Factori de risc pentru pancreatita acută la copii
Risk factors for acute pancreatitis in children
Abstract
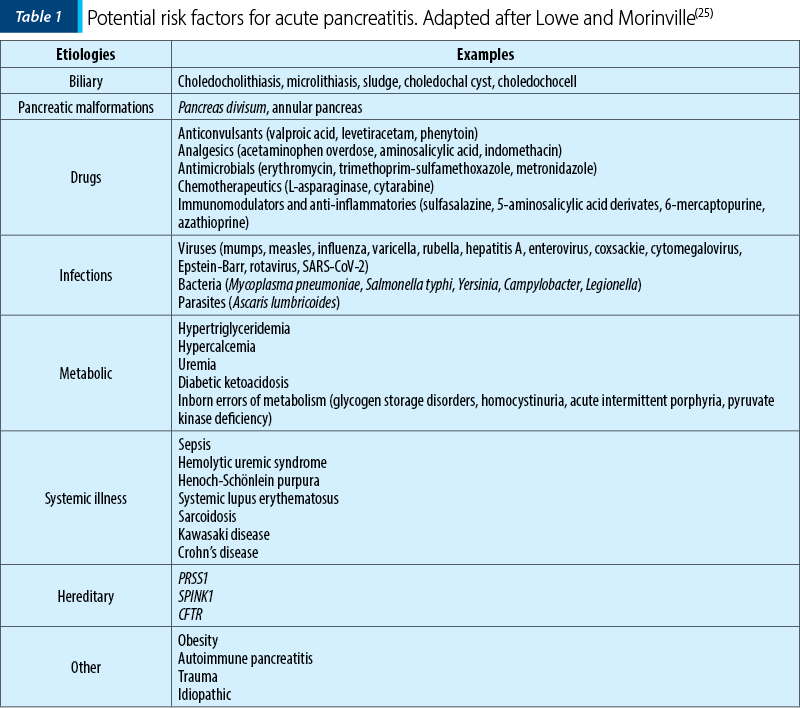
Acute pancreatitis (AP) is an acute inflammatory disease that must be taken into consideration in the differential diagnosis of abdominal pain in children, due to its unpredictable and in some cases severe evolution with systemic complications. The diagnosis is based on the clinical manifestations, laboratory tests and imaging modifications in children and adults, but the symptoms, evolution and prognosis often differ. In recent years, there has been an increasing interest in the identification of etiological factors associated with AP in children, given that they are different from those from the adult population. The main risk factors identified in acute pancreatitis in children are biliary tract pathology, pancreatic malformations, infections, systemic and metabolic diseases, drugs, traumatisms, geneticpredisposition, and idiopathic. In an important percentage of children, more than one risk factor is present. The identification of the etiological factors is important for a complete diagnosis but also for the follow-up and management of these patients, given the fact that some of the risk factors are associated with increased severity and others with recurrences and even evolution to chronic pancreatitis. Although important progress has been made recently, more data on children are needed for a better understanding and management
of acute pancreatitis.
Keywords
acute pancreatitisrisk factorschildrenRezumat
Pancreatita acută (PA) este o patologie inflamatorie care trebuie luată în considerare în diagnosticul diferenţial al durerii abdominale la copil, din cauza evoluţiei imprevizibile şi uneori severe, grevată de complicaţii sistemice importante. Diagnosticul se stabileşte pe baza manifestărilor clinice şi a modificărilor paraclinice şi imagistice, atât la adulţi, cât şi la copii, dar simptomele, evoluţia şi prognosticul sunt adesea diferite între cele două populaţii. În ultimii ani, s-a observat un interes crescut pentru identificarea factorilor etiologici în PA la copil, având în vedere că aceştia sunt diferiţi faţă de cei de la adulţi. Principalii factori de risc identificaţi la copil sunt patologia biliară, malformaţiile pancreatice, infecţiile, bolile sistemice şi metabolice, medicamentele, traumatismele, mutaţiile genetice şi formele idiopatice. Identificarea acestor factori este importantă, atât pentru un diagnostic complet, cât şi pentru prognosticul şi monitorizarea pacienţilor. Unii dintre aceşti factori se asociază cu o severitate crescută, dar şi cu apariţia episoadelor recurente şi a pancreatitei cronice. Deşi s-au făcut progrese importante în ultima perioadă, sunt necesare mai multe date pentru o înţelegere mai bună a pancreatitei acute la copil.Cuvinte Cheie
pancreatită acutăfactori de risccopiiIntroduction
Acute pancreatitis (AP) is represented by the acute inflammation of the pancreas that resolves completely after the attack is over, but it can be associated with important local and systemic complications(1). Acute pancreatitis has an increasing incidence in the last decade, reaching up to 13 cases per 100,000 children. This increase is partially due to early diagnosis and awareness from medical professionals(2).
For a positive diagnosis of AP, the fulfillment of the revised Atlanta criteria is needed. This requires two of the following three criteria: abdominal pain characteristic for AP, serum lipase or amylase values over three times the upper normal limit, or imaging findings characteristic for acute pancreatitis(3).
In contrast to pancreatitis in adults, in which the etiology is dominated by gallstones and alcohol, in children the etiological factors are more varied. Given this variety of etiologies and the fact that in approximately 20% of the children, more than one predisposing factor is present, it is now recommended to use the term risk factor, instead of etiology(4).
In this paper, we discuss the main risk factors involved in the onset of acute pancreatitis in children.
Risk factors for acute pancreatitis
1. Biliary disease
Biliary pancreatitis is one of the most important causes of acute pancreatitis, representing up to 30% of etiologies in some studies(5). Gallstone obstructs the choledochal duct or pancreatic duct, or both. The increased pressure secondary to obstruction is the trigger for the development of pancreatitis(6). In children, not only gallstones can trigger biliary pancreatitis, but also biliary tree malformations, like choledochal cysts and sludge. Although the causality between sludge/microlithiasis and pancreatitis has not been yet strongly demonstrated, the prevalence of sludge in biliary pancreatitis is estimated at approximately 30%(7). In most cases, biliary pancreatitis is associated with elevated liver enzymes and hyperbilirubinemia(7).
The management of biliary pancreatitis in children is similar to the one in adults. ERCP (endoscopic retrograde cholangiopancreatography) is recommended when available in the case of bile duct obstruction or microlithiasis. The timing of the intervention is recommended in the first 48 hours of admission if there are signs of obstructive jaundice or cholangitis(8). The treatment with choleretic medication (ursodeoxycholic acid) in the presence of sludge has been reported in some studies with good results, but there are not sufficient data for a strong recommendation(7).
2. Pancreatic malformations
The most common pancreatic malformation is pancreas divisum (PD). This malformation occurs when the ventral and dorsal ductal systems of the pancreas fail to fuse, in the second month of embryological development(9). There are two forms of PD, complete, in which the ventral and dorsal ducts drain separately in the duodenum, and the incomplete form, with a partial fusion of the ducts.
The role of PD in acute pancreatitis is controversial(10). Most of the patients with PD are asymptomatic. Until this moment, PD is considered a potential cofactor for the development of acute pancreatitis. The evidence for the involvement of PD in acute pancreatitis comes from the increased prevalence of this malformation in patients with acute recurrent episodes(11).
The management of these cases is conservatory in most cases. Surgery can represent an option in complicated and recurrent cases(11).
3. Drugs
The prevalence of drug-induced pancreatitis is less than 2% in the general population, but in children these numbers are higher, reaching up to 24%(12,13). Medication-related pancreatitis tends to be underreported due to the difficulty in establishing causality. In most cases, a rechallenge test with the suspected drug is missing, making it hard to determine if the drug was indeed the cause, a cofactor, or an incidental finding(12). Furthermore, in up to one-third of the cases in which drug-related pancreatitis is suspected, an additional risk factor is present(4).
There are several mechanisms for the development of medication-related pancreatitis, the most common being idiosyncratic reaction. Dose-dependent and genetic predisposition (HLA haplotypes) are less frequent(12,13).
The most common medications associated with pancreatitis are valproic acid, L-asparaginase, steroids, azathioprine, and levetiracetam(4,13).
The management of drug-induced pancreatitis consists of immediate interruption of the drug and supportive measures recommended in other forms of pancreatitis(12).
4. Infections
Infections are one of the most important causes of illness in children. Acute pancreatitis associated with infections represents approximately 10% of all cases(7). The strongest association is with mumps, in some cases pancreatitis manifesting without parotid gland enlargement(14). Other infectious agents that have been reported to be involved in AP are varicella, coxsackie B4, hepatitis A and E, rotavirus, adenovirus, measles, and Mycoplasma pneumoniae(5,7). Recently, SARS-CoV-2 infection but also multisystem inflammatory syndrome in children (MIS-C) have been associated with cases of acute pancreatitis(15,16).
The mechanism of pancreatic injury is either through the direct action of the infectious agent or through an immune response (as in the case of Mycoplasma-induced pancreatitis)(14). The diagnosis is established by temporal association of the symptoms of infection, laboratory analysis, and the lack of another risk factor(4).
The management of infectious AP consists of supportive treatment, both for the infection and pancreatitis.
5. Metabolic disorders
The most common metabolic disorders associated with acute pancreatitis are diabetic ketoacidosis, hypertriglyceridemia, hypercalcemia, and obesity. These pathologies represent up to 7% of the causes of acute pancreatitis(7).
Hypercalcemia (above 10.7 mg/dl total serum calcium) is a rare cause of AP. The most frequent causes of hypercalcemia-associated pancreatitis are primary hyperparathyroidism secondary to adenoma, malignancy-associated hypercalcemia, increased serum levels of vitamin D, familial hypocalciuric hypercalcemia, and parenteral nutrition(17).
-
Hypercalcemia causes increased intracellular calcium levels that can activate premature trypsinogen activation and NF-kB activation pathway, leading to acinar cell death and the initiation of the inflammatory response characteristic to AP(17).
Hypoalbuminemia is associated with severe pancreatitis; in these cases, calculating corrected total calcium levels or determining ionized calcium is the correct approach when investigating possible etiologies(12).
The management of hypercalcemia-induced pancreatitis includes the restriction of calcium intake, intravenous fluids for adequate renal perfusion and calcium elimination, and in some cases pharmacological options for calcium reduction (calcitonin, bisphosphonates, glucocorticoids) or parathyroidectomy(12,18).
-
Hypertriglyceridemia is another rare cause of AP in children. Recent data suggest that hypertriglyceridemia is a risk factor for more severe forms compared to other etiologies(19). The most common etiologies of hypertriglyceridemia-associated pancreatitis are primary hypertriglyceridemia (genetic defects of lipoprotein lipase, apolipoprotein C-II) or secondary causes of hypertriglyceridemia like diabetes ketoacidosis, non-alcoholic fatty liver disease, or type 1 glycogen storage disorders(12,19).
The serum triglyceride levels that increase the risk of AP are over the 95th percentile for age or 1000 mg/dl, although AP can develop at levels above 500 mg/dl(12,19).
The exact mechanism by which hypertriglyceridemia induces acute pancreatitis is not well understood. It is believed that pancreatic lipases metabolise the excess TG, leading to increased free fatty acids concentrations that aggregate and can cause ischemia and acinar cell damage. Additionally, chylomicrons can increase the serum viscosity, decreasing even more the blood flow to the pancreas(19).
The management of hypertriglyceridemia-associated pancreatitis in the acute phase consists of intravenous administration of dextrose and insulin, and in severe cases, plasmapheresis may be necessary(19). Long-term management includes dietary lifestyle intervention alongside pharmacotherapy (fibrates, omega-3 fatty acids)(19).
-
Obesity is considered an independent risk factor for developing AP in the adult population. Due to increased childhood overweight and obesity, this factor must be taken into consideration in the pediatric population also(20,21).
Obesity is associated with multiple metabolic disturbances, including hypertriglyceridemia, that can predispose to AP episodes, as stated before. Also, obesity is associated with a higher risk of severe forms through multiple mechanisms, one of the most important being the lipolyze of visceral fat by the leaked lipase, which leads to a systemic inflammatory response(21).
The management in the long term consists of lifestyle changes and weight loss.
6. Systemic diseases
Acute pancreatitis is often associated with a systemic disease. The most frequently associated diseases with AP are sepsis, hemolytic-uremic syndrome, lupus erythematous, and inflammatory bowel disease (IBD)(4,7). It is possible that the increase in the prevalence of pediatric AP is especially due to the increase of the forms associated with systemic diseases(7,22).
These forms require, besides the supportive measures, etiological treatment adequate to each cause.
7. Autoimmune pancreatitis
Autoimmune pancreatitis is a very rare entity in children, that can start as an acute episode. In adults, there are two distinct types of autoimmune pancreatitis: type 1, associated with the IgG4 spectrum of disease, and type 2 which is associated with IBD, whereas in children, autoimmune pancreatitis has features from both forms. Children with autoimmune pancreatitis are at a higher risk for developing other autoimmune or inflammatory disorders(23).
The positive diagnosis for autoimmune pancreatitis is through histopathological examination of the pancreatic tissues. In children, this is especially difficult, so we rely on imaging modifications (focal/ global enlargement of the pancreas) and in some cases, increased serum levels of IgG4(23).
Although there are insufficient data on the pediatric population, in symptomatic patients prednisone is recommended as the first line of treatment(23).
8. Hereditary
Hereditary pancreatitis can manifest as acute pancreatitis, representing approximately 8% of the causes, but it represents an important cause of recurrent and chronic pancreatitis. The main variants associated with AP are found in the cationic trypsinogen gene (PRSS1), the pancreatic secretory trypsin inhibitor gene (SPINK1), and the cystic fibrosis transmembrane regulator gene (CFTR)(7). PRSS1 variants may cause the secretion of a form of trypsinogen more susceptible to autoactivation. SPINK1 variant, on the other hand, is a loss of function variant, determining reduced inhibitor expression and compromise trypsin inhibition. CFTR variant is classically associated with cystic fibrosis, but milder variants with autosomal recessive transmission can cause AP by decreased bicarbonate secretion which leads to decreased liberation of zymogen and autodigestion(24).
Other variants recently associated with hereditary pancreatitis are CTRC (chymotrypsin C gene), CASR (plasma membrane calcium-sensing receptor), and CPA1 (carboxypeptidase A gene)(24).
9. Trauma
The most common causes of trauma-induced pancreatitis are bicycle handlebar injuries, motor vehicle crashes, sports injuries, accidental falls, non-accidental injury (child abuse), and iatrogenic injury (post-ERCP)(4,7). Trauma injuries should prompt emergency imaging investigation for the search of pancreatic duct disruption(4).
The management of these injuries can be conservative in mild cases or may require extensive surgical intervention.
10. Idiopathic
Even though there are a multitude of risk factors associated with acute pancreatitis in children, an important proportion of the cases remain without an identifiable risk factor. This percentage can go up to 30-35% of cases(4). Despite advances in the recognition and diagnosis of this pathology, the proportion of idiopathic pancreatitis is not decreasing(4). These numbers may go down, once other genetic mutations are discovered(7).
Conclusions
In children, identifying the risk factors associated with acute pancreatitis must be one of the main objectives from the first episode. Furthermore, these etiologies may impact the evolution and the subsequent follow-up of these patients, given the fact that some risk factors are strongly associated with recurrent episodes and progression to chronic pancreatitis. Pediatricians must be aware of these risk factors to be able to prevent an unfavorable outcome in children with acute pancreatitis, by early diagnosis and prompt intervention.
Funding: No funding to declare.
Corresponding author: Alina Grama E-mail: gramaalina 16@yahoo.com
Conflict of interest: none declared.
Financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.
Bibliografie
1. Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179-1187.e3.
2. Morinville VD, Barmada MM, Lowe ME. Increasing incidence of acute pancreatitis at an American pediatric tertiary care center: is greater awareness among physicians responsible?. Pancreas. 2010;39(1):5-8.
3. Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis - 2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102-111.
4. Husain SZ, Srinath AI. What’s unique about acute pancreatitis in children: risk factors, diagnosis and management. Nat Rev Gastroenterol Hepatol. 2017;14(6):366-372.
5. Mekitarian Filho E, Carvalho WB, Silva FD. Acute pancreatitis in pediatrics: a systematic review of the literature. J Pediatr (Rio J). 2012;88(2):101-114.
6. Wang GJ, Gao CF, Wei D, Wang C, Ding SQ. Acute pancreatitis: etiology and common pathogenesis. World J Gastroenterol. 2009;15(12):1427-1430.
7. Bai HX, Lowe ME, Husain SZ. What have we learned about acute pancreatitis in children?. J Pediatr Gastroenterol Nutr. 2011;52(3):262-270.
8. Abu-El-Haija M, Kumar S, Quiros JA, et al. Management of Acute Pancreatitis in the Pediatric Population: A Clinical Report From the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition Pancreas Committee. J Pediatr Gastroenterol Nutr. 2018;66(1):159-176.
9. V SK, Sangu P, C K, R P, Chidambaranathan S, Obla Lakshmanamoorthy NB. Congenital Anomalies of the Pancreas: Various Clinical Manifestations and Their Impact on Pancreatic Diseases and Outcomes. Cureus. 2022;14(8):e27915.
10. Thapa O, Basukala S, Shrestha M, et al. Acute recurrent pancreatitis in a child with pancreatic divisum - A case report. Ann Med Surg (Lond). 2022;82:104642.
11. Lin TK, Abu-El-Haija M, Nathan JD, et al. Pancreas Divisum in Pediatric Acute Recurrent and Chronic Pancreatitis: Report From INSPPIRE. J Clin Gastroenterol. 2019;53(6):e232-e238.
12. Husain SZ, Morinville V, Pohl J, et al. Toxic-metabolic Risk Factors in Pediatric Pancreatitis: Recommendations for Diagnosis, Management, and Future Research.
J Pediatr Gastroenterol Nutr. 2016;62(4):609-617.
13. Abu-El-Haija M, Hornung L, Lin TK, et al. Drug induced pancreatitis is the leading known cause of first attack acute pancreatitis in children. Pancreatology. 2020;20(6):1103-1108.
14. Suzuki M, Sai JK, Shimizu T. Acute pancreatitis in children and adolescents. World J Gastrointest Pathophysiol. 2014;5(4):416-426.
15. Nguyen HV, Brophy-Williams S. Acute pancreatitis in a child with SARS-CoV-2 infection. J Paediatr Child Health. 2022;58(11):2091-2092.
16. Acharyya BC, Dutta M, Meur S, Das D, Acharyya S. Acute Pancreatitis in COVID-
19-associated Multisystem Inflammatory Syndrome of Children - A Single Center Experience. JPGN Rep. 2021;3(1):e150.
17. Tiwari AK, Kumar V, Yadav DP, et al. Hypercalcemia - An enigmatic cause of acute pancreatitis. J Clin Transl Res. 2022;8(3):176-180.
18. Sadiq NM, Naganathan S, Badireddy M. Hypercalcemia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 4, 2023.
19. Grisham JM, Tran AH, Ellery K. Hypertriglyceridemia-induced acute pancreatitis in children: A mini-review. Front Pediatr. 2022;10:931336.
20. Kwak BO, Lee MJ, Park HW, Kim KS, Chung S. A case of recurrent acute pancreatitis in an obese child. Nutrition. 2014;30(10):1213-1216.
21. Navina S, Singh VP. Relationship between obesity and pancreatitis. Pancreapedia: Exocrine Pancreas Knowledge Base. 2015. doi: 10.3998/panc.2015.18.
22. Nydegger A, Heine RG, Ranuh R, Gegati-Levy R, Crameri J, Oliver MR. Changing incidence of acute pancreatitis: 10-year experience at the Royal Children’s Hospital, Melbourne. J Gastroenterol Hepatol. 2007;22(8):1313-1316.
23. Scheers I, Palermo JJ, Freedman S, et al. Recommendations for Diagnosis and Management of Autoimmune Pancreatitis in Childhood: Consensus From INSPPIRE. J Pediatr Gastroenterol Nutr. 2018;67(2):232-236.
24. Panchoo AV, VanNess GH, Rivera-Rivera E, Laborda TJ. Hereditary pancreatitis: An updated review in pediatrics. World J Clin Pediatr. 2022;11(1):27-37.
25. Lowe ME, Morinville VD. Chapter 23: Acute Pancreatitis in children. In The Pancreas: An Integrated Textbook of Basic Science, Medicine, and Surgery. 3rd Edition. John Wiley & Sons Ltd; 2018:219-229.





