Aneurysmal cyst of bone, a complex histopathological lesion – case presentation, differential diagnosis and correlation of imaging data
Chistul osos anevrismal, o leziune complexă histopatologică – prezentare de caz, diagnostic diferenţial şi corelaţii cu datele imagistice
Abstract
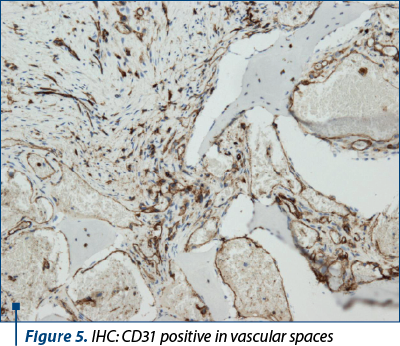
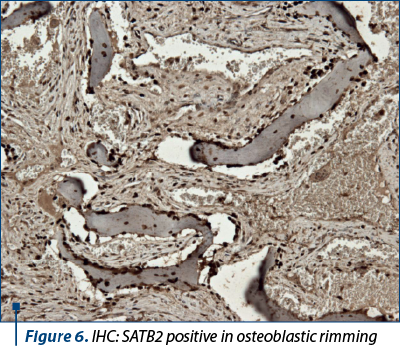
Aneurysmal bone cyst (ABC) is a benign osteolytic, expansile, sometimes destructive but self-limited bone lesion, composed of blood-filled channels and cystic spaces that are separated by stromal fibrous septae. We present the case of a 29-year-old female patient who discovered a deformity of the left forearm after trauma. The imaging data (simple radiography and whole-body scintigraphy) suggested the following diagnosis: low-grade central osteosarcoma, eosinophilic granuloma, Ewing sarcoma or osteoblastoma. The histologic examination of the bone biopsy showed a benign vascular lesion with overlapping features of ABC and osteoblastoma with ABC-like changes. The immunohistochemical tests (CD31, CD56, SATB2, MDM2, CD45 and Ki-67) were in favor of aneurysmal bone cyst, but they could not definitively exclude an osteoblastoma with ABC-like changes. We discuss each of the aforementioned differential diagnoses from the histopathological point of view, and we found arguments favoring both ABC and osteoblastoma with ABC-like changes. We conclude on the importance of correlations between the imaging data and the histopathological diagnostic.Keywords
aneurysmal bone cystosteoblastomaimmunohistochemistryimaging data and histopathologic correlationRezumat
Chistul osos anevrismal (COA) este o leziune osoasă osteolitică, expansivă, uneori distructivă, dar autolimitantă, fiind constituită din spaţii chistice vasculare separate de o stromă fibroasă. Prezentăm cazul unei paciente de 29 de ani care a descoperit o diformitate a antebraţului stâng după un traumatism. Datele imagistice (radiografie simplă şi scintigrafie osoasă) au sugerat următoarele diagnostice: osteosarcom central de grad scăzut, granulom eozinofil, sarcom Ewing sau osteoblastom. Examinarea histologică a biopsiei osoase a arătat o leziune vasculară compatibilă cu trăsături superpozabile între COA şi osteoblastomul asociat cu modificări de tip COA. Testele imunohistochimice (CD31, CD56, SATB2, MDM2, CD45 şi Ki-67) au fost în favoarea unui chist osos anevrismal, fără a putea exclude un osteoblastom cu modificări de tip COA. Se discută fiecare dintre aceste diagnostice diferenţiale menţionate anterior din punct de vedere histopatologic, găsind argumente pentru cele două entităţi, COA şi osteoblastom cu modificări de tip COA. Concluzionăm asupra importanţei corelaţiei dintre datele imagistice şi diagnosticul histopatologic.Cuvinte Cheie
chist osos anevrismalosteoblastomimunohistochimiecorelaţie date imagistice cu histologieIntroduction
Aneurysmal bone cyst (ABC) is a benign vascular neoplasm of bone. ABC can be broadly classified as primary and secondary (associated with another histologic different lesion). Both of them manifest as an expansile, destructive bone mass predominantly found in the vertebral bodies and long bones, usually well circumscribed but seldom with worrisome radiological features that leads to confusion with malignancy(1,2).
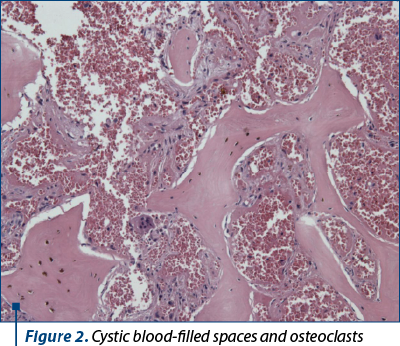
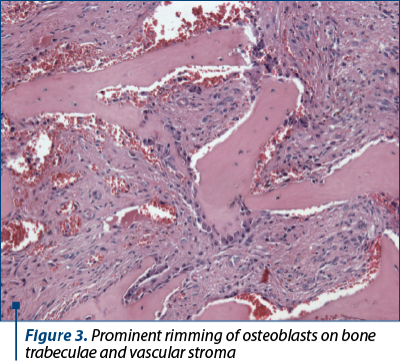
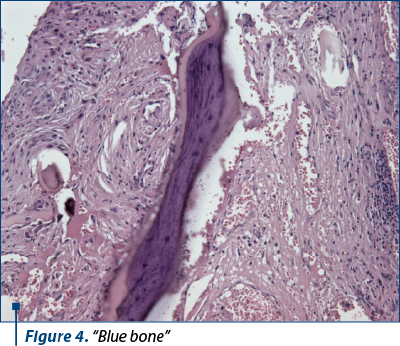
Histologically, conventional ABC consists of blood-filled, cystic spaces separated by fibrous septae composed of uniform bland fibroblast-like cells with mitotic activity commonly present but without atypical forms, scattered multinucleated osteoclast giant cells, reactive woven bone rimmed by osteoblasts, sometimes irregularly mineralized, known as “blue-bone”. Solid ABC variant consists of a few or no blood-filled cystic spaces and has the same components as conventional ABC, but it can present as a more hypercellular form due to the abundance of the fibrous stromal component, and may contain additional fibromyxoid matrix(3-7).
Case report
A 29-year-old female patient was referred to our anatomopathological department for a second opinion on a biopsy specimen taken from a bone lesion localized in the midshaft of the left cubitus, with imaging data suggesting different histopathological diagnosis: Ewing sarcoma, eosinophilic granuloma, low-grade central osteosarcoma or an osteoblastoma. The biopsy was processed in another medical center, with the diagnosis of low-grade osteosarcoma which gave credit to one of the radiological assumptions (Figure 1).
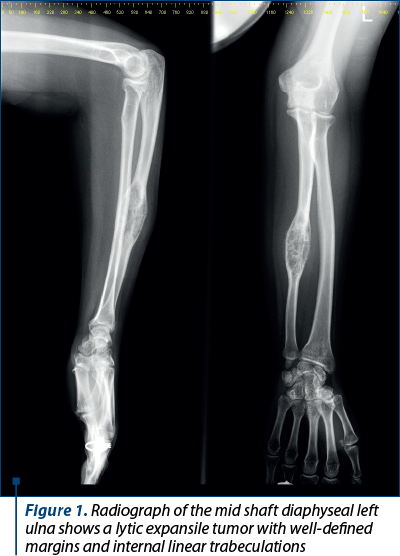
The whole-body scintigraphy revealed triphasic anomalies (vascular, tissular and osseous) on a unique mass located in the one-third middle of the cubitus with the hypercaptation and hiperfixation of the osteotropic radiotracer. The scintigraphic examination reported these changes compatible with an osteoblastoma.
Method. The paraffin block, including the biopsy bone specimen that we are referring to, was also examined in our laboratory on hematoxylin-eosin slides. We performed immunohistochemical tests with LEICA BOND III automatic machine using Leica Bond antibodies for: CD56 (clone 564), Ki-67 (clone MM1), CD31 (clone JC70A), and CD45 (clone X16/99). SATB2 (clone EPNCIR130A), MDM2 (clone 1B10) and ERG (clone 9FY) were performed manually.
The H&E slides showed cystic blood spaces, some of which were not lined by endothelial cells, others being of the capillary type associated with a loose fibroblastic benign stroma. These vessels seem to permeate the trabecular bone. Nevertheless, the bone trabeculae have reactive features, because they are delineated by active osteoblasts, a fact that does not sustain the osteosarcoma diagnosis. Random osteoclasts were also observed focally in apposition to the bone. “Blue-bone” was also present (Figures 2, 3 and 4). There was no abnormal osteoid deposition. Immunohistochemistry revealed: CD31 and ERG diffusely positive in the intertrabecular stroma (Figure 5), CD45 was positive in scattered inflammatory cells, Ki-67 low mitotic index (around 8%), MDM2 negative, SATB2 (Figure 6) and CD56 positive in osteoblastic bone rimming.
Our diagnosis, based on histological and immunohistochemical features, in correlation with clinical and imaging data, was aneurysmal bone cyst possibly secondary to a vascular malformation.
Discussion
The diagnosis of aneurysmal bone cyst can be challenging sometimes. In this case, the imaging data suggested four different histopathological diagnosis: Ewing sarcoma, eosinophilic granuloma, low-grade central osteosarcoma, or an osteoblastoma. One of these diagnostics – low-grade osteosarcoma – was expressed by a first histological examination of the biopsy. We proceeded to a new examination of the biopsy specimen and we discuss our findings and suggestions, taking into consideration, of course, all the clinical, imaging and histopathological available data of this case.
Based on the histopathological features, Ewing sarcoma and eosinophilic granuloma (Langerhans cell histiocytosis) were excluded.
Ewing sarcoma is a neoplasm affecting the bones and soft tissue, featuring a uniform population of “small round blue cells” that mainly affects children and young adults, nearly 80% of patients being less than 20 years old(3,4).
Eosinophilic granuloma (Langerhans cell histiocytosis) is a neoplastic proliferation of Langerhans cells most commonly affecting bones and adjacent soft tissue, and it presents as a solitary lesion or as a multisystem disease. Histologically, it presents as a proliferation of oval mononuclear large cells with eosinophilic cytoplasm and central ovoid, coffee bean-shaped or deeply idented nuclei, that can show mitotic figures without atypia, and interspersed inflammation, characteristically eosinophils, but other inflammatory cells may be variably present (lymphocytes, neutrophils or histiocytes)(3,4).
Low-grade central osteosarcoma (LGCOS) is a more challenging differential diagnosis, by its clinical, radiological and histological criteria. Being a well differentiated neoplasm, low osteosarcoma is histologically a more subtle lesion with few cellular atypia. It associates sometimes with secondary ABC. Histologically, LGCOS is characterized by mild to moderate cellular fascicles of bland spindle cells, intimately associated with long trabeculae or round islands of woven bone, which may have a pagetoid appearance(3,4). The bone trabeculae are usually parallel to each other, and not interconnected, and they are not rimmed by osteoclasts. There is also clear proof of osteoid formation. It also presents with an infiltrative grow pattern (proofs of infiltration of the tumor in preexisting bone)(3,4). The bland spindle shaped cells and vascular and even hemorrhagic stroma observed on H&E examination of the biopsy, as well as the presence of osteoblastic rimming in reactive new bone formation, “blue bone” type calcifications and focal aggregates of osteoclasts are more in accordance with a benign vascular lesion or osteoblastoma, or the association of both. Additional IHC showed that MDM2 was negative, and SATB2 was strictly positive in the osteoblasts rimming the reactive bone trabeculae (Figure 6).
Osteoblastoma clearly poses the greatest diagnostic challenge of the aforementioned differential diagnoses, because clinically, radiologically, as well as histologically, it has similar features as ABC. Osteoblastoma is a benign, locally aggressive bone-forming neoplasm that has a predilection for the spine and sacrum, and when located in tubular bones, it is mainly metaphyseal. Radiologically, it shows an expansile, usually well-defined but sometimes with poorly defined margins and expansion into adjacent soft tissue. One radiological difference with ABC is that osteoblastoma is a bone-forming lesion, while aneurysmal bone cyst is a lytic lesion of the bone. Histologically, this neoplasm is composed of haphazardly interconnecting trabeculae or sheet-like aggregates of woven bone rimmed by prominent active osteoblasts, with intertrabecular stromal tissue consisting of loose, richly vascular connective tissue often with extravasated erythrocytes. Diffusely scattered osteoclast-type giant cells are often present. Also, secondary ABC can occur in this type of lesion(3,8).
Coming back to our case and taking into account all the differential diagnoses discussed before, we excluded the diagnosis of LGCOS on histological and immunohistochemical grounds but, obviously, we retained the osteoblastoma radiological supposition with possible ABC-like changes. Even though the histologic data are essential and cannot be eluded the radiologic-histopathologic concordance, it is very important in bone pathology and should always be seriously taken into account.
We do not expect the complete surgical specimen analysis to change our histological diagnosis on the biopsy, osteoblastoma with ABC-like changes, but we are looking forward to thoroughly examine it, resection with clear margins being the treatment of choice in this case.
Conclusions
Vascular benign lesions of the bone – such as aneurysmal cyst of the bone, in our case – can be challenging on biopsies, even though the pathological tissue is not scanty. Biopsies are not able to encompass all possible histological features that can be seen in a heterogenous neoplasm. This is why radiologic-histological correlation is mandatory. Revising the whole case from the clinical, imaging and histological points of view is also necessary on the complete surgical specimen. Data regarding treatment and clinical evolution are contributing to definitive diagnosis, statistics and feedback on our previous histological observations.
Conflict of interest: none declared.
Financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.
Bibliografie
-
Mirra JM. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Philadelphia: Lea & Febiger; 1989.
-
Dabska M, Buraczewski J. Aneurysmal bone cyst. Pathology, clinical course and radiologic appearances. Cancer. 1969;23(2):371-389.
-
Nielsen GP, Rosenberg AE. Diagnostic Pathology: Bone. 3rd Edition. Elsevier, 2021.
-
WHO Classification of Tumors Editorial Board, World Health Organization. Soft Tissue and Bone Tumours. 5th Ed.; vol. 3. Lyon (France), 2020.
-
Devi P, Thimmarasa VB, Mehrotra V, Agarwal M. Aneurysmal bone cyst of the mandible: A case report and review of literature. Journal of Oral and Maxillofacial Pathology. 2011;15(1):105-108.
-
Capote-Moreno A, Acero J, García-Recuero I, Ruiz J, Serrano R, de Paz V. Giant aneurysmal bone cyst of the mandible with unusual presentation. Med Oral Patol Oral Cir Bucal. 2009;14(3):E137-E140.
-
Perrotti V, Rubini C, Fioroni M, Piattelli A. Solid aneurysmal bone cyst of the mandible. Int J Pediatr Otorhinolaryngol. 2004;68(10):1339-1344.
-
Limaiem F, Byerly DW, Mabrouk A, et al. Osteoblastoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.






