Estimated to affect about 10% of women of reproductive age, endometriosis represents a debilitating disease. Endometriosis is characterized by endometrial tissue implants in extrauterine locations. Laparoscopy represents the gold standard for the diagnosis of endometriosis. Noninvasive diagnosis of endometriosis remains an interesting field for research. In our review, we describe and discuss the current status of biomarkers of endometriosis in plasma, urine, peritoneal fluid and endometrium.
Biomarkeri în endometrioză
Biomarkers in endometriosis
First published: 13 martie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.27.1.2020.2887
Abstract
Rezumat
Endometrioza reprezintă o boală debilitantă, estimându-se a afecta 10% dintre femeile la vârstă reproductivă. Endometrioza se caracterizează prin implanturi de ţesut endometrial în afara cavităţii uterine. Laparoscopia rămâne metoda de elecţie în diagnosticarea endometriozei. Diagnosticul neinvaziv al endometriozei reprezintă un subiect intens cercetat. După revizuirea literaturii, am descris statusul actual al biomarkerilor endometriozei din plasmă, urină, lichid peritoneal şi endometru.
Background
Endometriosis is a gynecological condition affecting commonly Caucasian women between 25 and 40 years of age, and is characterized by the presence of endometrial glands and stroma outside the uterine cavity(1). The ectopic endometrial tissue was described first in 1920s, nowadays affecting from 5% to 45% of the women of reproductive age and, moreover, up to 50% of infertile patients(2). Although the cause of endometriosis remains unclear, a few pathophysiological mechanisms are described, such as the retrograde peritoneal seeding of endometrial cells during normal menses, peritoneal epithelium metaplasia or peritoneal müllerian remnants growth(1).
Several studies associate reproductive factors and general factors with the risk of developing endometriosis. Parity, current oral contraceptive use, smoking, a higher Body Mass Index, regular exercise, and fish and omega 3 fatty acids seem to have a protective role. On the other hand, earlier age at menarche, shorter menstrual cycle length, taller height, alcohol use and caffeine intake were observed to increase the risk of endometriosis(3).
The most frequent pelvic areas for endometriosis are the peritoneum, the rectovaginal pouch and on the ovary, with specific lesions such as peritoneal implants, deep infiltrating endometriosis and ovarian endometrioma. The extrapelvic lesions were found on surgical scars on the peritoneum, the gastrointestinal and urinary tract, the thorax and even on the nasal mucosa(4). Therefore, typical symptoms for endometriosis include chronic pelvic pain, dyspareunia, dysmenorrhea and infertility. The ESHRE guideline: management of women with endometriosis (2014) underlines the long delay of 7 to 10 years in the diagnosis of endometriosis(2), because of the variability and nonspecific symptoms, which need a diagnostic laparoscopy. In fact, laparoscopy, with histological confirmation, is considered the gold standard in the diagnosis of endometriosis. Pelvic ultrasound is operator-dependent and shows limited specificity for superficial peritoneal lesions; transvaginal ultrasound can only identify deep nodules and ovarian endometriotic cysts(5). In order to improve the diagnosis and to reduce the period until treatment, several studies have carefully observed the need of noninvasive tests. Therefore, biomarkers that would precisely establish the diagnostic of endometriosis in a short time, irrespective of the stage of the disease, arrive as a natural progress of research in this field.
Types of biomarkers in endometriosis
For decades, several studies have researched the pathogenesis of endometriosis, and different biomarkers in blood, tissue and urine with potential use in the diagnosis were tested. The low statistical value and the inadequate specificity and sensitivity of biomarkers determined the actual guidelines for the management of women with endometriosis to not recommend any of them as standard approach.
The idea of studying biomarkers in endometriosis started as a need for accurate and efficient diagnosis in endometriosis, avoiding the long delay and the invasive gold standard method of diagnosis, laparoscopy. Endometriotic lesions activate various pathophysiological mechanisms, with the release of analytes, proteins, cells, microRNAs and other markers corresponding to the stage of the disease, but none of the markers have proven to be a definitive clinical tool for the diagnosis of endometriosis(3). Some of the pathophysiological mechanisms and the potential biomarkers are shown in Figure 1.
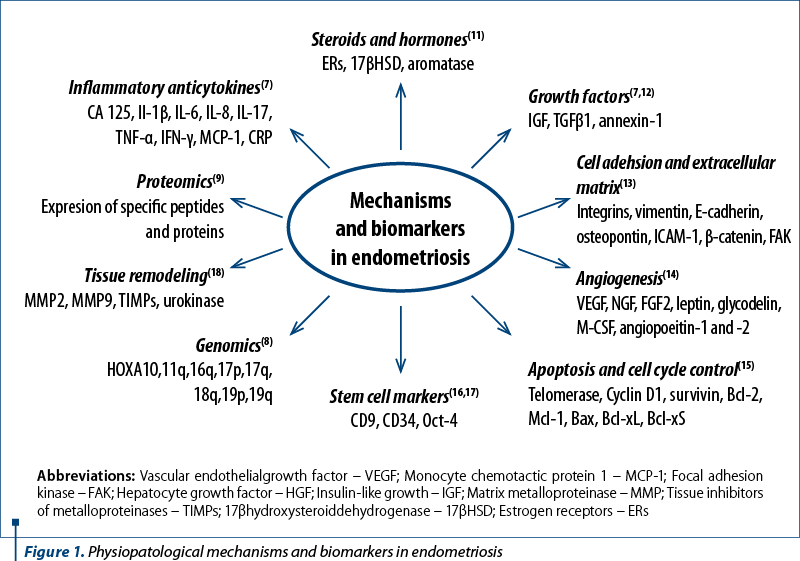
Ectopic endometrial tissue implants suffer the same cyclical histological changes similar to the uterine endometrium. Bleeding into the peritoneal cavity generates an inflammatory response, the activation of macrophages and the release of various cytokines and prostaglandins in peripheral blood and the peritoneal cavity. The cytokines activate different biological pathways and mechanisms, sending specific information to local cells and are released furthermore in the bloodstream to the entire organism. Each of the biomarkers described in Figure 1 were carefully researched, but the results regarding specificity, sensitivity and statistical value are uncertain. Thus, CA-125, a marker of peritoneal inflammation, is the most common endometriosis biomarker, with a mean sensitivity of 56% and a mean specificity of 91% in the meta-analysis by Nisenblat et al.(6) Thus, CA-125 seems to be hampered in its sensitivity, being elevated mainly in the advanced endometriosis stages, whilst its specificity is low because of its elevated level in other gynecological conditions. Similarly, various cytokines and inflammatory proteins, steroids, hormones and growth factors show high levels in advanced endometriosis stages, but this was not translated to any statistical significance(7). The level of hormones and inflammatory factors can induce epigenetic modifications of the genome by addition or removal of methyl groups, single-nucleotide polymorphism being associated with disease risk in endometriosis patients(8).
Studies regarding proteomics, protein or peptide fingerprints in peripheral blood and endometrium have shown promising results(9), but due to differences in analytical methods and the discrepancy between the level of gene expression in tissues and in blood, the results are limited. Sequencing and microarray technology allowed to observe the difference in endometrial gene expression between women with or without endometriosis, but there is still a need of further research of the potential use of circulating miRNA as a diagnostic marker for endometriosis(10).
The number of biomarkers studied in association with endometriotic lesions is significantly high, but the potential role in the diagnosis of endometriosis remains uncertain. Currently, the sensitivity and specificity of these biomarkers are low, with the possibility to identify advanced stages of endometriosis, but with the difficulty to differentiate them from other gynecological conditions. Only systematic research of biomarkers in a large cohort can set the diagnostic principles of endometriosis.
Discussion and conclusions
Although endometriosis, a complex gynecological condition, is frequently met in the population of women of reproductive age, the disorder shows an enigmatic etiology, with reduced and invasive diagnostic methods and less efficient therapeutic approaches. The study of biomarkers in endometriosis needs more research and the understanding of the disease-specific molecular pathways and, probably, future new therapeutic and diagnostic procedures will follow. Laparoscopy with histological confirmation remains the gold standard method of diagnosis in endometriosis, and although it is accurate, it is still an invasive method and adds additional procedure risks, surgical or anesthesia side effects and possible complications. In order to avoid these, semi-invasive methods should be developed to screen specific endometriosis markers in blood, peritoneal fluid or tissues sample.
Traditional inflammatory cytokines, steroids, hormones and growth factors were carefully observed in the development of endometriotic lesions, as well as future diagnostic biomarkers. The increased levels of such markers in ectopic endometriotic locations, blood/peritoneal fluid tests are not specific, as shown before, because these are elevated in other gynecological or general diseases, as well. Therefore, instead of a single biomarker, research seems to suggest that a group of biomarkers, or a biomarker panel, could be more useful in the pathway of diagnosis in endometriosis, with higher sensitivity and specificity. The biomarker panel could discriminate not only between endometriosis and other gynecological diseases, but could also identify the specific stage of endometriosis, especially the mild and moderate ones. Furthermore, depending on the severity of the lesions, the same biomarker panel could be the cornerstone to new strategies of target therapy.
Another future perspective comes from the new multiplex immunoassay and technologies that can identify pathophysiological molecular fingerprints, circulating and tissue miRNA, used as noninvasive or minimally invasive biomarkers for endometriosis. These strategies require special medical equipment and specific staff training, but if identified, these molecular findings of the genome and proteome could become a revolutionary step in diagnosis and could create a pattern in the individual’s genetic code, specific gene expression and regulation.
In spite of a wide biomarkers variety and plethora of research, the current guidelines on the management of endometriosis do not recommend reliable diagnostic biomarkers. This stressess out the need for extensive research to find out noninvasive diagnosis tools for endometriosis.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
- Missmer S, Hankinson S, Spiegelman D, et al. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004; 160(8):784-96.
- Dunselman G, Vermeulen N, Becker C, et al. ESHRE guidline: management of women with endometriosis. Human Reprod. 2014; 29(3):400-12.
- Parasar P, Ozcan P, Terry K. Endometriosis: Epidemiology, diagnosis and clinical management. Curr Obstet Gynecol Rep. 2017; 6(1):34-41.
- Machairiotis N, Stylianaki A, Dryllis G, et al. Extrapelvic endometriosis: a rare entity or an underdiagnosed condition. Diagn Pathol. 2013; 8:194.
- Hsu A, Khachikyan I, Stratton P. Invasive and noninvasive methods for the diagnosis of endometriosis. Clin Obstet Gynecol. 2010; 53(2):413-9.
- Nisenblat V, Bossuyt P, Shaikh R, et al. Blood biomarkers for the noninvasive diagnosis of endometriosis. Cochrane Database Syst Rev. 2016; 5:CD012179.
- May K, Villar J, Kennedy S, et al. Endometrial alterations in endometriosis: a systematic review of putative biomarkers. Hum Reprod Update. 2011; 17(5):637-53.
- Painter J, Anderson C, Nyholt D, et al. Genome-wide association study identifies a locus at 7p15.2 associated with endometriosis. Nat Genet. 2011; 43:51-4.
- Browne A, Yu J, Huang R, et al. Proteomic identification of neurotrophins in the eutopic endometrium of women with endometriosis. Fertil Steril. 2012; 98(3):713-9.
- Ahn S, Singh V, Tayade C. Biomarkers in endometriosis: challenges and opportunities. Fertil Steril. 2017; 107(3):523-32.
- Pan Q, Luo X, Toloubeydokhti T, et al. The expression profile of micro-RNA in endometrium and endometriosis and the influence of ovarian steroids in their expression. Mol Hum Reprod. 2007; 13(11):797-806.
- Othman E, Hornung D, Al-Hendy A. Biomarkers of endometriosis. Expert Opin Med Diagn. 2008; 2(7):741-52.
- Lessey B, Young S. Integrins and other cell adhesion molecules in endometrium and endometriosis. Semin Reprod Endocrinol. 1997; 15(3):291-9.
- Becker C, D Amato R. Angiogenesis and antiangiogenic therapy in endometriosis. Microvasc Res. 2007; 74(2-3):121-30.
- Kyama C, Mihalyi A, Gevaert O, et al. Evaluation of endometrial biomarkers for semi-invasive diagnosis of endometriosis. Fertil Steril. 2011; 95(4):1338-43.
- Du H, Taylor H. Contribution of bone marrow-derived stem cells to endometrium and endometriosis. Stem Cells. 2007; 25(8):2082-6.
- Tai M, Chang C, Kiupel M, et al. Oct4 expression in adult human stem cells: evidence in support of the stem cell theory of carcinogenesis. Carcinogenesis. 2005; 26(2):495-502.
- Yang H, Liu J, Fan Y, et al. Associations between various possible promoter polymorphisms of MMPs genes and endometriosis risk: a metaanalysis. Eur J Obstet Gynecol Reprod Biol. 2016; 205:174-88.
Articole din ediţiile anterioare
Prezervarea fertilităţii la o pacientă cu polifibromatoză uterină şi endometrioză ovariană. Prezentare de caz
Polifibromatoza uterină este o patologie frecventă, ale cărei diagnostic şi tratament sunt foarte bine documentate, existând numeroase ghiduri elab...
Diagnosticul imagistic al endometriozei profund infiltrative
Endometrioza profund infiltrativă (EPI) reprezintă, prin definiţie, infiltrarea implanturilor endometriozice în profunzime mai mult de 5 mm de l...
Statutul actual şi indicaţiile chirurgiei robotice în cadrul intervenţiilor ginecologice benigne şi maligne
Chirurgia robotică a câştigat teren în ultimii ani în cadrul intervenţiilor ginecologice benigne şi maligne. Scopul acestui articol este de a preze...
Endometrioza extragenitală - cicatrice post-miomectomie. Prezentare de caz
Endometrioza extragenitală este o afecţiune rară. Posibilele localizări sunt, în ordinea frecvenţei, la nivelul peretelui abdominal, al intestinulu...