Impactul psihoemoţional al sarcinii ectopice – experienţa clinicii noastre
The psychoemotional impact of ectopic pregnancy – the experience of our clinic
Abstract
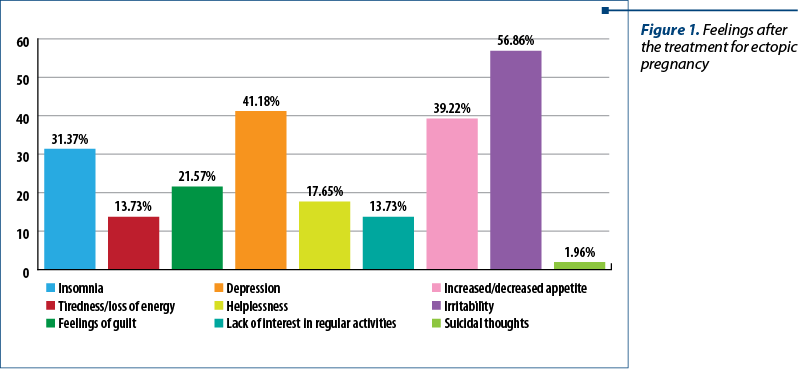
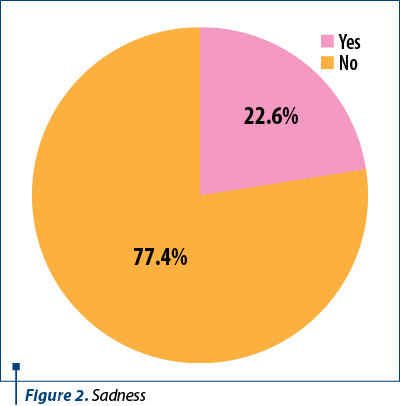
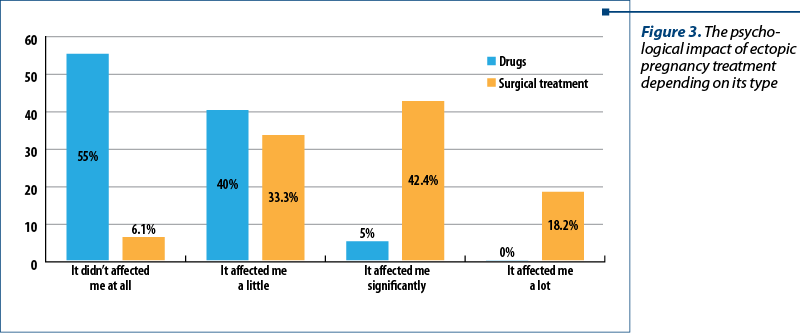
Introduction. Women with ectopic pregnancy experience feelings of sadness, depression and guilt. This study aimed to identify and evaluate the psychoemotional impact on women who were diagnosed with ectopic pregnancy and need psychological counselling after such an experience. Materials and method. We studied 53 eligible women who were diagnosed with ectopic pregnancy and treated at the Bucur Maternity, Bucharest. The patients completed a questionnaire with 28 questions. Results. The maximum incidence of ectopic pregnancy was between 26 and 30 years old. Regarding emotional disturbance, most patients (56.8%) experienced irritability, 41.1% had depression, 31.3% mentioned insomnia, and 21.5% felt guilty. The results showed that the highest incidence of depression was in patients who already had a child (52.4%). The patients were asked about their feelings when they were diagnosed with ectopic pregnancy, and most of them (77.4%) felt sad. Drug treatment had an impact on half of the interviewed women (55%). We tried to find if the patients needed or searched a psychological counselling session. The results indicated that 81.1% of them didn’t see a psychologist. Conclusions. According to our study, patients were psychoemotionally affected by the ectopic pregnancy. Most of them did not seek help from a psychologist.Keywords
ectopic pregnancypsychological issuesemotional disturbancepsychological counsellingRezumat
Introducere. Studiul de faţă a avut drept scop identificarea şi evaluarea impactului psihoemoţional al femeilor care au fost diagnosticate cu sarcină ectopică, dar şi nevoia de consiliere psihologică după această experienţă. Materiale şi metodă. Am analizat 53 de paciente care au fost diagnosticate şi tratate pentru sarcină ectopică la Maternitatea Bucur, Bucureşti. Pacientele au completat un chestionar alcătuit din 28 de întrebări. Rezultate. Incidenţa maximă a sarcinii ectopice a fost înregistrată la grupa de vârstă 26-30 de ani. În ceea ce priveşte impactul emoţional, majoritatea pacientelor (56,8%) au spus că au avut stări de nervozitate, 41,1% au avut stări depresive, 31,1% au avut insomnii, iar 21,3% sentimente de vinovăţie. De asemenea, rezultatele au arătat că incidenţa cea mai mare a depresiei a fost la grupul pacientelor care aveau deja un copil, respectiv 52,4%. Pacientele au fost întrebate despre sentimentele pe care le-au avut la aflarea diagnosticului şi majoritatea lor (77,4%) au răspuns că au fost triste. Tratamentul medicamentos a avut un impact psihoemoţional la aproximativ jumătate din ele (55%). Am încercat să aflăm dacă pacientele au avut nevoie sau au căutat ajutorul unui psiholog, iar rezultatele au arătat că 81,1% nu au apelat la şedinţe de consiliere psihologică. Concluzii. Conform studiului nostru, pacientele cu sarcină ectopică au fost afectate psihoemoţional de acest diagnostic. Majoritatea nu au încercat să apeleze la ajutorul unui psiholog.Cuvinte Cheie
sarcină ectopicăafectare psihologicătulburări emoţionaleconsiliere psihologicăIntroduction
Pregnancy and childbirth are sensitive periods in women, but also in a couple’s life. It implies a lot of physiological, emotional and behavioural changes and adaptations mainly from the woman’s point of view. Whenever the process is successfully ending with a healthy mother and child, the impact – mainly the psychological one – is positive, giving the sense of fulfilment. But in some cases, the pregnancy is lost from different reasons, including an ectopic pregnancy situation that can also trigger negative changes of the psychoemotional well-being of the women(1,2).
Besides the emotional impact of the pregnancy loss, there is also the legitimate worry about the mother health, life and fertility outcome. In most ectopic pregnancies, the right medical decision is mandatory to remove the pregnancy because the mother’s life could be in danger. At that moment, the ethical and emotional part of the medical profession faces difficult decision based on the risks/benefits approach(3).
Several studies have shown that women who had a miscarriage for whatever reason, or an ectopic pregnancy, are prone to feelings of sadness, depression and guilt. Depression is associated with the loss of a desired pregnancy, the worry for the future pregnancy and for the mother’s health(4).
This study aimed to identify and evaluate the psychoemotional impact on women who lost a pregnancy due to ectopic implantation behaviour, and the need for psychological counselling after such an experience. Those women were often overlooked whenever such issues occurred and their loss and grief were not properly addressed in our culture.
Materials and method
We conducted a prospective cohort study in 2020 at the Bucur Maternity, Bucharest. A group of patients diagnosed in our unit with ectopic pregnancy, between January 2015 and February 2020, was analyzed.
The inclusion criteria were: confirmed ectopic pregnancy, biochemical, by ultrasound or clinical, irrespective of the treatment mode, willing to answer the questions, and over 18 years old.
The exclusion criteria were: minor patients, suspected ectopic pregnancies without case outcome, patients who denied participation in the study.
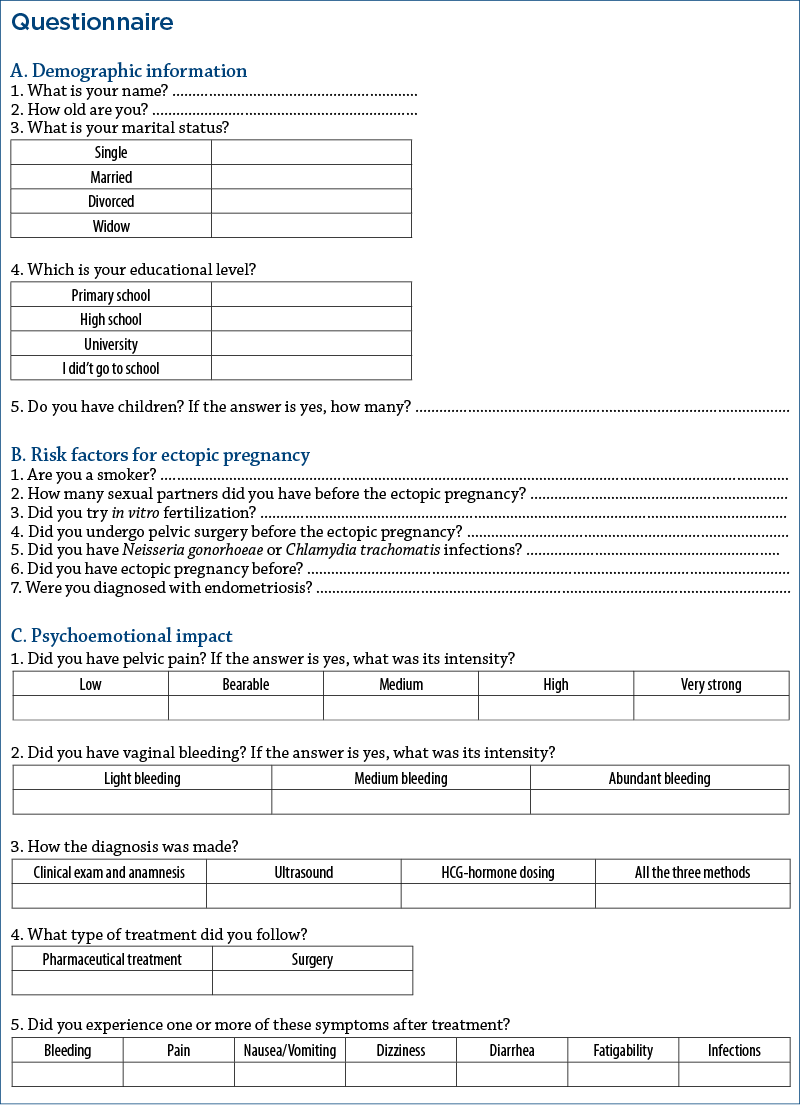
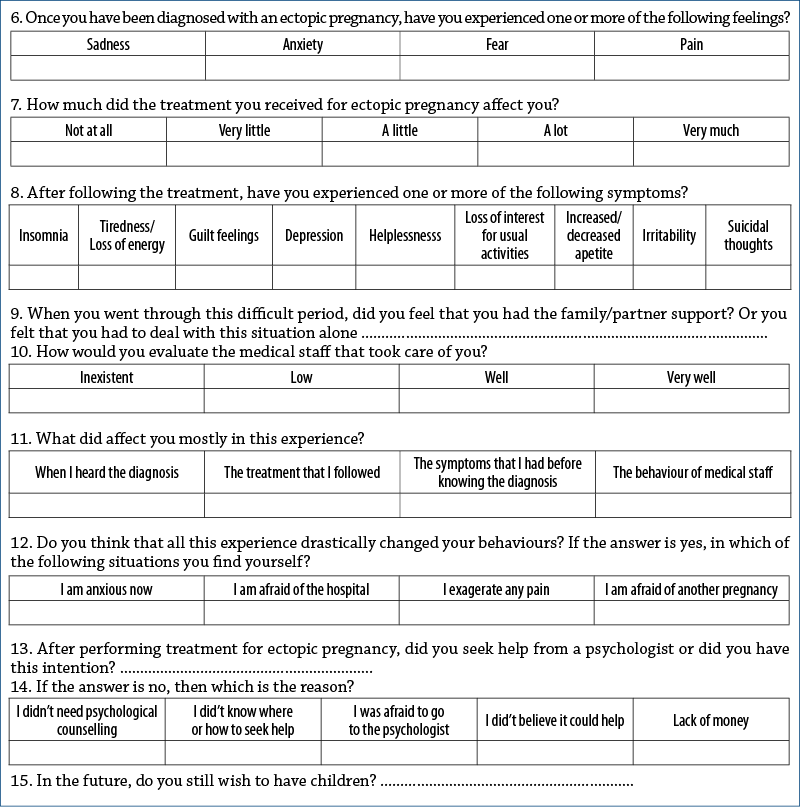
The patients who met the inclusion criteria of the study were contacted by phone. Out of a total of 101 patients, 53 were eligible and wanted to answer to our queries. We applied a questionnaire consisting of 27 questions divided into three sections.
The first part consisted in general demographic information from which we collected age, number of children, marital status and education level.
The second part consisted of questions related to risk factors for ectopic pregnancies, such as smoking, genital infections, pelvic surgeries, endometriosis, ectopic pregnancy history etc.
The third part included questions about the women’s mental health, emotions before and after they lost the pregnancy, and the need for a psychologist, for issues such as insomnia, feelings of guilt, depression, irritability, suicidal thoughts, sadness, the need for psychological counselling etc.
The study was aproved by the Ethical Comitee of the hospital.
The database, the statistical analysis of collected information, and the graphs were elaborated by using IBM SPSS Statistics version 25.0.
Results
A number of 53 patients diagnosed with ectopic pregnancy could be contacted by phone and agreed to answer our questionnaire. Concerning the issues related to marital status, 67.9% of the patients were married, 20.7% were divorced, and the percentage of unmarried was 11.3%.
Regarding their educational level, 15% of women graduated the primary school, 28.3% graduated the high school, and 56.7% had higher education.
The distribution by age groups showed that the maximum incidence of ectopic pregnancy belongs to the age range of 26-30 years old, while the lowest incidence is found in the age range of 41-45 years old. Regarding the number of children, 56.6% of women with ectopic pregnancy had already a child.
Furthermore, we analyzed the risk factors using the questionnaire. We found out that most of them were smokers (64.1%), that 20.7% of women had been diagnosed with genital infections such as Neisseria gonorrhoeae or Chlamydia trachomatis, that 7.5% of them had been diagnosed with endometriosis, and that 30.1% had pelvic surgery before ectopic pregnancy.
Regarding the emotional disturbance, Figure 1 illustrates the women’s feelings after the treatment for ectopic pregnancy. Most of the patients (56.8%) experienced irritability, 41.1% had depression, 31.3% mentioned insomnia, and 21.5% had feelings of guilt. On the other hand, a very small percentage (1.9%) had suicidal thoughts after this event.
We compared the incidence of depression after ectopic pregnancy treatment in patients with or without children. The results showed that the highest incidence of depression was found in patients who already had a child, respectively 52.4% of them answered that they had depressive states after pregnancy loss due to ectopic pregnancy because they wanted a second offspring. It also seems that those who had three or more children got over the episode more easily.
The patients were asked about their feelings when they were diagnosed with ectopic pregnancy. Figure 2 shows that most of them (77.4%) felt sad. Other feelings described by women were anxiety (49.1%), emotional pain (49.6%) and fear (56.6%). Given all these, it seems that a psychoemotional impact appeared since they found out about the diagnosis.
In the study, we also analyzed the psychoemotional impact in correlation with the treatment method (Figure 3). The statistical analysis of the answers given by patients showed that drug treatment had little impact on the psychoemotional status (55% of the patients). On the other hand, patients who underwent surgery appreciated that the treatment for removal of the ectopic pregnancy had affected them a lot from a psychological point of view (42.1% of them).
We tried to find out if the patients needed or looked for psychological counselling. The results indicated that 81.1% of them didn’t see a psychologist, although they answered at previous questions that they were emotionally affected by ectopic pregnancy. Only 11.3% of them sollicited a specialised psychological support. The underlying reason for not searching specialised pshychological support differed, thus 70.2% of the patients considered it unnecessary and 12.7% had no financial possibilities. Moreover, 86.8% answered that they relied on family support, so they did not need a psychologist.
At the end of the questionnaire, we analyzed if patients desire a new pregnancy in the future, and 32 out of 53 patients said that they plan having a new pregnancy in the future, while 21 of them said they didn’t want children anymore after the ectopic pregnancy experience.
Discussion
In our study, the most expressed feelings associated with ectopic pregnancy were emotional pain, anxiety, depression and fear. Among the feelings experienced by women after ectopic pregnancy treatment, practically after they have lost the desired pregnancy, there are depression, feelings of guilt and insomnia. All these states could be associated with psychological trauma of the women surveyed. It means that ectopic pregnancy leaves not only a physical imprint, but also an emotional one that should not be missed(5). Several studies have shown the same thing: women who have gone through a miscarriage, including an ectopic pregnancy, are prone to feelings of sadness, depression or guilt(6).
A prospective study published in 2016 and led by Farren et al. in London, on a group of 186 women, showed that most of them who had an ectopic pregnancy or abortion had specific symptoms for PTSD (post-traumatic stress disorder – a psychological response developed following a thread of death or injury). In the context of ectopic pregnancy, patients experience psychological trauma due to the subjective perception of the need for induced abortion, also due to bleeding or if they see foetal tissue.
The same study showed that women with ectopic pregnancy experienced associated symptoms with the psychoemotional impact, such as high levels of emotional stress, anxiety and depression, as evidenced by the present study(7). The same feelings were described by the women in the group that we analyzed.
Another study led by Lok et al., presented in 2004, also highlighted the psychological impact of losing a pregnancy. An important point of the study was that the age ranges most affected by depression after the removal of ectopic pregnancy were 26-30 years old and 36-40 years old(8). Our data are concordant with this paper, and we also found that the maximum incidence of ectopic pregnancy belongs to the same age range (26-30 years old).
Based on studies, post-traumatic stress is associated with pain and anxiety in the context of physical injuries. Symptoms such as nightmares, insomnia, inhibition of feelings, anxiety, irritability, concentration problems occur as a result of obstetric complications or miscarriage(9,10). We demonstrated in our study that 31.3% of patients had insomnia, and 56.8% of them had states of irritability.
The present study reveals that surgery amplifies the psychological trauma, in addition to the emotional shock suffered by patients when hearing the bad news that the desired pregnancy was no longer viable. Opposite study results were published in 1996 when Nieuwker et al. analyzed the impact of treatment performed for ectopic pregnancy in terms of patient’s quality of life. A questionnaire measuring the patient’s quality of life after drug treatment with methotrexate or laparoscopic procedure was used to collect data. The study demonstrated that patients treated with methotrexate were more affected by the treatment than those who underwent laparoscopic salpingectomy, as evidenced by the fact that these patients experienced symptoms more frequently after taking methotrexate and had more depressive symptoms(11).
Regarding psychological counselling, a study conducted in Denmark on a group of 1813 patients showed that 8.6% of women experienced severe depression after losing their desired pregnancy, and 42.1% had a high stress level. The care of these patients involved frequent ultrasounds investigations during subsequent pregnancies, mental stress assessment, and psychological counselling(12). Most of the patients enrolled in our study (81.1%) reported that they did not go to a psychologist, even though they felt emotionally affected by the experience with ectopic pregnancy.
The impact of the pregnancy loss, including an ectopic pregnancy, is determined by a lot of factors, among which education, age, cultural and social determinants, religion and marital status can be listed. Unfortunately, in our society the burden of such events is often overlooked from the psychological point of view and we do not dispose of sufficient studies in Romania that address such issues.
After an ectopic pregnancy, several factors can influence the future pregnancies and the patient’s fertility, which could decrease considerably due to injuries to the uterine tubes. Studies showed that women wearing intrauterine devices at the time of ectopic pregnancy have a better prognosis in terms of fertility after treatment(13). Because ectopic pregnancy affects fertility, more and more couples who want a baby choose in vitro fertilization, but even this method could fail due to the emotional stress that pregnant women go through. The stress generated by the ectopic pregnancy and the complexity of the in vitro treatment lead to complications for the new pregnancy and even to its loss. Also, stress before a new conception could increase infertility. Unfortunately, many women affected by ectopic pregnancy, with psychoemotional problems (anxiety, depression, post-traumatic stress disorders) and infertility, do not receive psychological counselling prior to assisted reproductive procedures(14).
Our study limitations consist in the small number of patients recruited and in the non-standardized questionnaire applied. We aimed to raise awareness for the healthcare providers to take into consideration those aspects at the level of medical services and to develop networks and guidelines for emotional and psychological support.
Screening for psychological risk is important for all women who lose a pregnancy, including those who are going through an ectopic pregnancy. The screening could be done by using various questionnaires applied to patients for psychological and emotional impact, scales and scores for depression, anxiety and other negative emotions that appeared after the loss of pregnancy(15).
Conclusions
Currently, there are few studies on the psychoemotional impact of ectopic pregnancy, most of them regarding the psychoemotional impact of losing a pregnancy, but they are not specific for ectopic pregnancy. In this study, the majority of the patients developed states of irritability. Depression also had a high share, as well as insomnia. Regarding the feelings at the time of diagnosis, the patients felt sadness, anxiety and emotional pain because they wanted that pregnancy. Most patients did not seek help from a psychologist, the main reason being that they did not consider it necessary.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Janssen HJ, Cuisinier MC, Hoogduin KA, et al. Controlled prospective study on the mental health of women following pregnancy loss. Am J Psychiatry. 1996;153(2):226–30.
- Swanson KM, Chen HT, Graham JC, et al. Resolution of depressionand grief during the first year after miscarriage: a randomized controlled clinical trial of couples-focused interventions. J Womens Health. 2009;18(8):1245–57.
- Lauzon P, Roger-Achim D, Achim A, Boyer R. Emotional distress among couples involved in first trimester abortions. Can Fam Physician. 2000;46:2033-40.
- Major B, Cozzarelli C, Cooper ML, Zubek J, Richards C, Wilhite M, Gramzow RH. Psychological responses of women after first-trimester abortion. Arch Gen Psychiatry. 2000;57(8):777-84.
- Toffol E, Koponen P, Partonen T. Miscarriage and mental health: results of two population-based studies. Psychiatry Res. 2013;205(1-2):151–8.
- Bradshaw Z, Slade P. The effects of induced abortion on emotional experiences and relationships: a critical review of the literature. Clin Psychol Rev. 2003;23(7):929-58.
- Farren J, Jalmbrant M, Ameye L, Joash K, et al. Post-traumatic stress, anxiety and depression following miscarriage or ectopic pregnancy: a prospecive cohort study. BMJ Open. 2016;6:e011864.
- Lok IH, Yip AS, et. al. A 1-year longitudinal study of psychological morbidity after miscarriage, Fertility and Sterility. 2010;93(6):1966-75.
- Engelhard IM, van den Hout MA, Arntz A. Posttraumatic stress disorder after pregnancy loss. Gen Hosp Psychiatry. 2001;23(2):62-6.
- Lisonkova S, Tan J,Wen Q, Abdellatif L, Richter LL, Alfaraj S, et al. Temporal trends in severe morbidity and mortalityassociated with ectopic pregnancy requiring hospitalization in Washington State, USA: a population-based study. BMJ Open. 2019;9(2):e024353.
- Nieuwkerk PT, Hajenius PJ, Ankum WM, et al. Systemic Methotrexate therapy versus laparoscopic salpingectomy in patient with tubal pregnancy. Impact on patients health-related quality of life. Fertility and Sterility. 1998;70(3):P518-522.
- Kolte AM, Olsen LR, Mikkelsen EM, Christiansen OB, Nielsen HS. Depression and emotional stress is highly prevalent among women with recurrent pregnancy loss. Hum Reprod. 2015;30(4):777-82.
- Bernoux A, Job-Spira N, Germain E, Coste J, Bouyer J. Fertility outcome after ectopic pregnancy and use of an intrauterine device at the time of the index ectopic pregnancy. Hum. Reprod. 2000;15(5):1173-7.
- Pasch LA, Holley, SR, Bleil ME, Shehab D, Katz PP, Adler NE. Addresing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services. Fertil Steril. 2016;106(1):209-15.
- Rapaport MH, Clary C, Fayyad R, et al. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–8.



