Incidenţa crescută a prematurităţii şi restricţiei de creştere intrauterină la gravidele cu vârstă înaintată
Prematurity and IUGR in advanced maternal age
Abstract
There are controversial findings regarding the association between prematurity and intrauterine growth restriction (IUGR) in advanced maternal age. We aspire to find a link between prematurity and intrauterine growth restriction and pregnancies with advanced maternal age, therefore we performed a retrospective study in our clinic in order to show the causality between the above mentioned. The patients selected for this study cohort, using their medical health information, were women over 35 years of age who delivered in our hospital. The possible maternal complications in pregnancy over 35 years old include increased risk of preterm labor, preeclampsia, gestational diabetes mellitus, stillbirth, chromosomal abnormalities, spontaneous miscarriage and caesarean delivery. The possible adverse fetal outcomes include intrauterine growth restriction, low birth weight, low Apgar score at birth or admission to neonatal intensive care units. We looked after prematurity and IUGR, but we also compared the conceiving way and the delivery method.Keywords
prematurityintrauterine growth restrictionadvanced maternal agechildbearing agelow birth weightpremature birthRezumat
Există informaţii controversate cu privire la asocierea dintre prematuritate şi restricţia de creştere intrauterină (RCIU) în sarcina de vârstă avansată a mamei. Obiectivul este de a găsi o legătură între aceste complicaţii în sarcina de vârstă maternă avansată, printr-un studiu retrospectiv, folosind baza noastră de date clinice, pentru a releva cauzalitatea dintre factorii menţionaţi anterior. Pacientele selectate pentru cohorta de studiu prin utilizarea informaţiilor lor medicale de sănătate sunt femei cu vârsta de peste 35 de ani care au născut în spitalul nostru. Posibilele complicaţii materne în sarcina cu vârsta de peste 35 de ani includ riscul crescut de travaliu prematur, preeclampsia, diabetul gestaţional, naşterea cu făt mort, anomaliile cromozomiale, avortul spontan şi naşterea prin cezariană. Posibilele rezultate adverse fetale includ restricţia de creştere intrauterină, greutatea scăzută la naştere, scorul Apgar mic la naştere şi internarea în unităţile de terapie intensivă neonatală. În acest grup de paciente, au fost studiate prematuritatea şi RCIU, împreună cu metoda de concepere şi naştere.Cuvinte Cheie
prematuritaterestricţie de creştere intrauterinăvârstă maternă avansatăvârstă fertilăgreutate mică la naşterenaştere prematurăIntroduction
Women are having their first children at older ages, a global trend called delayed childbearing. Pregnancies over 35 years old can be classified in the advanced maternal age category(1). In the last decades, the rate of pregnancies at an advanced maternal age (AMA) has increased steadily(2), more and more women delaying childbearing and having fewer babies. This movement of advanced maternal age can be related to social and demographics reasons(2).
The development of contraceptive use, one of the most important factors, has given women the power to control their childbearing age. There is clear empirical evidence of the postponement of the first child. The improvement of women’s educational level is another vital factor contributing to delayed childbearing, as well as women’s employment rate. In most countries, the lack of family-friendly policies at the workplace is still a critical deterrent for women to have children. Hence, many professional women intend to have children later and have fewer children in order to protect their career.
Other reasons for postponing parenthood are gender equity, partnership changes, housing conditions, unemployment, temporary work, economic uncertainty, divorce and the absence of supportive family policies. Moreover, the advantages of artificial reproductive technologies can be accounted for adjourning to an advanced maternal age.
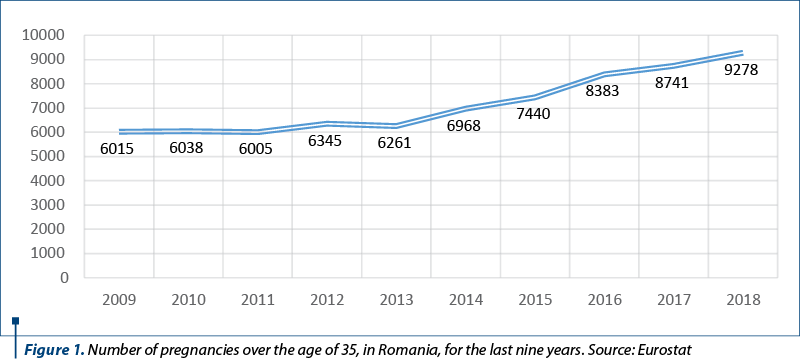
The late childbearing has become a common phenomenon in developed countries and its prevalence is also increasing in developing countries such as Romania(5). Thus, it has been noticed an increased number of live birth rate for women over 35 years old(3). In 2018, in Romania, there were 9278 live births from women who were over 35 years old. This means that approximately 4.57% from the total live births were from a mother included in the advanced maternal age cluster. We used a dataset that included all the births in Romania in the last nine years and found an increased number of pregnancies over the age of 35, from 6015 in 2009 to 9278 in 2018 (Figure 1).
Data from literature regarding advanced maternal age pregnancies and the maternal and fetal outcomes are conflicting and have yielded inconsistent conclusions. Some studies have shown that childbearing in women over 35 years old can be associated with a high risk of hypertensive disorders, gestational diabetes, caesarean birth, low birth weight, preterm birth, fetal growth restriction, placental abruption and stillbirth(4,5). On the other hand, some studies have suggested a favorable effect of advanced maternal age on the neonatal mortality and morbidity among preterm infants(11).
This study attempted to determine the frequency of intrauterine growth restriction, premature birth and low birth weight in advanced maternal age category, in order to provide good healthcare practices.
In the present research, a newborn was considered preterm when the gestational age was less than 37 completed weeks, as calculated from the first day of the last menstrual period, low birth weight newborn was considered if they weighed less than 2500 grams, and intrauterine growth restriction was diagnosed by ultrasound and defined as an estimated fetal weight below the 10th percentile. In the advanced maternal age category, there were included pregnant women aged more than 39 years old.
Objectives
The aim of this paper is to follow-up a group of patients with advanced maternal age (over 39 years old) hospitalized in the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology, Bucharest, and to identify the prevalence and incidence of prematurity and intrauterine growth restriction (IUGR) among advanced maternal age pregnancies, in order to develop a tailored healthcare plan to improve the quality of life and the outcome of pregnant patients at extreme ages.
The research hypothesis starts from the existence of a potential causal link between the extreme age of pregnancy and the identified pathology: extreme age in pregnancy may be a risk factor for the identified pathology and the fact that the control of risk factors for the pathology associated with extreme age during pregnancy may influence the health of both the mother and the child.
Through the results obtained from the research to be carried out, the project aims to improve the healthcare practices both for the mother and the child. Through this project, we want as well to increase the satisfaction with the healthcare process performed by midwives among patients. The results of the research can be transformed into a mother and child healthcare protocol adapted to the pathological conditions identified in advanced age pregnancies and can be disseminated among midwives, and it can also be transformed into a guide manufactured to improve the quality of life of pregnant patients at extreme ages.
Materials and method
This is a retrospective, descriptive study of women with advanced maternal age. The databased used in this study included 109 women (over 35 years old) with their maternal antepartum and postpartum health information. The data were collected in our clinic within a year. We included the patients with premature birth (before 37 weeks of gestation, but more than 24 weeks of gestation), with low birth weight (under 2500 grams) and with intrauterine growth restriction (diagnosed antenatally).
Results
In the following part of the paper, we studied the average age within the group, the conceiving way, the childbirth delivery, the number of premature newborns, the number of fetuses with growth restriction and the average Apgar score at birth.
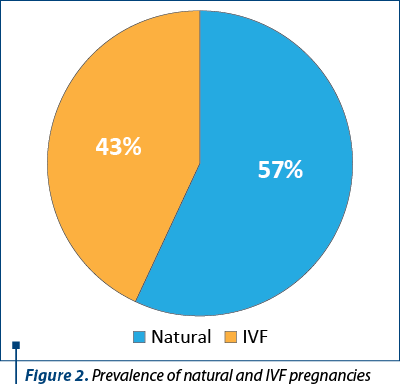
The mean age of the 109 patients with advanced maternal age was 41.2 years old. The parity of the women ranged from 1 to 6. The pregnancies were obtained by natural way (62 pregnancies) and by in vitro fertilization method (47 pregnancies). In Figure 2, we can observe the percentages of the conceiving way.
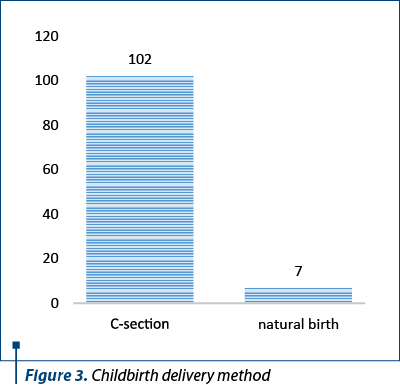
The childbirth delivery method included natural childbirth (6%) and delivery by caesarean surgery (C-section) – 94% (Figure 3).
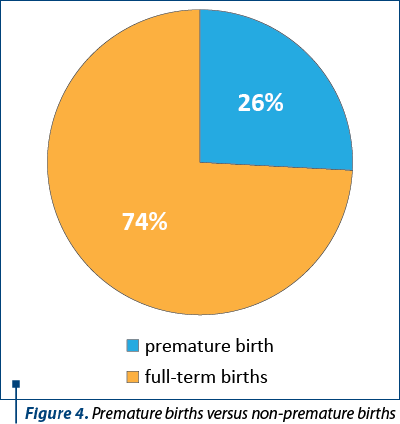
The premature births (28 premature births) in terms of gestational age ranged from 27 weeks of pregnancy to 36.8 weeks of pregnancy. In terms of birth weights, the birth weights of the premature births ranged from 650 grams to 3980 grams, with a mean weight of 2150 grams. The percentages of premature births are represented in Figure 4.
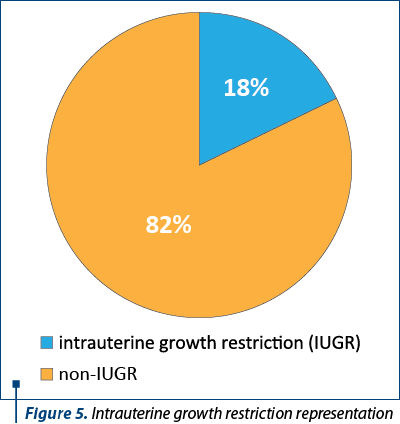
Out of 109 pregnancies, intrauterine growth restriction was diagnosed in 20 pregnancies (Figure 5).
The Apgar score of the 109 newborn infants ranged from 3 to 10, with a mean score of 8.8.
Discussion
More women defer pregnancy to the fifth decade of their life and even further by taking advantage of the artificial reproductive technologies. As a result, the live birth rate for women of advanced maternal age has increased steadily over the past years.
Delaying childbearing comes with age-related diseases that may affect the pregnancy. Age-related pathologies have potentially significant clinical implications for both maternal and fetal health. Identifying the advanced age-related pathologies is a first step in developing and adapting the protocols for providing good healthcare in the prenatal, intrapartum and postpartum period.
We consider it necessary to have a distinct healthcare approach for elderly mothers, in order to identify and prevent unwanted events that may put the pregnancy at risk. Numerous studies have concluded that a pregnancy that occurs at an advanced age can predispose a woman to several complications, such as preeclampsia, placenta praevia, gestational diabetes, premature birth or even neonatal death.
To strengthen our paper, we found a study conducted in Tel Aviv, Israel, that compared the perinatal outcomes between advanced maternal age women and a control group. They had similar results with ours, and they concluded that advanced maternal age increased the rate of preterm delivery, the rate of low birth weight and, overall, the caesarean section delivery rate was increased significantly in the study group compared with the control groups(10).
An explanatory, retrospective case-control study based on the revision of the newborn registers from the Neonatal Screening Center of the province of Alicante concluded that older pregnant mothers were at higher prematurity and low birth weight risk(8), therefore it imposed the need to trace educational interventions to minimize the risk, similar to our objective.
A population-based cohort study elaborated by the University of Manchester (UK) concluded that adverse pregnancy outcomes in AMA are independent of parity and remain after adjusting for the ameliorating effects of higher socioeconomic status(7). The authors also hope the data from their cohort will be one of interest to healthcare providers and women, and they will facilitate the evidence-based counseling of older expectant mothers.
Certainly, there are also some suggestions in the literature that the social advantage may ameliorate some of the effects of advanced maternal age on perinatal outcome, even though the advanced maternal age might be associated with an increased survival without major morbidity among the newborns(9). We found some evidence that suggests the main predictor of outcome is maternal health, and not maternal age(10).
AMA might not be a risk factor for unsatisfactory outcomes, as childbearing women over 35 years old are likely to be better educated and of higher socioeconomic status. Studies suggest that these women are more likely to follow a healthy lifestyle, attend for regular antenatal care and have a positive perception of their pregnancy, factors which are strongly associated with lower rates of poor outcome(11).
As our retrospective study has shown, advanced maternal age has been associated with the need for caesarean section in both primiparous and multiparous women, which leads to many postpartum complications.
Our study retrospectively highlights the increased maternal and fetal risks for pregnancy in these extreme age groups. We presume that pregnancy counseling is essential for this age group, so that a woman can make an informed decision about when to give birth and further to receive customized healthcare based on each and everyone’s needs.
Through this retrospective study, we consider that we have achieved our goal to identify the prevalence and incidence of prematurity and intrauterine growth restriction among advanced maternal age pregnancies and soon to be able to develop a tailored healthcare plan, in order to improve the quality of life and the outcome of pregnant patients at extreme ages.
Conclusions
Thus, we can conclude that the hypothesis of our study is confirmed in this research. Although pregnancy at extreme ages may be associated with significant maternal and fetal risks, old age cannot be considered a risk factor during pregnancy, childbirth and the postpartum period. It should be borne in mind that the negative results of an elderly pregnancy are not entirely due to age, but additional factors, such as the mother’s chronic conditions, the mother’s lifestyle, parity and social environment, may influence negatively the proper evolution of a pregnancy. On this issue, we consider that having good healthcare protocols and working together – childbearing women, doctors, nurses and midwives –, we can achieve a good pregnancy outcome.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Lean SC, Derricott H, Jones RL, Heazell AEP. Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS One. 2017;12(10):e0186287.
- Carolan M, Frankowska D, Lecturer MN. Advanced maternal age and adverse perinatal outcome: a review of the evidence. Midwifery. 2011;27(6):793–801.
- Yogev Y, Melamed N, Bardin R, Tenenbaum-Gavish K, et al. Pregnancy outcome at extremely advanced maternal age. Am J Obstet Gynecol. 2010;203(6):558.e1-7
- Callaway LK, Lust K, McIntyre HD. Pregnancy outcomes in women of very advanced maternal age. Aust N Z J Obstet Gynaecol. 2005;45(1):12-6.
- Dildy GA, Jackson GM, Fowers GK, Oshiro BT, Varner MW, Clark SL. Very advanced maternal age: pregnancy after age 45. Am J Obstet Gynecol.1996;175(3 Pt 1):668-74.
- Dulitzki M, Soriano D, Schiff E, Chetrit A, SMashiach S, Seidman DS. Effect of very advanced maternal age on pregnancy outcome and rate of cesarean delivery. Obstet Gynecol. 1998;92(6):935-9.
- Kenny LC, Lavender T, McNamee R, O’Neill SM, Mills T, et al. Advanced maternal age and adverse pregnancy outcome: evidence from a large contemporary cohort. PLoS One. 2013;8(2):e56583.
- Cortes Castell E, Rizo-Baeza MM, Aguilar Cordero MJ, Rizo-Baeza J, Gil Guillén V. Maternal age as risk factor of prematurity in Spain; Mediterranean area. Nutr Hosp. 2013;28(5):1536-40.
- Kanungo J, James A, McMillan D, Lodha A, Faucher D, Lee SK, Shah PS; Canadian Neonatal Network. Advanced maternal age and the outcomes of preterm neonates: a social paradox? Obstet Gynecol. 2011;118(4):872-7.
- Schwartz A, Many A, Shapira U, et al. Perinatal outcomes of pregnancy in the fifth decade and beyond - a comparison of very advanced maternal age groups. Sci Rep. 2020;10(1):1809.
- Mills TA, Lavender T. Advanced maternal age. Obstet Gynaecol Reprod Med. 2014;24(3):85-90.




