Influenţa variabilelor clinice şi paraclinice ale pacientei asupra eşecului în a obţine o sarcină după embriotransfer: evaluare prin analiză statistică
Influence of clinical and paraclinical variables of the patient in the failure to achieve a pregnancy after embryotransfer: statistical analysis evaluation
Abstract
We conducted this observational prospective study in order to establish to what extent do the clinical and paraclinical characteristics of the patient and the factors that determine infertility also negatively influence pregnancy rate (PR) per embryotransfer. We included 79 women who underwent 145 embryotransfers and we analyzed the positive β-hCG test result. We identified that the following parameters are not statistically significantly correlated to the failure rate: smoking (p=0.7230, OR=1.23), drug use (p=0.7850, OR=1.38), BMI (p=0.4210, OR=1.04), history of infertility, family illness (p=0.3212, OR=1.64), history of miscarriages (p=0.4438, OR=0.61) or abortions (p=0.9842, OR=0.99), previous ectopic pregnancy (p=0.6880, OR=1.30), dyspareunia (p=0.5400, OR=1.43), dysmenorrhea (p=0.4232, OR=0.65), endometriosis (p=0.1150, OR=2.43), impermeable fallopian tubes (p=0.1676, OR=2.11). AMH is not an independent risk factor for pregnancy failure either (p=0.1690, OR=0.79). Age and menarche are risk factors. Age predisposes to a 3.30 times higher failure rate to obtain a pregnancy (calculated cutoff: 34 years old; p=0.0210; OR=3.30). A patient who had menarche before 13 years old (calculated cutoff) has a four times higher risk of failure to obtain a biochemical pregnancy (p=0.0126, OR=3.91). As a conclusion, after reaching the embryo transfer point, the clinical and paraclinical characteristics of the patient are not independent negative factors on PR, except for patient’s age and menarche time.Keywords
embryotransferpregnacy raterisk factorsRezumat
Am realizat acest studiu prospectiv observaţional pentru a vedea în ce măsură caracteristicile clinice şi paraclinice ale pacientei şi factorii care determină infertilitatea influenţează şi rata de sarcini (PR) per embriotransfer. Am inclus 79 de femei care au efectuat 145 de embriotransferuri şi am analizat testul β-hCG pozitiv. Am identificat faptul că următorii parametri nu sunt semnificativ statistic corelaţi cu rata de eşec: fumatul (p=0,7230, OR=1,23), consumul de droguri (p=0,7850, OR=1,38), IMC (p=0,4210, OR=1,04), antecedente de infertilitate, boli familiale (p=0,3212, OR=1,64), istoricul de avorturi spontane (p=0,44438, OR=0,61) sau avorturi (p=0,9842, OR=0,99), sarcina ectopică anterioară (p=0,6880, OR=1,30), dispareunia (p=0,5400, OR=1,43), dismenoreea (p=0,4232, OR=0,65), endometrioza (p=0,1150, OR=2,43), trompe uterine impermeabile (p=0,1667, OR=2,11). Nici AMH nu este un factor de risc independent pentru eşecul obţinerii sarcinii (p=0,1690, OR=0,79). Vârsta pacientei şi menarha sunt factori de risc. Vârsta predispune la o rată de eşec de 3,3 ori mai mare pentru a obţine o sarcină (cutoff calculat: 34 de ani; p=0,0210; OR=3,30). O pacientă care a avut menarha înainte de 13 ani (cutoff calculat) are un risc de patru ori mai mare de eşec la obţinerea unei sarcini biochimice (p=0,0126, OR=3,91). Ca o concluzie, după atingerea punctului de transfer embrionar, caracteristicile clinice şi paraclinice ale pacientei nu sunt factori negativi independenţi asupra PR, cu excepţia vârstei pacientei şi a vârstei de menarhă.Cuvinte Cheie
embriotransferrată de sarcinifactori de riscIntroduction
1. Working hypothesis
We conducted this study in order to evaluate what clinical and paraclinical variables of the patients influence pregnancy rates in assisted human reproduction techniques.
2. Relevance of the paper’s topic
Infertility is an important issue that frequently influences couple’s life(1) worldwide, as well as in Romania, being noticed a decrease in the pregnancy rate(2).
The causes of infertility are diverse, having either female, male or combined etiology, as well as a psychological-emotional origin. In women, the obstruction of the fallopian tubes, infections, problems of hormonal or anatomical origin, anovulation or low quality of oocytes are some of the health issues that a woman faces when trying to have a child(3-5).
The question we asked below, which is the subject of the current paper, is: to what extent do the factors that determine infertility also influence the rate of pregnancy through assisted human reproduction techniques?(6-12)
3. Objectives
The evaluation by statistical analysis of the influence of clinical and paraclinical variables on pregnancy failure (biochemical) after embryotransfer.
Materials and method
Study design
We performed a prospective, observational, non-randomized study on a sample of 79 women who underwent 145 embryo transfers in the Department of Assisted Human Reproduction of the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology, Bucharest, between March 2018 and May 2020.
Criteria for inclusion: patients undergoing embryo transfer in the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology who signed a consent form in order to participate in this study.
The exclusion criteria: the refusal to sign the consent form.
Analyzed variables
To perform the analysis on the sample of patients who participated in our study, the success has been quantified per embryotransfer by biochemical pregnancy rate (obtaining a positive b-hCG result).
Statistical analysis
A usual descriptive analysis was performed. A simple univariate binomial logistic regression was used in the inferential analysis, with the dependent variable represented by the success, respectively the patient’s failure to obtain the biochemical pregnancy. The various clinical, paraclinical and demographic parameters followed in the study were used as independent variables.
In the following tables and figures, the data are presented as mean ± standard deviation (DS), median (Inter Quartile Range = IQR) and minimum to maximum for continuous variables. The category variables (smokers, previous abortions, previous ectopic pregnancies etc.) are presented in the form of absolute frequencies (relative frequencies = percentages).
Results
1. Variable distribution
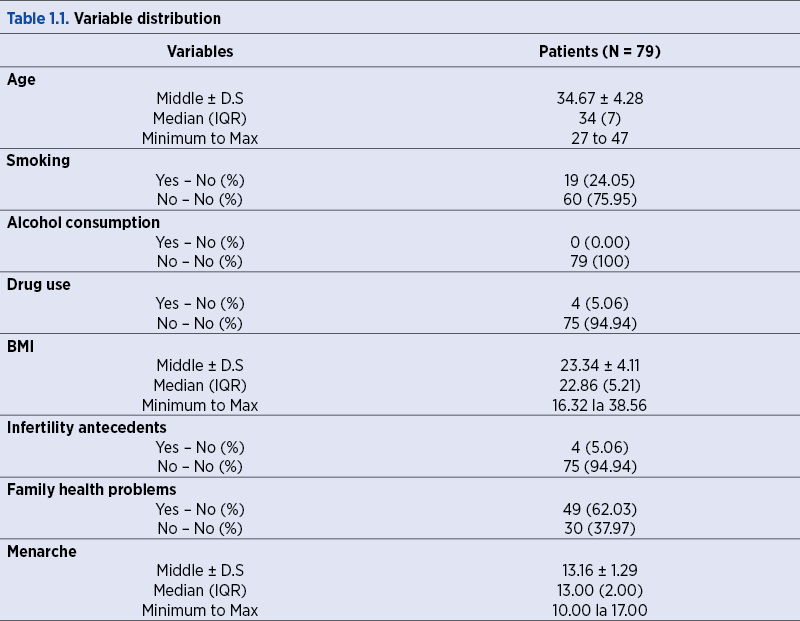
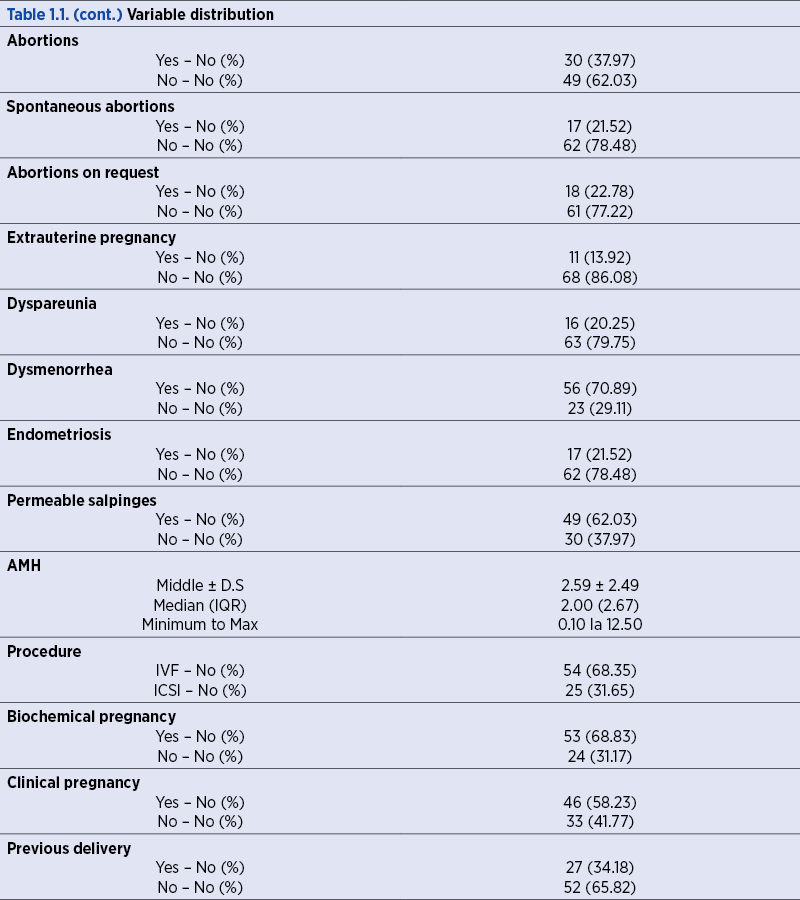
We analyzed the distribution of each variable in our sample.
2. The influence of clinical and paraclinical variables on obtaining a biochemical pregnancy
Then, we performed the analysis of the variables aforementioned, in order to determine whether or not they influence the obtaining of the biochemical pregnancy, the following calculations having in the foreground the failure to obtain the biochemical pregnancy (positive b-hCG value).
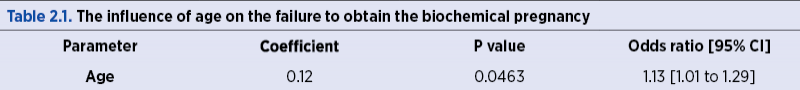
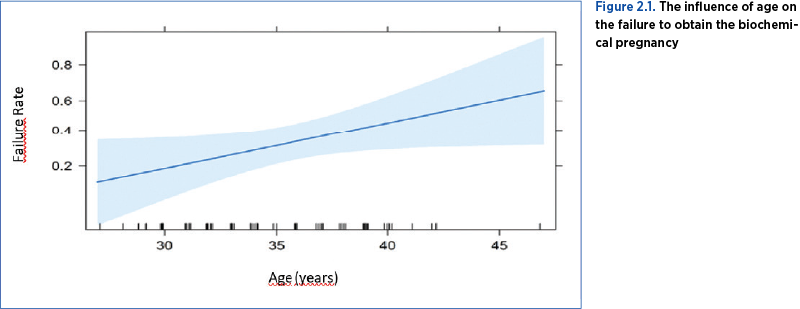
2.1 Age. Our group age range was 27 to 47 years old. We noticed that an elderly age was prone to a higher failure rate of obtaining biochemical pregnancy, an additional year being associated with a 13% increase in failure (p<0.05) (Table 2.1, Figure 2.1).
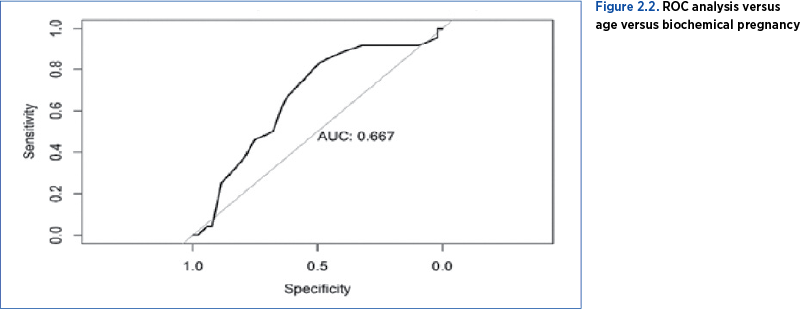
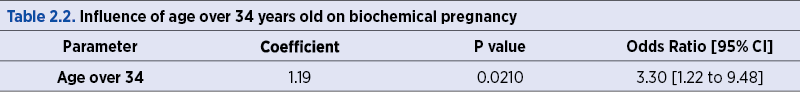
With the help of a ROC analysis, a cutoff value for age was obtained, this being 34 years old, corresponding to a specificity of 83.33% and a sensitivity of 49.05% (Figure 2.2).
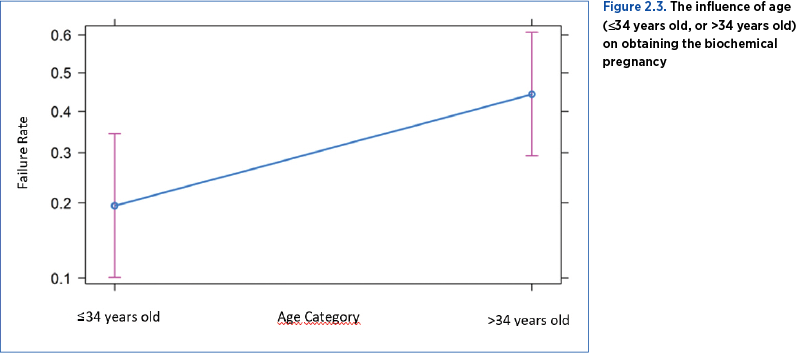
Thus, it was highlighted that a patient over 34 years old, compared to a patient of maximum 34 years old, has a 3.30 times higher risk of having a failure in obtaining the biochemical pregnancy (p<0.05) – Table 2.2, Figure 2.3.
2.2. Next, we analyzed the influence of smoking, drug use, Body Mass Index (BMI), infertility antecedents, familial diseases, previous miscarriages, abortions on demand, the existence of previous abortions (regardless of type), previous ectopic pregnancy, dyspareunia, dysmenorrhea, endometriosis, and AMH as independent risk factors influencing the failure to obtain the biochemical pregnancy. No statistically significant effect was observed (p>0.05; Table 2.3), so we can say that these factors do not influence the failure to obtain a biochemical pregnancy in women performing embryotransfer.
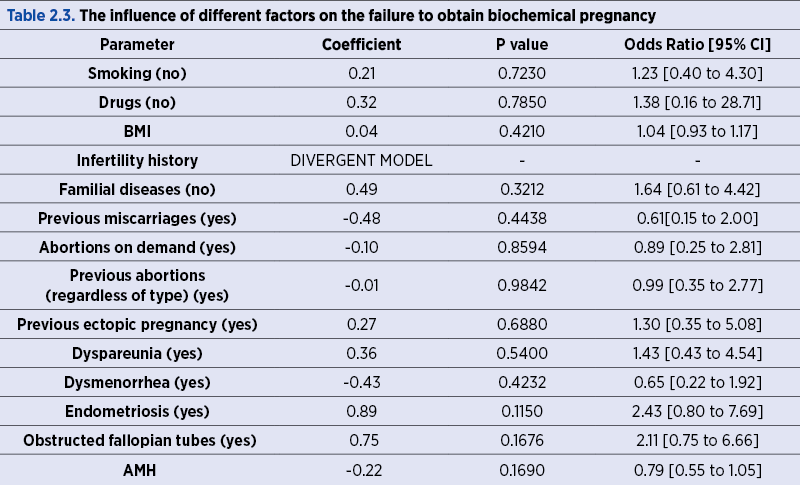
We must note that the influence of the infertility antecedents on the failure to obtain the biochemical pregnancy was not possible in our study, because the number of patients who had such problems was too small (only four patients and none of them obtained a biochemical pregnancy), therefore it was not possible to achieve a logistic regression, the model being divergent.
Regarding endometriosis, no statistically significant influences were highlighted (p>0.05). Even though the result of the analysis (odds ratio 2.43) suggests that patients with endometriosis have a 2.43 times higher risk of failure to obtain a pregnancy, the fact that the statistical power is weak (p=0.115) prevents us from saying this according to the our study (probably due to the small number of patients with endometriosis included).
Regarding AMH, the analysis was without statistical significance (p>0.05). AMH alone, when other factors such as age are not taken into account, does not influence the biochemical pregnancy rate.
2.3. Menarche age influences the pregnancy rate. If menarche appears later, it is associated with a better rate of having a pregnancy (Table 2.4). The failure rate decreases progressively with the passing of the years, so that the best fertilization rates were obtained by patients with menarche at 17 years old, and the lowest rate, by those with menarche at 11 years old, in our studied group (Figure 2.4).
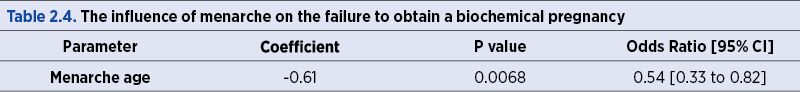
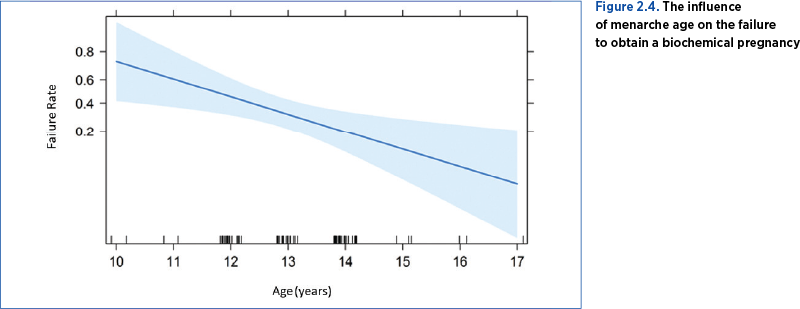
In this regard, we performed an ROC analysis, which highlighted a cutoff value for menarche that appeared at the age of 13 years old, with a specificity of 43.40% and a sensitivity of 25%.
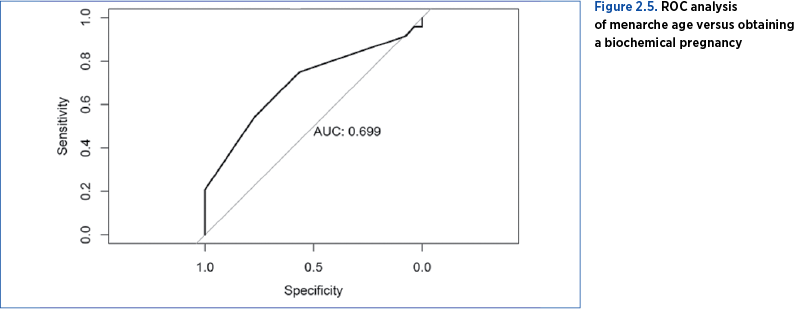
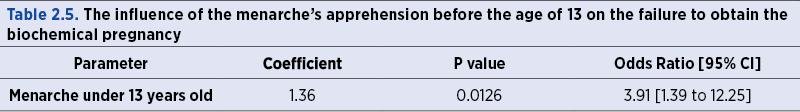
The patients were divided into two categories: patients who had menarche up to and including the age of 13, and patients who had menarche after the age of 13 years old, being observed that the first category has a risk of failure to obtain a biochemical pregnancy almost four times higher than the second one (p<0.05) – Table 2.5. In conclusion, the later the patients had menarche, the more successful they were in obtaining a higher rate of biochemical pregnancy.
Conclusions
The variables that change the rate of obtaining a biochemical pregnancy with statistically significant results are: mother’s age and menarche age. The influence of other variables in patients performing assisted human reproduction techniques is of no statistically significant value.
Following the study, we can draw the following conclusions, analyzing the results from the point of view of statistical analysis:
1. In case of patients undergoing assisted human reproduction treatments, the failure rates of obtaining a biochemical pregnancy are not statistically significantly influenced by the following parameters: smoking (p=0.7230, OR=1.23), drug use (p=0.7850, OR=1.38), BMI (p=0.4210, OR=1.04), history of infertility, family illness (p=0.3212, OR=1.64), history of miscarriages (p=0.4438, OR=0.61), previous abortions on demand (p=0.8594, OR=0.89), abortions regardless of type (p=0.9842, OR=0.99), previous ectopic pregnancy (p=0.6880, OR=1.30), dyspareunia (p=0.5400, OR=1.43), dysmenorrhea (p=0.4232, OR=0.65), endometriosis (p=0.1150, OR=2.43), impermeable fallopian tubes (p=0.1676, OR=2.11), AMH (p=0.1690, OR=0.79), type of procedure performed (ICSI or IVF) (p=0.4334, OR=0.64).
2. In patients undergoing assisted human reproduction treatments, old age predisposes to a higher rate of failure to obtain a biochemical pregnancy. Thus, the calculated cutoff age was 34 years old. A patient over 34 years of age has, compared to a patient of maximum 34 years old, a 3.30 times higher risk of failure in obtaining the biochemical pregnancy (p=0.0210, OR=3.30).
3. In case of patients undergoing assisted human reproduction treatments, the earlier the menarche appears, the greater the risk of failure to obtain the biochemical pregnancy. Thus, the cutoff age calculated by the menarche was 13 years old. A patient who had menarche up to a maximum of 13 years old has a risk of failure to obtain a biochemical pregnancy almost four times higher than patients who had menarche at the age of 13 years old (p=0.0126, OR=3.91).
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Valsangkar S, et al. An evaluation of the effect of infertility on marital, sexual satisfaction indices and health-related quality of life in women. J Hum Reprod Sci. 2011 May;4(2):80-5.
- Nahman N. Romanian IVF: a brief history through the ‘lens’ of labour, migration and global egg donation markets. Reprod Biomed Soc Online. 2016;2:79-87. doi:10.1016/j.rbms.2016.06.001.
- Deshpande PS, et al. Causes and Prevalence of Factors Causing Infertility in a Public Health Facility. J Hum Reprod Sci. Oct-Dec 2019;12(4):287-293. doi: 10.4103/jhrs.JHRS_140_18.
- Petraglia F, Serour G, Chapron C. The changing prevalence of infertility. Int J Gynaecol Obstet. 2013 Sep;123(Suppl 2):S4-8. doi: 10.1016/j.ijgo.2013.09.005.
- Vander Borght M, Wyns C. Fertility and infertility: Definition and epidemiology. Clin Biochem. 2018 Dec; 62:2-10. doi: 10.1016/j.clinbiochem.2018.03.012.
- Ni L, Sadiq S, Mao Y, Cui Y, Wang W, Liu J. Influence of various tubal surgeries to serum antimullerian hormone level and outcome of the subsequent IVF-ET treatment. Gynecol Endocrinol. 2013;29(4):345-9. doi: 10.3109/09513590.2012.743004.
- Meng J, Zhu M, Shen W, et al. Influence of surgical evacuation on pregnancy outcomes of subsequent embryo transfer cycle following miscarriage in an initial IVF cycle: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19:409. https://doi.org/10.1186/s12884-019-2543-9.
- Zhang J, Liu H, Mao X, et al. Effect of body mass index on pregnancy outcomes in a freeze-all policy: an analysis of 22,043 first autologous frozen-thawed embryo transfer cycles in China. BMC Med. 2019 Jun 26;17(1):114. https://doi.org/10.1186/s12916-019-1354-1.
- Gomez R, Schorsch M, Hahn T, et al. The influence of AMH on IVF success. Arch Gynecol Obstet. 2016;293:667-673. https://doi.org/10.1007/s00404-015-3901-0.
- Jiao Z, Zhuang G, Zhou C, Xu Y, Liang X, Li L, Deng M. Influence of advanced age on the outcome of in vitro fertilization and embryo transfer. Zhonghua Fu Chan Ke Za Zhi. 2002 Apr;37(4):223-6 [Chinese].
- Behie A, O’Donnell M. Prenatal smoking and age at menarche: Influence of the prenatal environment on the timing of puberty. Human reproduction (Oxford, England). 2015 Apr;30(4):957-62.
- Lin J, Huang J, Zhu Q, Kuang Y, Cai R, Wang Y. Effect of Maternal Age on Pregnancy or Neonatal Outcomes Among 4,958 Infertile Women Using a Freeze-All Strategy. Front Med (Lausanne). 2020 Jan 10;6:316. doi: 10.3389/fmed.2019.00316.





