Relapsed giant mucinous cystadenoma – clinical case
Chistadenom mucinos gigant recidivat – caz clinic
Abstract
Giant ovarian mucinous cystadenoma is a benign tumor in most cases and usually appears in adult or middle-aged women. The mucinous cystadenoma is a noncancerous type of ovarian tumor. The ovarian mucinous cystadenoma is the second most frequent benign ovarian tumor and represents approximately 15% of all ovarian tumors. This paper presents the clinical case of a 35-year-old patient admitted to our hospital, in the gynecology department, with a history of repetitive menometrorrhagia, for about six months, diffuse abdominal pain, radiating in the lumbar region and the lower limbs, fatiguability, asthenia, dyspareunia and the voluminal growth of the abdomen in the previous two months. The physical examination, the gynecological examination, the laboratory tests focused on ovarian tumor markers (CA125, HE4, ROMA score) and the echographic examination revealed the existence of a giant ovarian tumoral growth on the only remaining ovary, the left ovary. A particularity of this clinical case is the fact that, five years before, the patient had undergone another surgery for a giant ovarian cyst on the right ovary (mucinous cystadenoma), when both a cystectomy and a right adnexectomy had been performed. In our case, we paid special attention to the values of the ovarian tumor markers, since our goal was to surgically intervene for the excision of the intact cyst, but also to keep the left ovary (a reason why we also asked for an extemporaneous examination), taking into account the missing right ovary and the age of the patient, who was only 35 years old.Keywords
mucinous cystadenomaovarymucinovarian tumor markerscystectomyadnexectomyRezumat
Chistadenomul mucinos gigant al ovarului este o tumoră benignă în majoritatea cazurilor şi apare de obicei la femeile adulte sau de vârstă mijlocie. Chistadenomul mucinos este un tip necanceros de tumoră ovariană. Chistadenomul mucinos ovarian este a doua ca frecvenţă dintre tumorile ovariene benigne şi reprezintă aproximativ 15% din totalul tumorilor ovariene. Această lucrare prezintă cazul clinic al unei paciente în vârstă de 35 de ani, internată în spitalul nostru în secţia de ginecologie, cu un istoric de menometroragii repetitive de aproximativ şase luni, dureri difuze abdominale cu iradiere lombară şi la nivelul membrelor inferioare, fatigabilitate, astenie, dispareunie şi creşterea de volum a abdomenului în ultimele două luni. Examenul fizic, examenul local ginecologic, investigaţiile de laborator cu accent pe markerii tumorali ovarieni (CA125, HE4, scorul ROMA) şi examenul ecografic au decelat existenţa unei formaţiuni tumorale ovariene gigante, dezvoltată pe un ovar unic restant, respectiv ovarul stâng. Ca particularitate, acest caz clinic se remarcă prin faptul că, în urmă cu cinci ani, pacienta a suferit o altă intervenţie chirurgicală pentru un chist gigant ovarian dezvoltat pe ovarul drept (chistadenom mucinos), când s-au practicat chistectomie şi anexectomie dreaptă. În cazul nostru, am ţinut cont îndeosebi de valoarea markerilor tumorali ovarieni, întrucât scopul nostru a fost să intervenim chirurgical pentru extirparea intactă a formaţiunii chistice, dar cu păstrarea ovarului stâng (motiv pentru care am solicitat şi examen extemporaneu), ţinând cont de lipsa ovarului drept, precum şi de vârsta pacientei, care avea doar 35 de ani.Cuvinte Cheie
chistadenom mucinosovarmucinămarkeri tumorali ovarienichistectomieanexectomieIntroduction
Ovarian cysts are a frequent pathology in the gynecological practice.
-
Pathological ovarian cysts are represented by(1):
-
Dermoid cysts or teratomas, that usually affect females under 30 years old and require surgery for their excision. The growth has an embryonic origin and can contain other types of tissues, such as fat, bones, hair or cartilage.
-
Cystadenomas, that form in the ovarian cortex and require surgery for their excision.
-
Endometrioma is a type of cyst formed when endometrial tissue (the mucous membrane that makes up the inner layer of the uterine wall) grows in the ovaries.
In the case of this ovarian pathology, it is compulsory to do a differential diagnosis with ovarian cancer (preoperatively) in order to approach the case correctly from a surgical point of view, but the certainty of the benign characteristic of the excised growth (the mucinous cystadenoma) is offered solely by the anatomopathological examination (intraoperatively, through an extemporaneous examination) and postoperatively(2).
Materials and method
We present the clinical case of a 35-year-old gynecopathic patient with an active sex life and irregular menstrual cycles, who came to our hospital complaining of menstrual irregularities (repetitive menometrorrhagia, for about six months), diffuse abdominal pain, radiating in the lumbar region and the lower limbs, fatigability, asthenia, dyspareunia and a voluminal growth of the abdomen which she had noticed in the last two months.
Among the heredocollateral and personal pathological antecedents, we must mention the fact that the patient’s menarche was at the age of 12 and she had irregular menstrual cycles until the age of 17, when, after a gynecological examination, she was diagnosed with polycystic ovary syndrome and she received an oral contraceptive treatment for 24 months.
Afterwards, the menstrual cycles were regular, and the patient had two pregnancies carried to full term, finalized with caesarean section surgeries, and had no abortions.
Five years ago, the patient underwent another classical surgery for a large ovarian growth developed on the right ovary. After that surgery, the cyst and the right adnexa were excised (declaratively). The patient couldn’t present the hospital discharge papers, but she was able to reproduce the histopathological report from which we noted that the cystic growth excised during the previous surgery was a giant mucinous cystadenoma, and the fact that a right adnexectomy was also performed during the same intervention.
After that surgery (still declaratively), the patient has not taken any hormonal substitution treatment or any other type of treatment.
The general clinical examination highlighted the fact that she was a highly irritable person, also suffering from a mild neurosis.
The inspection revealed the existence of a median subumbilical incision on the abdomen and the local examination (VVE and DVE) revealed a highly ascended, laterally deviated cervix, but also the existence of a tumoral growth of ovalar shape, renitent, which filled the lower abdominal floor, subumbilically, with approximately 100/80 mm in size, a little mobile, but non-painful, with a slightly irregular and slightly bosselated contour.
The access path for the two caesarean section surgeries and for the cystectomy plus right adnexectomy surgery (which had been performed five years ago) was median subumbilical.
The laboratory tests done in the hospital revealed the existence of iron deficiency anemia (Hb=9 g/dl; Ht=34%; serum ferritin=110 ng/mL), slightly elevated ESR (25 mm in 1 hour and 60 mm in 2 hours), along with slightly elevated C-reactive protein (CRP), the rest of the blood and urine test results being within the normal limits.
The transvaginal echography revealed the existence of the cystic tumoral growth on the left ovary, approximately 100/80 mm in size, with an irregular shape, multilocular, but without intracystic vegetation, a thin film of fluid in the Douglas pouch, the uterus with normal shape and size highly deviated to the right by the tumor and the absence of the right adnexa.
The cytobacteriological smear, together with the endocervical culture test and antibiogram, discovered the presence of vaginal candidiasis, while the cytodiagnostic smear indicated the existence of inflammatory infiltrate, the Pap smear being within normal limits.
The diagnosis upon admission was pelvic tumor, while the diagnosis after 24 hours was left ovary tumor. We were going to undertake more tests for the differential diagnosis of ovarian cancer.
CA 125, HE4 and ROMA score tumor markers were collected and were within normal limits, which made us conclude (taking into account the patient’s age and the gynecological pathological antecedents) that this was a new ovarian cyst of a benign nature.
CA125, HE4 (Human Epididymis Protein 4) and ROMA score tumor markers are the most studied ones for the detection of ovarian cancer(3,4).
In our case, we paid a lot of attention to the values of the ovarian tumor markers, since our goal was to proceed surgically to the excision of the cyst, but also to keep the left ovary (a reason why we asked for an extemporaneous examination), taking into account the absence of the right ovary (removed during the previous surgery) and the patient’s age, 35 years old.
We intervened surgically with a classical approach and with general anesthesia (IOT), making a median subumbilical incision and excising the old scar.
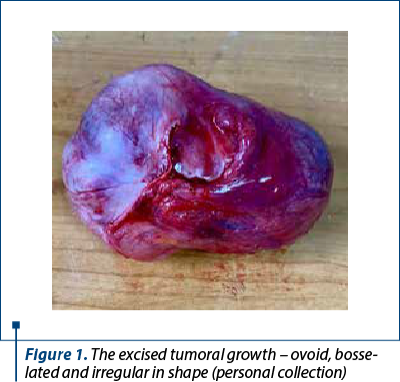
Intraoperatively, upon opening the peritoneal cavity, we noticed the existence of a voluminous tumoral growth, renitent, incapsulated, slightly irregular and slightly bosselated (Figure 1), the left ovary almost completely attached to the growth, but with an existing small cleavage space, the absence of the right adnexa (from the previous surgery) and, also, the absence of intraperitoneal deposits which would suggest malignancy.
We proceeded to a gentle detachment in the cleavage space between the ovary and the tumor, slowly and carefully releasing the ovary from the tumoral growth (to reduce as much as possible the risk of a hemorrhage and to preserve the left ovary), and the tumor was excised in its entirety, without accidentally opening it intraoperatively.
We requested an extemporaneous examination to be certain of the benign character of the excised tumoral growth, in order to preserve the remaining left ovary. When we were informed that it was a benign tumor, we closed the abdomen in the classical way, leaving in a peritoneal drain in the Douglas pouch and applying the intradermal suture at cutaneous level.
Postoperatively, the evolution was favorable. The patient did a four-day antithrombotic, antalgic and antibiotic treatment. We discharged the patient on the fifth day and on the nineth day we removed the intradermal suture.
The extemporaneous histopathological examination revealed at a macroscopic level a tumoral growth of 10.5/7.5/6 cm, multilocular, with a bosselated external surface and hemorrhagic areas (Figure 2), walls with thickened areas and a smooth internal surface, apparently without vegetation, a slightly hemorrhagic serocitrin and gelatinous contents, and at a microscopic level, cyst fragments lined with simple cylindrical mucous secretory epithelium, fibrous stroma with hemorrhagic areas which included several glandular structures lined with the same epithelium as the surface.

In section, the cavity was divided by very thin interlocular septa into several loculi of various sizes which contained mucoid, viscous and adherent material (Figure 3).
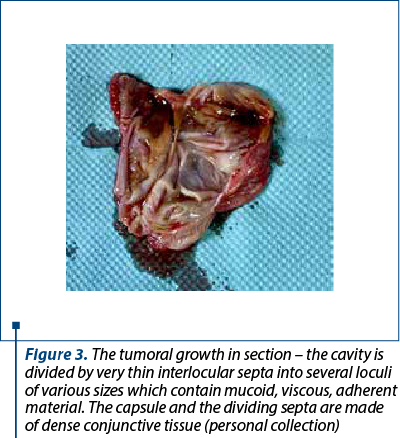
The capsule and the dividing septa were made of dense conjunctive tissue.
Microscopic aspect
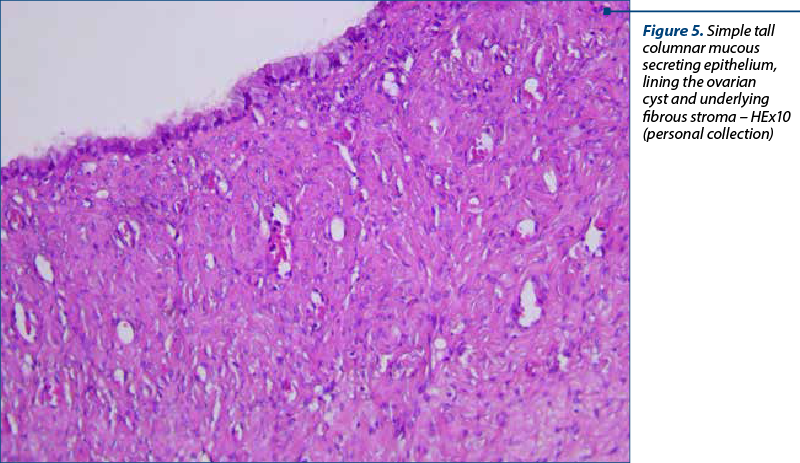
Microscopically, the multilocular cyst is lined by simple tall columnar mucous secreting epithelium (Figure 4) with a basal disposition of the nuclei, abundant cytoplasm and apical accumulation of mucinous substance.
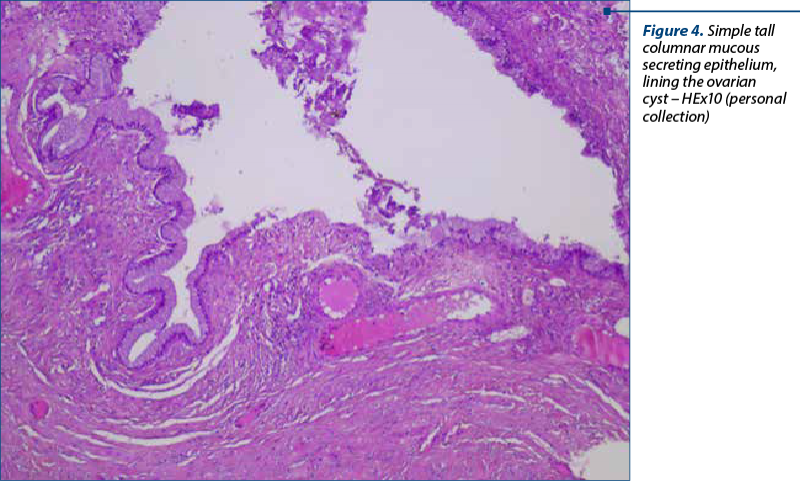
The epithelium presented focal vaginations, forming several glandular structures lined by the same surface lining epithelium. The stroma was fibrous, with hemorrhagic areas (Figure 5). The Fallopian tube had a normal microscopically aspect.
The evolution of the patient was favorable. The postoperative checkups after one, three and six months did not reveal any pathological changes at the level of the remaining internal genital organs, the menstrual cycles have become regular again, and the patient resumed her daily activities.
At her three-month postoperative checkup, the patient was prescribed COC treatment for 12 consecutive months, in order to make the remaining left ovary dormant.
We have no information about the health of the patient 12 months after surgery, since she did not come in for her preestablished checkup.
Discussion
A mucinous cystadenoma is a noncancerous type of ovarian tumor(5). Although these tumors are noncancerous, they can grow to large sizes and can cause significant symptoms for many patients(2).
The ovarian mucinous cystadenoma is the second most frequent of all benign ovarian tumors and represents approximately 15% of all ovarian tumors(1). In contrast to serous tumors, it appears bilaterally in only 3-7% of cases (rarely).
These tumors are rarely malignant, having a much more favorable prognosis than their serous correspondents(1). The mucinous cystadenoma appears more frequently during the third and fourth decades of life and, in 10% of cases, after the installation of menopause(2).
Regarding the methods of investigation, the transvaginal echography is the means of evaluating adnexal tumoral growth (including the mucinous cystadenoma), due to the fact that it allows for a detailed description of the macroscopic characteristics of the tumors, can offer high quality images and is relatively cheap, being the first method used(6).
When the lesion is large and complex, it presents septa on the inside, has different irregularities of the wall, just like in the case of existing bilateral lesions, and the suspicion of cancer may arise. In such cases, the measurement of tumor markers is compulsory(7).
The CA125 and HE4 (Human Epididymis Protein 4) tumor markers are the most studied for the detection of ovarian cancer(4,8). It has been noticed that they have a higher success rate in diagnosing ovarian cancer than CA19-9, CA72-4 or the carcinoembryonic antigen (CEA)(3).
The CA-125 tumor marker is elevated in less than half of the patients in the early stages of epithelial ovarian cancer and in approximately 80% of the patients with epithelial ovarian cancer(4). Measuring the CA-125 is considered the gold standard in the management of ovarian cancer(9).
Magnetic resonance imaging (MRI) may detect the tumor modifications characteristic to malignant ovarian tumors with a sensitivity of 92% and a specificity of 88% for the detection of malignancy(10). Computed tomography (CT) is suitable for the cases when the tumor exceeds the adnexa.
In our patient’s case, the ultrasound and other laboratory examinations did not raise any suspicions but the tumor needed to be excised, nonetheless. The classical approach was preferred due to the large size of the tumor and to our endeavor to excise the tumor intact and preserve the single remaining ovary.
Macroscopically, mucinous tumors are usually larger than the serous ones and are known for their gigantic size, in some cases. They measure between 1 and 50 cm in diameter, but most of them measure between 10 and 35 cm in diameter(1).
They are frequently completely cystic growths and multilocular. The external surface is smooth, rarely bosselated, whitish grey in color and without extracystic papillary extensions.
In section, the cavity is divided by very thin interlocular septa into several loculi of various sizes, which contain mucoid, viscous and adherent material. The contents may be red or brown if there was an intracystic hemorrhage. Intracystic papillary processes were detected in 10-20% of tumors and are more frequent in the malignant variants. The capsule and the interlocular septa are made of dense conjunctive tissue(5).
Microscopically, the cysts are lined by tall columnar secretory epithelium, with a basal disposition of the nuclei, abundant cytoplasm and apical accumulation of mucinous substance. These cells look like the secretory cells of the endocervix and the intestine. Between these cells are dispersed argentaffin cells and Paneth cells.
The treatment of benign mucinous cystadenoma in young women consists of a unilateral cystectomy or oophorectomy, with the inspection of the collateral ovary. In patients older than 40 years of age, a total hysterectomy with a bilateral adnexectomy is performed(2).
The handling of the tumor growth must be gentle, in order to avoid its rupturing and the dissemination of the mucinous tissue in the peritoneal cavity, with the appearance of pseudomyxoma peritonei.
Surgical therapy is essential in cases that become symptomatic, regardless of age or menstrual status, especially for those where there are changes in the characteristics of cysts and the increase of the values of tumor markers(2).
-
In our case, we took into consideration the following aspects:
-
the young age of the patient (35 years old)
-
the existence of a single remaining adnexa
-
the existence of the giant tumoral growth on the single remaining adnexa
-
our attempt to preserve the remaining adnexa
-
the values of the tumor markers (within normal limits)
-
the request for an extemporaneous examination on the day of the surgery
-
the attempt to find the cleavage space intraoperatively (successful)
-
ensuring efficient and optimal hemostasis when detaching and depolishing the tumor growth
-
the attempt to excise the tumor intact, reducing as much as possible the risk of accidental rupture intraoperatively.
Regarding the clinical case described here, one particularity is the fact that a second mucinous cystadenoma developed rapidly, only five years after the first cystadenoma (which was excised together with the adnexa), the bilaterality of this pathology being reduced (3-7% of cases).
Another peculiarity is the fact that the first surgery was performed when the patient was 30 years old. Her tumor growth (cyst) was removed together with the adnexa (right), and the patient was left with the single adnexa on which, five years later, another giant mucinous cystadenoma developed, which required another surgical intervention (at the age of 35).
Yet another particularity of the case is the young age of the patient who came to the hospital to be diagnosed and to receive specialist therapeutic conduct, taking into account the fact that the patient had one adnexa excised during the previous surgery and now, at the age of 35, she had to undergo another surgical procedure with the preservation of the remaining ovary as much as possible and the removal of the tumor growth intact, in order to avoid its rupture with the dissemination of the mucinous tissue in the peritoneal cavity and the appearance of pseudomyxoma peritonei.
The experience of the surgeon, the finding of the cleavage space between the remaining ovary and the mucinous cystadenoma, the possibility to slowly and efficiently detach and depolish the tumor, and ensuring efficient hemostasis made possible the excision of the tumor growth intact and the preservation of the single remaining ovary.
What we consider optimal for the patient was the request for an extemporaneous examination from the anatomopathologist, the diagnosis (mucinous cystadenoma) giving us the chance to preserve the patient’s adnexa, taking into account her young age. It is well known that the diagnosis of the anatomopathologist during the extemporaneous examination may change the type of surgery performed or the treatment recommended after surgery.
The surgery that we performed was a cystectomy through a laparotomy and extemporaneous examination, preserving the single remaining adnexa.
Conclusions
The giant mucinous cystadenoma of the ovary is a benign tumor, in most cases, and usually appears in adult middle-aged women(5).
Ovarian cysts remain a frequent pathology that must be kept under observation and, in many cases, must be resolved surgically.
The giant mucinous cystadenoma can be resolved surgically through a classical approach of the abdominal wall, with a large median subumbilical incision, possibly extended lateral-umbilically to the left, in order to excise the tumor growth intact and to avoid its rupture with the dissemination of the mucinous tissue in the peritoneal cavity and the appearance of pseudomyxoma peritonei(2).
Only the histopathological examination can guarantee the benign characteristic of the excised tumor. Ideally, we need to request (where possible) the anatomopathologist to do an extemporaneous examination in order to perform preservation surgery (in the case of young women).
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, et al. (eds). SEER Cancer Statistics Review, 1975-2014, National Cancer Institute. Bethesda MD. Available at: https://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017.
-
Biggs WS, Marks ST. Diagnosis and management of adnexal masses. Am Fam Physician. 2016;93(8):676-81.
-
Granato T, Porpora MG, Longo F, Angeloni A, Manganaro L, Anastasi E. HE4 in the differential diagnosis of ovarian masses. Clin Chim Acta. 2015;446:147-55.
-
Jacobs I, Bast RC Jr. The CA 125 tumor-associated antigen: a review of the literature. Hum Reprod. 1989;4(1):1-12.
-
Dodge JE, Covens AL, Lacchetti C, Elit LM, Le T, Devries-Aboud M, et al. Preoperative identification of a suspicious adnexal mass: a systematic review and meta-analysis. Gynecol Oncol. 2012;126(1):157-66.
-
Smorgick N, Maymon R. Assessment of adnexal masses using ultrasound: a practical review. Int J Womens Health. 2014;6:857-63.
-
Lycke M, Kristjansdottir B, Sundfeldt K. A multicenter clinical trial validating the performance of HE4, CA125, risk of ovarian malignancy algorithm and risk of malignancy index. Gynecol Oncol. 2018;151(1):159-65.
-
Anton C, Carvalho FM, Oliveira EI, Maciel GA, Baracat EC, Carvalho JP. A comparison of CA125, HE4, risk ovarian malignancy algorithm (ROMA), and risk malignancy index (RMI) for the classification of ovarian masses. Clinics (Sao Paulo). 2012;67(5):437-41.
-
Hentze JL, Høgdall C, Kjær SK, Blaakær J, Høgdall E. Searching for new biomarkers in ovarian cancer patients: Rationale and design of a retrospective study under the Mermaid III project. Contemp Clin Trials Commun. 2017;8:167-74.
-
Ekerhovd E, Wienerroith H, Staudach A, Granberg S. Preoperative assessment of unilocular adnexal cysts by transvaginal ultrasonography: A comparison between ultrasonographic morphologic imaging and histopathologic diagnosis. Am J Obstet Gynecol. 2001;184(2):48-54.



