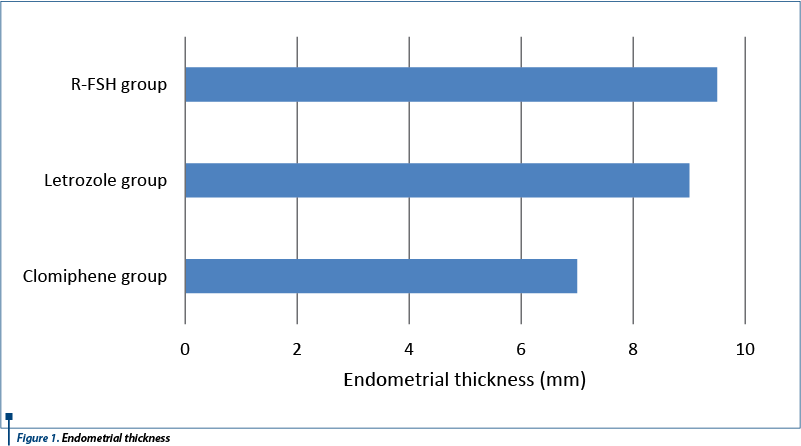
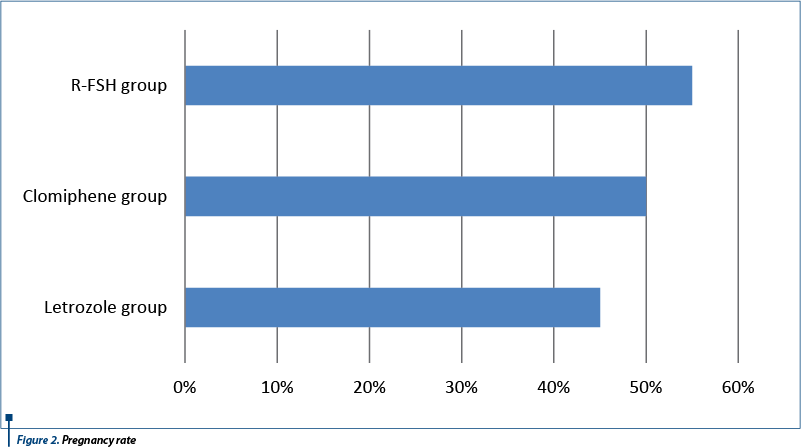
The number of follicles was lower in the letrozole group (1.2) and highest in clomiphene group (2.1). The endometrial thickness and ovulation were better in the recombinant FSH group than the other two. In the recombinant FSH group, the pregnancy rate was highest, and the lowest (9 cases) was in the letrozole group. Ten biochemical pregnancies were achieved in clomiphene group. The clinical characteristics and the results are shown in Table 1.
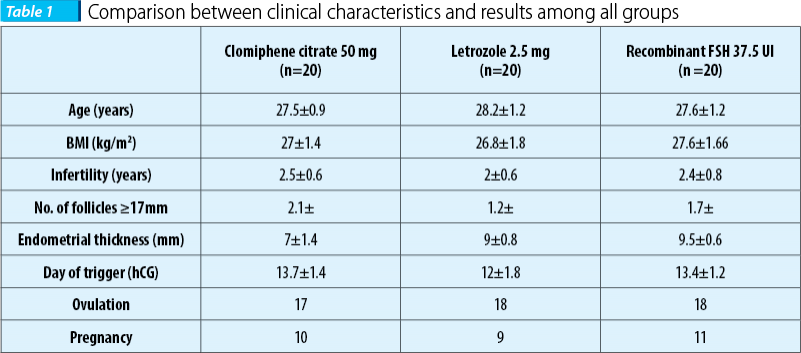
As it was expected, in the clomiphene group the endometrial thickness was thicker than in the other two groups.
In the recombinant FSH group, it was registered the greatest number of positive free-bhCG.
The ovulation rate did not differ in the rFSH and letrozole group, as it is presented in Figure 3.

Discussions
As it is well known, clomiphene citrate is the most used agent for ovulation induction in PCOS patients(5,11,12). Despite its advantages, low cost, oral administration and few side effects (flushing, headache, abdominal discomfort), clomiphene citrate has an antagonistic effect on the endometrium and reduces the endometrial thickness. Mono-ovulation is induced in most of the cases and it has a low rate of multiple pregnancies. The recombinant FSH is frequently used when resistance at clomiphene citrate appears(8). Despite the good result of recombinant FSH, the risk of hyper stimulation syndrome exists and should be taken into consideration. According to our results, the ovulation and pregnancy rate were lower for clomiphene group, when compared to R-FSH. A surprise was the higher number of follicles recruited in the clomiphene group versus R-FSH group.
Different treatment options can lead to ovulation in PCOS patients. Despite its efficiency, letrozole is still used as an “off label” ovulation agent in PCOS. Its standard recommendation in Europe is for treating breast cancer(8,10).
In a study, Atay and his collaborators compared the use of letrozole versus clomiphene citrate for ovarian stimulation and their findings suggested that letrozole was associated with a higher pregnancy rate in PCO patients than clomiphene citrate(10).
Another study, double-blind, multicenter trial, that assigned 750 patients, concluded that letrozole was associated with higher live-birth and ovulation rates among infertile women with the polycystic ovary syndrome and also with a better endometrial thickness(13). As compared to our results, we found that the ovulation rate was better for the letrozole group, but not the pregnancy rate.
In a pilot study, Batool Hossein-Rashidi and his collaborators found that recombinant FSH and clomiphene citrate had similar efficacy for the first cycle of ovulation induction in PCOS patients, according to their published results(14).
In comparison, our research results were better for recombinant FSH than for clomiphene.
Conclusions
Accordind to our results, it seems that recombinant FSH had the best results (55%) in positive-b-hCG, without significant differences in endometrial thickness in comparison with letrozole (45%).
The less positive b-hCG in clomiphene citrate can be explained by the antiestrogenic effect on the endometrium. Moreover, there was no significant difference in the ovulation and pregnancy rates between clomiphene citrate and letrozole.
The limitation of our study was the small number of patients evaluated. Although it cannot be concluded from this study that recombinant FSH usage for ovulation induction in PCOS infertile women is superior to clomiphene, its small advantage should not be neglected.
Anovulation and menstrual dysfunction represent an important aspect that affects between 6-10 percent of the PCOS patients(15).
In our opinion, an individualized treatment should be offered to PCOS patients complaining of anovulation and infertility and further studies are needed to establish which agent is better(16).
Acknowledgement: The authors report no biomedical financial interests or potential conflicts of interest
Bibliografie
2. Birch K, Gros N, Tønnes A, Petri M, Freiesleben C. Mono-ovulation in women with polycystic ovary syndrome: a clinical review on ovulation induction. Reprod Biomed Online [Internet]. 2016;32(6):563–83. Available from: http://dx.doi.org/10.1016/j.rbmo.2016.03.006
3. Jalilian A, Kiani F, Sayehmiri F, Sayehmiri K, Khodaee Z, Akbari M. Prevalence of polycystic ovary syndrome and its associated complications in Iranian women: A meta-analysis. Iran J Reprod Med. 2015;13(10):607–20.
4. Rees DA, Jenkins-Jones S, Morgan CL. Contemporary reproductive outcomes for patients with polycystic ovary syndrome: a retrospective observational study. J Clin Endocrinol Metab [Internet]. 2016; 101(April):jc20152682. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26859102%5Cnhttp://press.endocrine.org/doi/10.1210/jc.2015-2682
5. Palomba S, Falbo A, Russo T and Zullo F. Ovulation Induction in Anovulatory Patients with Polycystic Ovary Syndrome. Current Drug Therapy, 2006; 1(1):23-9.
6. Conway G, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Franks S, Gambineri A, et al. The polycystic ovary syndrome: A position statement from the European Society of Endocrinology. Eur J Endocrinol. 2014; 171(4):P1–29.
7. Melo AS. Treatment of infertility in women with polycystic ovary syndrome. Ann Endocrinol (Paris) [Internet]. 2010; 71(3):225–7. Available from: http://dx.doi.org/10.1016/j.ando.2010.03.006
8. Melo A., Ferriani R. and Navarro P. Treatment of infertility in women with polycystic ovary syndrome: approach to clinical practice. Clinics, 2015; 70(11):765-9.
9. Salem W, Javaid H, Abuzeid YM. Outcome of Assisted Reproduction in Women with Polycystic Ovarian Disease Compared to Tubal Factor Infertility: A Cohort Study. Androl Gynecol: Current Res, 2014; 02(03).
10. Atay V, Cam C, Muhcu M. Comparison of Letrozole and Clomiphene Citrate in Women with Polycystic Ovaries Undergoing Ovarian Stimulation., J Int Med Res, 2006; 34(1):73–6.
11. Tarlatzis BC, Fauser B, Thessaloniki EA-S. Consensus on infertility treatment related to polycystic ovary syndrome. Hum Reprod. 2008; 23(3):462–77.
12. Teede H, Misso M, Deeks A, Moran L, Stuckey B, Wong J, Norman R and Costello M. Assessment and management of polycystic ovary syndrome: summary of an evidence-based guideline. Med J Aust, 2011; 195(6):S65-S112.
13. Coutifaris C, Schlaff W and Casson P. Letrozole versus Clomiphene for Infertility in the Polycystic Ovary Syndrome. N Engl J Med, 2014; 371(15):1465-5.
14. Hossein-Rashidi B, Khandzad B, Shahrokh-Tehraninejad E, Sc M, Gorginzadeh M. Recombinant FSH Compared to Clomiphene Citrate as the First- Line in Ovulation Induction in Polycystic Ovary Syndrome Using Newly Designed Pens: A Randomized Controlled Trial, J Family Reprod Health, 2016; 10(1):42–8.
15. Diculescu D, Pop D, Mihu D, C. Todea, C. Iuhas, R. Nicula. Role of ultrasound evaluation of ovarian causes of infertility. Ginecologia.ro, 2015;3(9):34-9.
16. Luchian L, Bogdan Marinescu B. The outcome of the assisted reproductive technology (in vitro stimulation) in polycystic ovary syndrome phenotypes. Ginecologia.ro, 2017;5(15):8-11.
Articole din ediţiile anterioare
Cervical ectopic pregnancy – case report
The definition of an ectopic pregnancy (EP) is that of a pregnancy where implantation occurs outside the endometrial cavity. Roughly 95% of EPs tak...
The metabolic pattern for monitoring and management of gestational diabetes
Globally, the prevalence rate of overweight or obesity between 1980 and 2013 increased by 27.5% for adults and by 47.1% for children, to a total of...
Large submucous myoma in pregnancy: is caesarean myomectomy an option?
Leiomyomas are the most common benign tumors of the reproductive tract in women of childbearing age(1). The prevalence of uterine leiomyomas during...