Experienţa noastră în managementul gravidelor infectate cu SARS-CoV-2
Our experience in the management of pregnant women with SARS-CoV-2 infection
Abstract
The infection with SARS-CoV-2 among pregnant women represents a new challenge all over the world. Establishing an effective way to prevent the infection with the new type of coronavirus could decrease its incidence. Although this pathology is not completely understood and its perinatal complications are not entirely well known, it should be necessary to create a protocol to prevent and manage this disease. We present the experience of the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital regarding pregnant women associating SARS-CoV-2 infection.Keywords
SARS-CoV-2COVID-19pregnancyabortionRezumat
Infecţia cu SARS-CoV-2 în rândul pacientelor gravide reprezintă o nouă provocare în întreaga lume. Stabilirea unei modalităţi eficiente de a preveni infecţia cu noul tip de coronavirus poate duce la scăderea incidenţei acesteia. Deşi patologia acestei boli nu este complet înţeleasă, iar complicaţiile perinatale nu sunt pe deplin cunoscute, ar trebui creat un protocol de prevenire şi management pentru această patologie. Prezentăm experienţa Departamentului de obstetrică şi ginecologie al Spitalului Universitar de Urgenţă Bucureşti în rândul pacientelor gravide infectate cu SARS-CoV-2.Cuvinte Cheie
SARS-CoV-2COVID-19sarcinăavortIntroduction
With the debut of the COVID-19 pandemic, one of the main concerns of the medical staff was to clarify if pregnant women are vulnerable to the SARS-CoV-2 infection, due to the changes in the immunological status that they undergo during pregnancy.
The experience in dealing with SARS and MERS brought about the fear that SARS-CoV-2 could also be associated with miscarriage, intrauterine death or fetal growth restriction. Medical data gathered over the last year have shown that pregnant women infected with SARS-CoV-2 do not suffer from a more severe form of the disease than the general population, and are not at a higher risk of contracting the infection(1).
In pregnant women, the disease onset is most frequently accompanied by common symptoms as in the general population, like fever, cough, myalgia or fatigue. As far as specific biomarkers are concerned, the most often encountered are: an increase in C-reactive protein (CRP) and lymphopenia.
Preterm birth has the highest incidence concerning obstetrical complications, but there is a smaller percentage of cases regarding premature rupture of membranes, gestational diabetes, preeclampsia and gestational hypertension. As for fetal and neonatal complications, the few studies conducted during the last year revealed higher cases of lung infections and isolated cases of stillbirth and neonatal death. The data on the impact of SARS-CoV-2 infection on maternal, fetal and neonatal pregnancy complications are scarce and the studies conducted are small(2).
Obstetrical, fetal and neonatal complications are also directly related to vertical transmission. The laboratory findings regarding intrapartum viral exposure are consistent(3). The transplacental transmission of SARS-CoV-2, although possible, is rare. The virus genetic material has been discovered in several umbilical cord blood, placenta and breast milk samples. Simultaneously, anticoronavirus antibodies were identified in umbilical cord blood and milk(4). The extent and the clinical relevance of womb transmission have not been adequately researched. It is still unknown if the vertical transmission level differs depending on the moment the viral infection occurs during gestational stages.
In the context of trying to control the pandemic through vaccination, another concern is whether pregnant women can safely benefit from it. COVID-19 mRNA vaccine induces an immune response in pregnant and breastfeeding women similar to that in nonpregnant women. Even the postvaccination side effects are not significantly different. Neutralizing antibodies are present in samples of the umbilical cord and breast milk samples. However, it is still unclear if the immune transfer that occurs is relevant enough to protect the fetus or the newborn since the level of antibodies, at least in umbilical cord serum, is relatively low. It remains to be researched when it is the appropriate period during pregnancy to get vaccinated to benefit from a maximum level of protection(5).
Materials and method
We performed an observational, retrospective study on 2556 pregnant women admitted to the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital, a tertiary centre in Romania, between 1 March 2020 and 31 March 2021. We divided the pregnant women into two groups. In the first group, we enrolled pregnant patients who tested negative for SARS-CoV-2 on the real-time reverse transcription polymerase chain reaction (RT-PCR) method, while in the second group, pregnant women tested positive for SARS-CoV-2 on the RT-PCR method. Each group was split into two other groups: pregnant women under 24 weeks of pregnancy who had a spontaneous abortion and tested negative or positive for SARS-CoV-2 on RT-PCR method, and pregnant women over 24 weeks of pregnancy who gave birth and tested negative or positive for SARS-CoV-2 on RT-PCR method. The information about abortion, pregnancy and delivery outcomes was retrieved from the hospitalization sheets and the Base Data System of the Bucharest University Emergency Hospital. The informed consent for participating in this study was obtained from the legal guardian of patients aged less than 18 years old or for the patient for the adolescents aged ≥18 years old.
The infection with SARS-CoV-2 was defined as the positive result on RT-PCR conducted in our hospital. We tested all patients who needed hospitalization for SARS-CoV-2. The gestational age was calculated based on the time of the last menstrual period. Abortions were considered the product expulsions before 24 weeks of pregnancy, while deliveries were defined after completing 24 weeks of pregnancy. Deliveries before 37 weeks of gestation were counted as preterm births.
We evaluated and compared the rate of positive patients for SARS-CoV-2 in each group and the obstetrical complications. The statistical analysis was performed using Microsoft Excel and SPSS 9.5.
Results
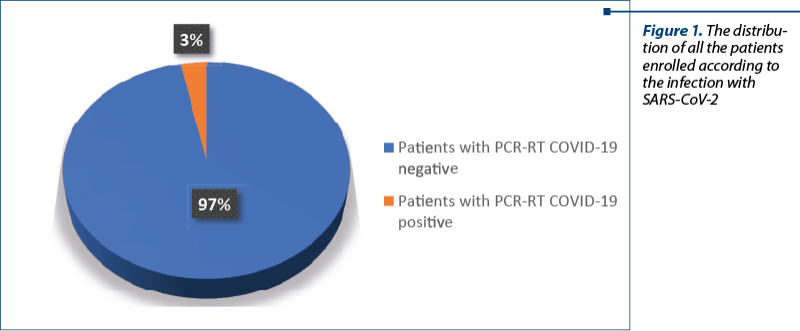
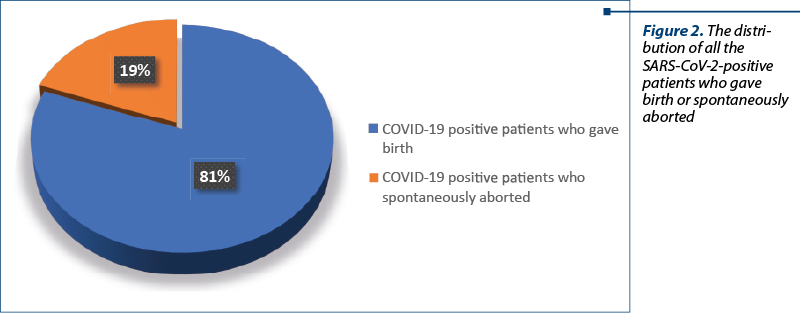
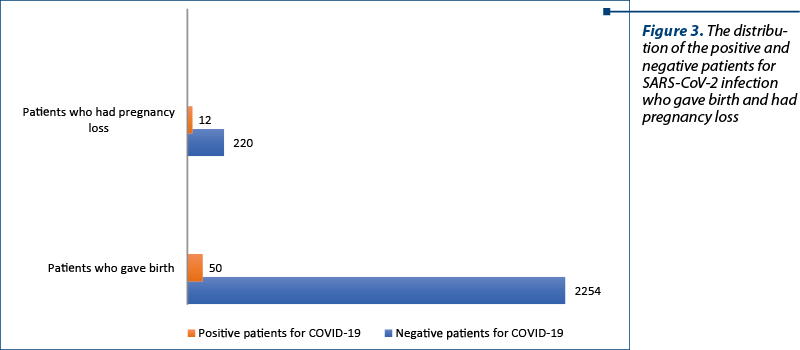
In group I there were enrolled 2474 patients, while in group II there were enrolled 82 patients (Figure 1). In group I, there were 220 patients who lost a pregnancy and 2254 patients who gave birth. Both subgroups tested negative for SARS-CoV-2. In group II, there were 12 patients who lost the pregnancy and 50 patients who delivered; the patients from both subgroups tested positive for SARS-CoV-2 (Figure 2).
We mention that there were four pregnant women under 24 weeks hospitalized for threatened miscarriage associated with COVID-19. Also, 16 patients with pregnancy over 24 weeks with false labour associated a positive RT-PCR test for SARS-CoV-2.
Most of the patients enrolled in group II did not have any symptoms of SARS-CoV-2 infection (n=75). One patient enrolled in the study was admitted to the intensive care unit. She was a 35-year-old patient, pregnant in 23 weeks, who had an RT-PCR SARS-CoV-2 positive test, and after five days of hospitalization the fetus stopped from evolution, and she had a spontaneous abortion.
We observed that 2.17% (n=50) of all deliveries (n=2304) were patients with a positive test for SARS-CoV-2, while from all spontaneous abortions (n=232), 5.17% were patients with a SARS-CoV-2 positive test (Figure 3). The extracted fragments were sent to the anatomopathological department for further examinations, from all the patients who had a spontaneous abortion. We mention that, from all 12 patients with coronavirus disease, 10 had a specific change at the anatompathologic examination: multiple hemorrhagic sites (Figure 4 and Figure 5).
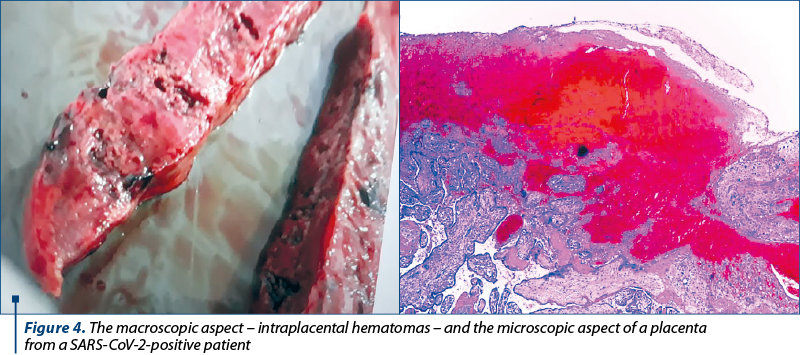

It is important to mention that one patient who tested positive had an antepartum dead fetus. In contrast, in the group of negative patients for SARS-CoV-2, 19 patients had an antepartum dead fetus, examined by the anatomopathological department that observed an abnormal hemorrhagic number of modifications in the placenta.
We analyzed the delivery method (vaginal delivery or caesarean extraction) in pregnant women who completed 24 weeks of pregnancy and were infected with SARS-COV-2, and the one who had not associated this pathology. In patients with coronavirus infection, there were 66% deliveries by caesarean section, while in the other group there were 72.8% indications for this type of delivery.
We also studied the indications for caesarean extraction and the preterm term deliveries in the group of patients with COVID-19. The most frequent indication was uterine scare after a caesarean extraction, representing 45.45% (n=15) of all indications. The indications for caesarean extraction, in the order of frequency, were: fetal distress (n=7), preeclampsia (n=6), and placenta praevia (n=2). Caesarean extraction indications were represented by: gestational diabetes, cervical dystocia, and frontal and parietal venous thrombosis (n=1). Preterm deliveries were observed in 18% of all deliveries in patients infected with SARS-CoV-2, and 66.66% of them delivered by caesarean section.
In the group of negative patients for SARS-CoV-2, compared to the positive group, the frequency of indications for caesarean section were: uterine scar (43.02%), preeclampsia (6.09%), fetal distress (4.57%).
None of the patients enrolled in the study had an anti-COVID-19 vaccine.
Discussion
The infection with SARS-CoV-2 is still new, spreading very fast, all over the world. There have not been many studies regarding the pregnancy and this pathology due to the short time it has appeared and because its physiopathology is not completely known.
Although in other studies the incidence of SARS-CoV-2 was higher, we had only 3% of pregnant women associating this infection in our study. The explanation may be related to the fact that our hospital was not a unit dedicated only to patients infected with SARS-CoV-2. Still, we have also been treating patients negative for coronavirus.
According to the rate of abortion, it seems that the coronavirus disease is not an independent predictor for abortion(6). In the studies that were performed, the early pregnancy loss rate varied between 1.2% and 2.2%(6,7). It is essential to mention that in our study the percentage was higher (5.17%) than the mean rate evaluated in other studies. The explanation may be linked to the fact that our patients never undergo a medical examination before. In other studies, spontaneous abortion was caused by the aggressive symptoms of COVID-19, and they have not found any link between asymptomatic patients and loss of pregnancy(8). In our study, only one patient had significant symptoms and was admitted to intensive care unit, having a spontaneous abortion, while the other patients had no symptomatology.
The histopathological changes of placentas analyzed in our study revealed more hemorrhagic modifications in patients with coronavirus disease than in placentas from non-COVID-19 patients. Recent research that also analyzed the placentas from positive COVID-19 patients observed a high number of villitis of unknown etiology(9). We did not observe this modification.
Regarding the delivery method, emergency caesarean section had a higher incidence in both groups. In the subgroup of patients positive for COVID-19 who gave birth, the most frequent indications for caesarean extraction were uterine scar, fetal distress and preeclampsia. In other studies, fetal distress, premature rupture of the membrane and stillbirth were the most common indications for caesarean section(10). It is supposed that these obstetrical and perinatal complications may be associated with the coronavirus infection and can occur due to the physiologic changes that reduce the women’s intolerance to hypoxia during late pregnancy(10,11). In our study, the uterine scar after other caesarean section was the most common indication in both studies. The explanation may be that this type of delivery has been liberalized in the last years.
Preterm deliveries were observed in 18% of all positive patients for SARS-CoV-2 who gave birth. In other studies, the preterm delivery rate oscillated between 16.9% and 26.3%(7,12). This is an important alarm sign, because physicians in obstetrics and gynecology should pay more attention to pregnant women with COVID-19.
Conclusions
The infection with SARS-CoV-2 still represents a challenge for all doctors. It is important to detect this infection in pregnant women, even in early pregnancy, because we can prevent abortion, preterm delivery, or other obstetrical or neonatal complications.
We need to improve the prevention of coronavirus disease 2019. Also, we should promote vaccination in the population in order to stop the virus from spreading, and prevent its perinatal complications.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Wang CL. Impact of COVID-19 on pregnancy. Int J Med Sci.2021;18(3):763-7.
-
Makvandi S, et al. The 2019 novel Coronavirus disease in pregnancy: a systematic review. Adv Exp Med Biol. 2021;1321:299-307.
-
Penfield CA, Lighter J, Roman AS. Intrauterine vertical transmissibility of SARS-CoV-2: the evidence is evolving. Am J Obstet Gynecol MFM. 2020;2(4):100227.
-
Fenizia C, et al. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat commun. 2020;11(1):5128.
-
Gray KJ, et al. COVID-19 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol. 2021;2021.03.07.21253094.
-
Cosma S, et al. Coronavirus disease 2019 and first-trimester spontaneous abortion: a case-control study of 225 pregnant patients. Am J Obstet Gynecol. 2021;224(4):391e1-391e7.
-
WAPM (World Association of Perinatal Medicine) Working Group on COVID‐19. Maternal and perinatal outcomes of pregnant women with SARS‐CoV‐2 infection. Ultrasound Obstet Gynecol. 2021;57(2):232-41.
-
Patberg ET, Adams T, Rekawek P, Vahanian SA, Akerman M, Hernandez A, Rapkiewicz AV, Ragolia L, Sicuranza G, Chavez MR, Vintzileos AM, Khullar P. Coronavirus disease 2019 infection and placental histopathology in women delivering at term. Am J Obstet Gynecol. 2021;224(4):382.e1-382.e18.
-
Patberg ET, Adams T, Rekawek P, Vahanian SA, Akerman M, Hernandez A, Rapkiewicz AV, Ragolia L, Sicuranza G, Chavez MR, Vintzileos AM, Khullar P. Coronavirus disease 2019 infection and placental histopathology in women delivering at term. Am J Obstet Gynecol. 2021;224(4):382.e1-382.e18.
-
Liu Y, et al. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J Infect. 2020 Mar 5 [Epub ahead of print].
-
Al-Tawfiq JA, Rana F. Kattan RF, Memish ZA. Middle East respiratory syndrome coronavirus disease is rare in children: an update from Saudi Arabia. World J Clin Pediatr. 2016;5(4):391-6.
-
Crovetto F, et al. Impact of SARS-CoV-2 infection on pregnancy outcomes: a population-based study. Clin Infect Dis. 2021 Feb 8;ciab104.





