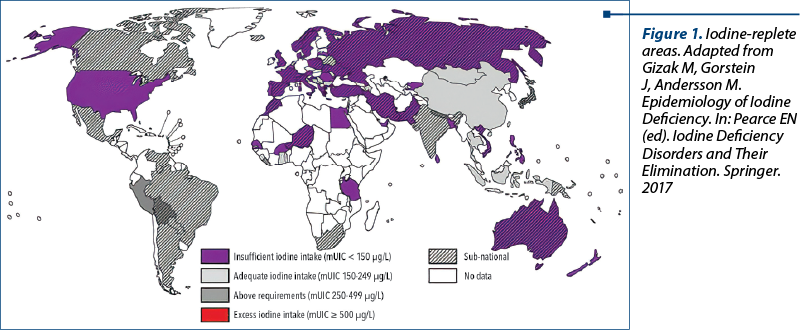
Hypothyroidism is the most common gestational endocrine disease. Globally, the most common cause for hypothyroidism is iodine deficiency. Other causes include: genetic variations that are responsible for TSH variations, prior thyroidectomy or ablative radioiodine therapy, whereas secondary (pituitary) and tertiary (hypothalamic) causes are rare. Most international guidelines suggest targeted thyroid testing in pregnant women with risk factors for thyroid insufficiency, such as living in iodine-replete areas.
Constatări ultrasonografice ale hipotiroidismului în timpul sarcinii
Ultrasound findings of hypothyroidism during pregnancy
First published: 12 decembrie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.26.4.2019.2704
Abstract
Rezumat
Hipotiroidismul este cea mai frecventă patologie endocrină care apare în timpul sarcinii. La nivel global, cel mai des întâlnită cauză pentru hipotiroidism este deficitul de iod. Alte cauze includ: mutaţii genetice responsabile de variaţii ale TSH-ului, tiroidectomie în antecedente sau radioterapia ablativă, în timp ce hipotiroidismul secundar şi cel terţiar sunt rar întâlnite. Majoritatea ghidurilor internaţionale sugerează testarea tiroidiană ţintită a gravidelor care asociază factori de risc, precum cele care trăiesc în zone sărace în iod.
Introduction
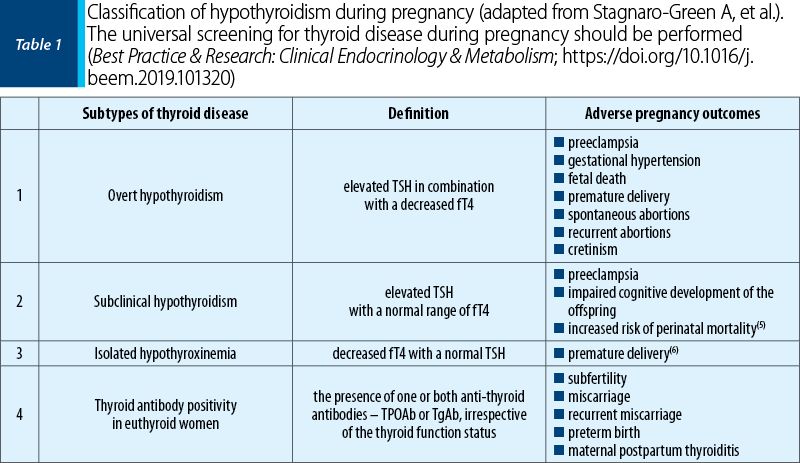
In iodine-replete areas (Figure 1), the prevalence of spontaneous hypothyroidism is between 1% and 2% (about 10 times more common in women than in men)(3). The epidemiological data suggest that the children of women with low levels of free T4 may have psychoneurological deficits(4) (Table 1). In classic areas of iodine deficiency, a similar range of deficits in children has been described, where maternal hypothyroxinaemia rather than high serum TSH was the main biochemical abnormality(10). Even in areas previously thought to be iodine sufficient, there is now evidence of substantial gestational iodine deficiency, which may lead to low maternal circulating T4 concentrations. In addition to the childhood neuropsychological problems relating to low T4 values, there is evidence that maternal TPOAb may result in intellectual impairment even when there is normal thyroid function(4).
Ultrasonography as a screening tool has a high sensitivity and will result in findings that are common and rarely have pathological significance(8).
The thyroid gland during pregnancy
During pregnancy, the production of T4 and T3 hormones increases by 50%, which leads to an increase of 50% in the iodine requirement(11). Also, there is a rise in the levels of TBG, resulting in lower levels of free T4 and a feedback stimulation of the thyroid gland. Due to the similarities in the chemical structure of TSH and hCG glycoprotein, the high levels of hCG in maternal blood during early pregnancy stimulate furthermore the thyroid gland(3).
Fifty percent of pregnant women are estimated to be positive for thyroid autoantibodies, indicating an underlying chronic autoimmune thyroiditis such as Hashimoto’s thyroiditis, TPOAb being the most sensitive and specific autoantibodies. In these cases, the immunosuppression of the pregnancy results in a marked decrease in thyroid antibodies titer. In the postpartum, however, there is a rapid return to the pre-pregnancy thyroxine and triiodothyronine levels, with an increase of thyroid antibodies – often to a higher titer than the one present in the first trimester(2).
Ultrasound aspects of hypothyroidism
The ultrasound examination of the thyroid gland does not require prior patient’s preparation; it should be preceded by a clinical consultation of the neck region, following the symmetry, dimensions of the gland, as well as the presence of cervical adenopathies.
The use of ultrasound examination of the thyroid gland refers to the most accurate measurement of the thyroid volume, hence providing the early diagnosis of diffuse pathologies and the detection and characterization of nodular lesions. Determining the volume of the thyroid is one of the most common purposes for which it is resorted to thyroid ultrasound, the hypertrophy of the thyroid gland being the most common thyroid pathology in our geographical area.
Regarding the diagnosis of diffuse thyroid diseases, thyroiditis is in the first place. In acute and subacute thyroiditis, the clinical picture is suggestive of the diagnosis, the importance of ultrasound being in monitoring the evolution of the disease under treatment.
In acute thyroiditis, the ultrasound of the gland highlights hypertrophy with multiple hypoechogenic areas, imprecisely delimited, which may evolve under treatment to remission or may evolve into abscess, needing surgical drainage – spontaneous fistulation to mediastinum is to be avoided during pregnancy.
In subacute thyroiditis, the ultrasound aspect is homogeneous, hypoecogenic hypertrophy. Under treatment (corticosteroid), it can evolve with healing – return to the isoecogenic aspect, or persistence of hypoecogenic areas that show the continuation of the inflammatory process.
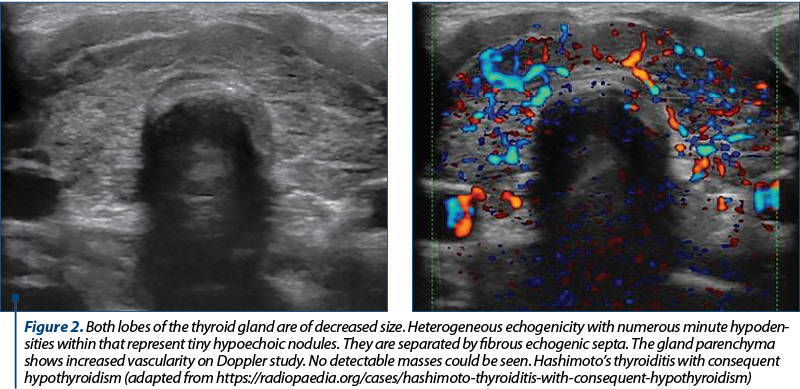
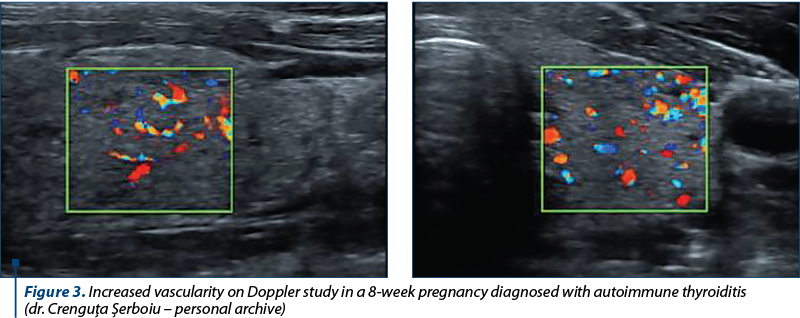
In chronic thyroiditis (Hashimoto’s lymphocytic thyroiditis), the contribution of the ultrasound is major, especially due to the very poor clinical picture. The ultrasound aspect is suggestive: diffuse hypertrophy of the gland, polycyclic contour, micronodular structure (nodules between 1 mm and 5 mm in diameter – “painted” appearance) and hypoecogenic. Also, there is evidence of calcifications and increased vascularization, a pseudolobulated aspect through the development of fibrous septa. The confirmation of the diagnosis is made by determining TPOAb and thyroid hormones, Hashimoto’s thyroiditis being an autoimmune disease(7).
Materials and method
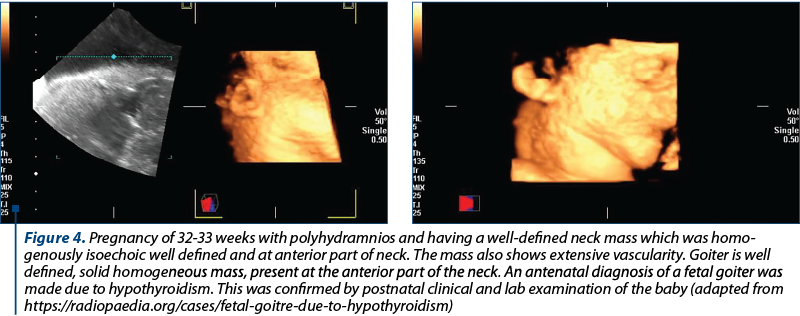
In a retrospective analysis of the cases admitted in the Department of Obstetrics and Gynecology of the Bucharest Emergency University Hospital, from January 2015 up to September 2019, we identified a number of 186 pregnancies marked by hypothyroidism and 11 cases with hyperthyroidism (Figure 5).
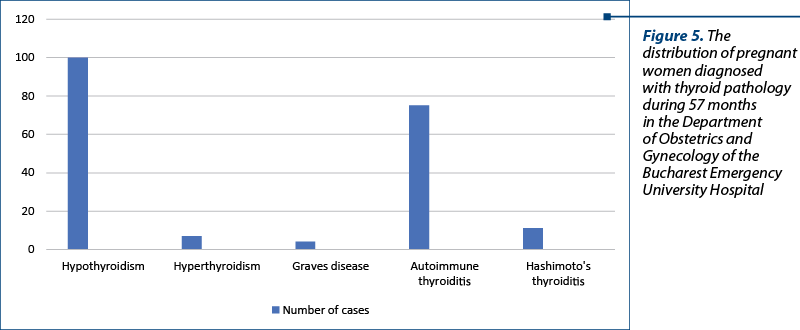
Fourteen cases of hypothyroidism also associated hereditary thrombophilia, compared to 21 cases of autoimmune thyroiditis and two cases of Hashimoto’s lymphocytic thyroiditis.
Discussion
The national societies of endocrinologists, obstetricians and gynecologists, as well as governmental agencies have weighed in on the debate of universal screening for thyroid disease in pregnancy, with opinions varying from society to society, country to country, year to year, and even within societies(2). In 2014, the European Thyroid Association (ETA) published a guideline, recommending universal screening for overt hypothyroidism. However, this recommendation was not unanimous, with two of the six authors dissenting(7). The obstetrical societies recommend targeted instead of universal screening. In 2015, the Practice Bulletin of The American College of Obstetricians and Gynecologists (ACOG) recommended for targeted screening and against universal screening in pregnant women(8).
Conclusions
Thyroid ultrasound (TUS) is an optimal initial imaging tool used in the evaluation of hypothyroid disorders because it is noninvasive, available and doesn’t use any radiation. It is widely used in the diagnostic workup of thyroid dysfunction. In a hypothyroid patient, TUS may lead to cost savings: if a typical autoimmune pattern is present on TUS, the measurement of antithyroid antibodies will not be necessary for the diagnosis of Hashimoto’s thyroiditis. TUS in these circumstances is especially valuable in case of women who wish to conceive or are pregnant.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
- Abalovich M, Amino N, Barbour LA, Cobin RH, De Groot LJ, Glinoer D, et al. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2007; 92(8 Suppl):S1-47.
- Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017; 27:315-89.
- Walsh JP. Managing thyroid disease in general practice. Med J Aust. 2016; 205:179-84.
- Flynn RV, MacDonald TM, Morris AD, et al. The thyroid epidemiology, audit and research study; thyroid dysfunction in the general population. J Clin Endocrinol Metab. 2004; 89:3879–84.
- Van den Boogaard E, Vissenberg R, Land JA, van Wely M, van der Post JA, Goddijn M, et al. Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy: a systematic review. Hum Reprod Update. 2011; 17(5):605-19.
- Korevaar TI, Schalekamp-Timmermans S, de Rijke YB, Visser WE, Visser W, de Muinck Keizer-Schrama SM, et al. Hypothyroxinemia and TPO antibody positivity are risk factors for premature delivery: the generation R study. J Clin Endocrinol Metab. 2013; 98(11):4382-90.
- Lazarus J, Brown RS, Daumerie, et al. 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J. 2014; 3:76-94.
- ACOG. Practice Bulletin no. 148: Thyroid disease in pregnancy. Obstet Gynecol. 2015; 125:996-1005.
- Surks MI, Ortiz E, Daniels GH et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. 2004; 291:228–38.
- Knudsen N, Jørgensen T, Rasmussen S et al. The prevalence of thyroid dysfunction in a population with borderline iodine deficiency. Clin Endocrinol (Oxf). 1999; 51:361–67.
- Biondi B, Cooper DC. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008; 29:76–131.
Articole din ediţiile anterioare
Adenomioza – algoritm de diagnostic, tratament şi implicaţii obstetricale
Adenomioza continuă să fie o provocare pentru ginecologi, deşi posibilităţile de diagnostic au progresat foarte mult. Tehnicile imagistice moderne ...
A rare case of complete hydatidiform mole with prolonged evolution – clinical case
Mola hidatiformă, cunoscută drept sarcină molară, reprezintă o boală gestaţională trofoblastică cu punct de plecare placentar şi capacitate de meta...
Managementul ante-, peri- şi postnatal al unei gravide cu histiocitoză pulmonară cu celule Langerhans - prezentare de caz
Histiocitozele cu celule Langerhans sunt un grup de patologii rare produse prin proliferarea clonală a celulelor dendritice Langerhans, care pot af...
Complicaţii materne şi neonatale în sarcina gemelară obţinută spontan versus sarcina gemelară obţinută prin FIV
Acest studiu a avut ca obiectiv identificarea complicaţiilor materne şi neonatale din sarcina gemelară obţinută spontan, comparativ cu sarcina gem...