Arteră ombilicală unică asociată cu agenezie renală fetală unilaterală – prezentare de caz
Single umbilical artery associated with unilateral fetal kidney agenesis – case report
Abstract
Single umbilical artery is the most frequent anomaly of the umbilical cord. Most of the times, the anomaly is isolated, but it can be associated with gastrointestinal anomalies (atresia or stenosis of different gastric segments), cardiac anomalies (the risk is 7 to 8 times greater than in the general population), genitourinary abnormalities and aneuploidies (trisomy 13, 18, 21). In this article, we present a resume of the knowledge regarding umbilical artery and its abnormalities, starting from a case of a female newborn who was diagnosed with single umbilical artery, right kidney agenesis and intrauterine growth restriction. The newborn associated congenital hypothyroidy which was diagnosed neonatally by metabolic screening, without any specific clinical outcome.Keywords
single umbilical arterykidney agenesiscongenital hypothyroidyRezumat
Artera ombilicală unică reprezintă cel mai des întâlnită malformaţie a cordonului ombilical. În majoritatea situaţiilor, această anomalie este izolată, dar uneori se poate asocia cu malformaţii gastrointestinale (atrezia sau stenoza anumitor segmente ale tubului digestiv), malformaţii cardiace (riscul este de 7-8 ori mai mare decât la populaţia generală), malformaţii genitourinare şi cu aneuploidii (trisomia 13, 18, 21). În continuare, vom prezenta informaţiile actuale asupra acestei malformaţii, pornind de la cazul unui nou-născut de sex feminin diagnosticat cu arteră ombilicală unică, agenezie renală stângă şi restricţie de creştere intrauterină. În urma screeningului metabolic neonatal, a fost diagnosticat şi un hipotiroidism congenital, fără a avea urmări semnificative asupra evoluţiei ulterioare a cazului.Cuvinte Cheie
arteră ombilicală unicăagenezie renalăhipotiroidism congenitalIntroduction
Single umbilical artery – general knowledge
The development of the blood vessels and fetal circulatory system starts in the fourth week of gestation. Initially, the umbilical cord contains four vessels, two arteries and two veins, after which the right umbilical vein resorbs, and in the end, the umbilical cord contains two arteries and the left umbilical vein(1).
Single umbilical artery (SUA) represents an anatomical variety in which the umbilical cord only contains one artery and one vein. It can be isolated, in about 60% to 85% of cases, or can be associated with aneuploidies and other congenital abnormalities(2).
In the embryological evolution, there are three proposed mechanisms for the existence of the single umbilical artery. The first mechanism is represented by secondary atresia or atrophy of a previous normal umbilical artery. The second mechanism is represented by primary agenesia of one of the umbilical arteries. The third mechanism represents the persistence of the allantoic artery. Approximately 40% of the umbilical cords with single umbilical artery which were analyzed using microscopy presented muscular reminiscences which supports the theory of atresia or atrophy of a previously normal umbilical artery. As a result, this theory is considered the most frequent cause of single umbilical artery. Usually, the left umbilical artery is the absent one.
There are four types of umbilical cords with single umbilical artery.
Type 1 is the most frequent (approximately 98% of cases) and is represented by an umbilical cord with two vessels, an umbilical artery of allantoic origin and an umbilical vein which is derived from the left umbilical vein; this type is associated with genitourinary abnormalities(2).
Type 2 (around 1.5% of cases) is represented by an umbilical cord with two vessels, an umbilical artery with vitelline origin detached from the superior mesenteric artery and a venous ramification from the left umbilical vein; this type is associated with severe fetal malformations, like sirenomielia and caudal regression syndrome(2).
Type 3 is rarely met, and the umbilical cord contains three umbilical vessels, an allantoic artery and two veins, detached from the left umbilical vein and from the abnormal persistence of the right umbilical vein; this type is associated with major congenital abnormalities and has a severe prognosis(2).
Type 4 is the least frequent type, being extremely rare. The umbilical cord has two vessels, a vitelline or allantoic artery and a vein detached from the right umbilical vein; this type is associated with pregnancy failure(2).
The prevalence of single umbilical artery in live newborns is around 0.3-1%. Single umbilical artery seems to be associated with extreme pregnancy age in Eastern Europe and is less frequent in Asian or African populations. There are inconstant sources which suggest that males are more likely to develop the abnormalities and are more likely to associate other malformations(3).
Single umbilical artery is more frequent in twin pregnancies (one twin with a single umbilical artery, while the other has a normal umbilical cord), with no difference between mono- or dichorionic pregnancies(4).
The risk factors that were associated with single umbilical artery are multiple pregnancies, ethnicity, smoking during pregnancy, diabetes, arterial hypertension and maternal convulsions. The presence of a single umbilical artery at the first newborn from one family doubles the recurrence risk and there is a four-time higher risk for congenital malformations for the second pregnancy(4,7,8).
Single umbilical artery is frequently diagnosed antenatally by ultrasonography and was associated with intrauterine growth restriction, premature membrane rupture, premature delivery with SGA, low placental weight, sirenomielia, genitourinary malformations (renal agenesia)(5,9), cardiovascular malformations (atrial septal defect, ventricular septal defect), gastrointestinal malformations (anal atresia, Meckel diverticulum, tracheoesophageal fistula), musculoskeletal malformations (vertebral malformations, limb malformations – VACTERL), nervous system malformations (anencephaly) and pulmonary malformations (diaphragmatic hernia, pulmonary hypoplasia)(4,7,8).
Unilateral renal agenesis and crossed renal ectopia
Unilateral renal agenesis represents the absence of one of the two kidneys. The incidence of this abnormality is approximately 1 in 1000 live newborns, the gender ratio being 1:1. Embryologically, renal agenesia can appear when the ureteral bud doesn’t differentiate the metanephric mesoderm.
Crossed renal ectopia represents the situation in which the kidney is absent on one side and it can be identified in the other side, near the other kidney which is situated normally. The most frequent case is the identification of the left kidney on the right side (approximately 85% of cases), sometimes the two kidneys being fused together at one tip, this variety being called crossed renal ectopia with fusion. The most accepted theory is the contralateral migration of the ureteral bud with the differentiation of the metanephric mesoderm with the formation of one unique renal mass, of great proportions, with two collecting ducts, on one side. The normal ascension of the kidneys, before the eighth week of gestation, is necessary for the normal development of the perirenal extraperitoneal compartment and, as a result, unilateral renal agenesis leads to connective tissues abnormalities in the respective compartment. This can lead to an exaggerated laxity of the local mesentery with further malposition of intestinal loops.
In this article, we concentrated toward the rarely encountered situation of a case with a single umbilical artery which associates unilateral renal agenesis, as well as other congenital abnormalities (congenital hypothyroidism).
Case report
The female newborn was born by a caesarean section from a single pregnancy, at a gestational age of 38 weeks, from cranial presentation, weighing 2370 g (the 5th percentile), measuring 46 cm (the 10th percentile), whit a cranial perimeter of 34 cm (the 75th percentile), BMI of 2.4 g/cm3 and an Apgar score of 9. The mother is 31 years old, at the first pregnancy, A(II) blood group, positive Rh, with the following personal pathological background: myopia, thrombophilia with mutations for MTHFR gene, VIII factor, PAI-1. The pregnancy was investigated using the double marker test and NIPT (Panorama), with normal results, negative TORCH profile, normal PAPP-A and AFP levels, first-trimester ultrasonography describing an umbilical cord with two vessels, with the absence of the left umbilical artery. At the second-trimester screening ultrasonography, the left kidney was described as a double kidney (with two collector ducts) and the right kidney was absent in the right renal lodge. At the third-trimester ultrasonography, the intrauterine growth restriction (the fetal weight was at the 5th percentile at birth) was described, as well as the aforementioned malformations.
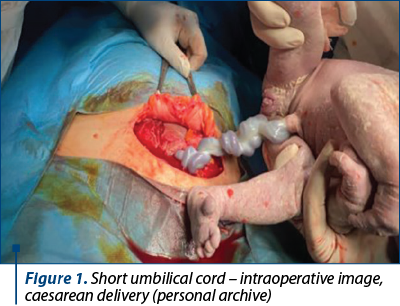
During the delivery, a short umbilical cord (40 cm) and normal amniotic fluid were identified. At the initial clinical examination, the newborn presented pink skin with acrocyanosis, spontaneous breathing, HR=120 b/min, umbilical cord with two vessels, one artery and one vein without other visible malformations. After the delivery, the newborn was hospitalized in the neonatology ward, with no ICU care required.
The abdominal ultrasonography performed at 19 days of life showed right renal agenesis and a normally situated left kidney, regulated outline, with slightly increased dimensions (61 mm/29 mm), with a parenchymatous index of 11 mm, and two separate renal pelvises and a mild swelling of the superior calyx.
At the transfontanellar ultrasonography, a bilateral periventricular hyperechoic area was identified, while at the echocardiography an atrial septal defect of approximately 2 mm was discovered, with a hemodynamically insignificant left-right shunt.
The clinical evolution was normal, with oral alimentation from the first day of life and normal digestive tolerance, with normal diuresis (2 ml/kg b.w./h), normal intestinal transit and ascending weight curve. During the stay in our maternity, the newborn developed neonatal jaundice, which required phototherapy, being discharged in the eighth day of life.
At 19 days of life, the metabolic screening results showed an increased TSH value of 176 mU/l (normal range <10 mU/l). The thyroid hormones were measured (TSH>75 mU/l, T3: 40 ng/dl and FT4<0.30 ng/dl), with an additional ultrasonography performed which showed a normal thyroid gland with two normal echogenic lobes. At the endocrinological evaluation it was recommended levothyroxine, 10 mcg/kg b.w./day. After two weeks of treatment, the thyroid hormones values normalized, with a normal clinical evolution.
Considering the right renal agenesis, further biochemical evaluations were recommended (creatinine, urea, uric acid, urinalysis) and periodic ultrasound evaluation of the left kidney, as a result of the increased risk of urinary infection and chronic kidney disease.
As a result of the association between the single umbilical artery, right renal agenesis and congenital hypothyroidy, a genetic evaluation was performed. The geneticist found no genetic syndrome and recommended WES (whole exome sequencing), a renal ultrasonography of the parents and familial planning for the next pregnancy.
The follow-up was comprised of checkups at 1 month and 2 months, the patient showing normal psychomotor development based on age and normal weight curve, which suggested a positive prognosis.

Discussion
Single umbilical artery represents the most frequent abnormality of the umbilical cord. Usually, being isolated, the newborn has a positive long-term prognosis. When congenital malformations are associated with single umbilical artery and are diagnosed intrauterinely by Doppler ultrasound, a personalized postnatal evaluation plan must be devised. In our case, the single umbilical artery was associated with a genitourinary malformation (right kidney agenesis). As a particularity of this case, the patient also associated congenital hypothyroidism which was diagnosed via extensive metabolic screening, without an obvious symptomatology.
Most often, the literature describes isolated single umbilical artery cases. The cases with associated congenital malformations are more rarely described. Our case follows the clinical pattern of missing left umbilical artery and the association with intrauterine growth restriction.
The rarity of the single umbilical artery associated with other congenital abnormalities represents the reason for the absence of a postnatal management plan. Based on the congenital abnormalities associated, the management plan should be personalized, therefore the newborn should benefit from a multidisciplinary approach, capable of correctly assessing the diagnosis and choosing the right treatment.
In our case, due to the association between the single umbilical artery and the renal malformation, additional ultrasound exams were performed to discover other possible associated abnormalities (cardiovascular, genitourinary, nervous system).
Conclusions
As we know, the literature describes frequent isolated single umbilical artery cases. In our case, the single umbilical artery was associated with renal agenesis and congenital hypothyroidism, creating a particular clinical situation, which did not fit into a specific genetic syndrome. As a result, a detailed follow-up plan was devised, including the WES examination to certify if there any genetical determinism existed or each abnormality was independent.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Sakar MN, Oğlak SC, Demir S, Gültekin H, Demi B. Isolated single umbilical artery: implications for pregnancy. East J Med. 2020;25(3):444-9.
- Rosa ET, Sepulveda W. Single umbilical artery. https://www.uptodate.com. Accessed: 18 Jan 2022.
- Ebbing C, Kessler J, Moster D, Rasmussen S. Isolated single umbilical artery and the risk of adverse perinatal outcome and third stage of labor complications: A population-based study. Acta Obstet Gynecol Scand. 2020;99(3):374–80.
- Jain A, Shankar K. Single umbilical artery. Perinatology. 2018;19(3).
- Ozcan T. Renal agenesis: prenatal diagnosis. https://www.uptodate.com. Accessed 20 Jan 2022.
- Doornebal N, de Vries TW, Bos AF, de Vries NKS. Screening infants with an isolated single umbilical artery for renal anomalies: Nonsense? Early Hum Develop. 2007;83(9):567–70.
- Prucka A, Clemens M, Craven C, McPherson E. Single umbilical artery: what does it mean for the fetus? A case-control analysis of pathologically ascertained cases. Genet Med. 2004;6(1):54 –7.
- Wiegand S, McKenna DS, Croom C, Ventolini G, Sonek JD, Neiger R. Serial sonographic growth assessment in pregnancies complicated by an isolated single umbilical artery. Am J Perinatol. 2008;25(3):149-52.
- Delmas HL, Kohler M, oray B, Lemery D, Francannet C, Quistrebert J, Marie C, et al. Congenital unilateral renal agenesis: prevalence, prenatal diagnosis, associated anomalies. Data from two birth-defect registries. Birth Defects Res. 2017;109(15):1204-11.
- LaFranchi S. Clinical features and detection of congenital hypothyroidism. https://www.uptodate.com. Accessed: 20 Jan 2022.




