Introduction. Gestational trophoblastic neoplasia (GTN) represents a generic term that includes invasive mole (IM), choriocarcinoma (CCA), placental site trophoblastic tumor (PSTT) and epithelioid trophoblastic tumor (ETT).
Case report. In this paper we report the case of a 40-year-old woman, gesta 2, para 2, presenting with a cervical well vascularized mass causing vaginal bleeding two years after the delivery of her second baby at term by caesarean section. The cervical CCA suspicion diagnosis was established based on imaging aspect - transvaginal ultrasound showing a parenchymatous area that protrudes into the cervical canal with intense peripheral vascular network and contrast-enhanced MRI describing an expansive bulky, round-oval, well defined mass with a long necrotic pedicle and extensive central area of necrosis. For the differential diagnosis it was recommended the dosage of serum βHCG, which showed a very high value of 63291 mUI/mL. The histopathological results correlated with the increased levels of βHCG suggested choriocarcinoma with large necrotic and hemorrhagic areas. Accurate positive diagnosis of CCA was realized through immunohistochemistry evaluation (IHC), the AE1-AE3 markers, βHCG, HPL, MUC4 and Ki-67 diffusely positive in tumor cells. A trachelectomy was performed, followed by abdominal uterine cerclage, in order to preserve the patient’s ability to carry a future pregnancy until term.
Discussions. Usually, the diagnosis of a primary extrauterine CCA is difficult because of the non-specific clinical presentation that can mimic other conditions.
Conclusions. Primary cervical choriocarcinoma is an extremely rare condition that should be considered in the differential diagnosis of a cervical mass with profuse bleeding particularly due to intense vascularity, especially in young women. Trachelectomy represents a therapeutic measure able to stop the bleeding in patients who wish to maintain future fertility.
Coriocarcinom primar al colului uterin mimând o sarcină cervicală
Primary choriocarcinoma of the cervix mimicking a cervical pregnancy
First published: 15 martie 2016
Editorial Group: MEDICHUB MEDIA
Abstract
Rezumat
Introducere. Neoplazia trofoblastică gestaţională (NGT) reprezintă un termen generic care include mola invazivă (IM), coriocarcinomul (CCA), tumorile trofoblastice de situs placentar (PSTT) şi tumorile trofoblastice epitelioide (ETT).
Prezentare de caz. În această lucrare am raportat cazul unei paciente, în vârstă de 40 de ani, secundigestă, secundipară, care prezintă o formaţiune tumorală bine vascularizată la nivelul colui uterin, cauzatoare de sângerari vaginale debutate la doi ani de la naşterea celui de-al doilea copil, prin operaţie cezariană. Diagnosticul de suspiciune de CCA cervicală a fost stabilit pe baza aspectului imagistic - ecografia transvaginală arată o masă parenchimatoasă care protruzionează în canalul cervical cu reţea vasculară periferică intensă, iar IRM cu substanţă de contrast descrie un proces expansiv voluminos, rotund-ovalar, bine definit, cu pedicul lung necrotic şi zonă centrală extinsă de necroză. Pentru diagnosticul diferenţial se recomandă dozarea βHCG seric, care a evidenţiat o valoare foarte mare, de 63291 mUI/ml. Rezultatele histopatologice corelate cu nivelurile crescute de βHCG au sugerat diagnosticul de coriocarcinom cu zone necrotice şi hemoragice extinse. Diagnosticul pozitiv de CCA a fost realizat prin evaluarea imunohistochimică (IHC), markerii AE1-AE3, βHCG, HPL, MUC4 şi Ki-67 fiind întâlniţi difuz pozitivi în celulele tumorale. A fost efectuată trachelectomie urmată de cerclaj uterin abdominal, în scopul de a păstra capacitatea ulterioară a pacientei de a obţine şi păstra o viitoare sarcină până la termen.
Discuţii. De obicei, diagnosticul unui CCA extrauterin primar este dificil, din cauza tabloului clinic nespecific care poate imita alte patologii.
Concluzii. Coriocarcinomul primar al colului uterin este o condiţie extrem de rară, care ar trebui luată în considerare în diagnosticul diferenţial al unei formaţiuni de col uterin cu sângerare abundentă, în special din cauza vascularizaţiei intense, mai ales la femeile tinere. Trachelectomia reprezintă o atitudine terapeutică în măsură să oprească sângerarea la pacientele care doresc să îşi menţină fertilitatea ulterioară.
Introduction
Gestational trophoblastic neoplasia (GTN) represents a generic term that includes a variety of malignant pathologies, the common link between them being the uniqueness of their physiopathology, as the maternal characteristic lesions arise only from fetal tissues(1). The heterogenic lesions with origin in the abnormal proliferation of the trophoblast include invasive mole (IM), choriocarcinoma (CCA), placental site trophoblastic tumor (PSTT) and epithelioid trophoblastic tumor (ETT). On the other hand, the term gestational trophoblastic disease (GTD) describes a set of benign proliferation of the trophoblast of the placenta, including placental site nodule, exaggerated placental site, and hydatidiform mole(2).
Gestational trophoblastic disease (GTN) has an incidence of 0.6 to 2/1,000 pregnancies worldwide nowadays. It has a recurrence risk of around 1% after a molar pregnancy(3). Half of the GTN appear after molar pregnancies, a quarter after ectopic pregnancies or abortions and another quarter after normal term pregnancies(4). As a particular aspect though, PSTT and ETT occur after term pregnancies or non-molar abortions in 95% of the cases. The period of time between the last pregnancy of any type and the appearance of CCA is described in very wide range, from a few months up to 15 years(5). Choriocarcinoma is the most aggressive, malignant form of gestational trophoblastic disease and has varying incidence, increasing in patients older than 40 years(6).
Apparently, IM and CCA arise from the abnormal proliferation of the chorionic villi, while PSTTA and ETT arise from the extravillous trophoblast. Both IM and CCA usually respond to chemotherapy, as the cure rates show a level of over 90%, which is a positive aspect because they are the most common forms of GTN(7). They are associated with high levels of the beta subunit of the human chorionic gonadotropin (bHCG), and frequently need monochemotherapy, usually using methotrexate or actinomycin D. On the other hand, the more rare cases of PSTT and ETT express low levels of bHCG and are relatively resistant to chemotherapy, multiagent treatment which combines etoposide, methotrexate, actinomycin D, cyclophosphamide and vincristine being necessary, but in these cases the first line of treatment is surgery, especially in non-metastatic cases(8).
In this paper we report the case of a 40-year-old woman, gesta 2, para 2, presenting with a cervical well vascularized mass causing vaginal bleeding two years after the delivery of her second baby at term by cesarean section.
Case report
The 40-year-old Caucasian patient had an obstetrical history of two term deliveries by caesarean section in 2011, respectively 2013. She presented in June 2015 at the gynecologist accusing irregular vaginal bleeding with reduced to moderate flow, after her last normal period in 20 May. The local exam showed normal external genital organs and reduced metrorhagia with a normal cervical aspect at the speculum exam. The vaginal tact revealed though an enlarged cervix, with a diameter of 6 centimeters, regulated surface and reduced consistency with a normal uterine dimension and mobility and normal adnexal areas.
A transvaginal ultrasound was then performed, which described normal ovaries and at the level of the uterine isthmus in the posterior uterine wall a parenchymatous area with a diameter of 5 centimeters, which protrudes into the inferior third of the uterine cavity and the superior cervical cavity with peripheral vascular network in direct contact with the urinary bladder. According to the clinical examination findings and the ultrasound aspect, the diagnostic suspicion of uterine leiomyoma is raised. Magnetic resonance imaging with contrast substance is recommended in order to establish the extent and particularities of the cervical tumor.
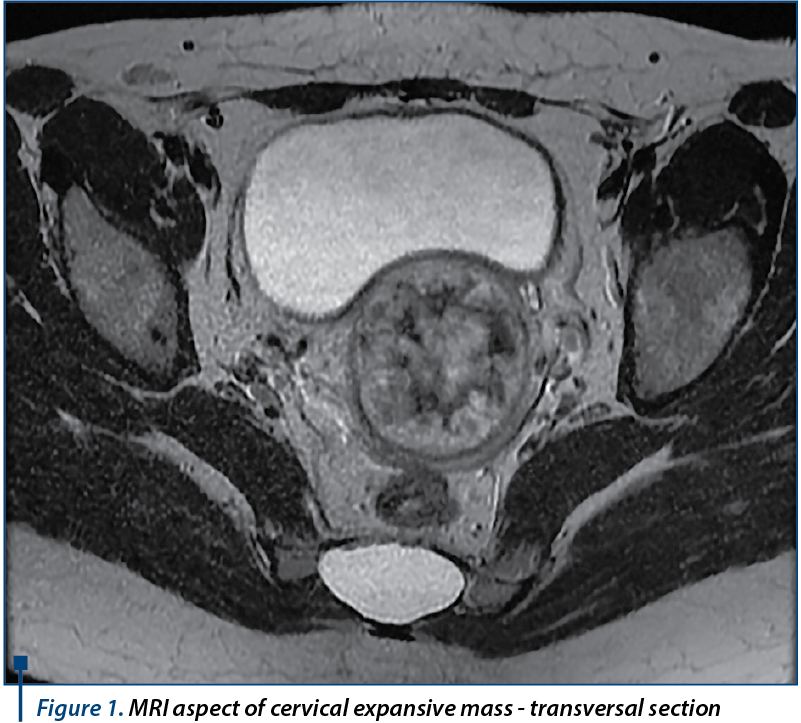
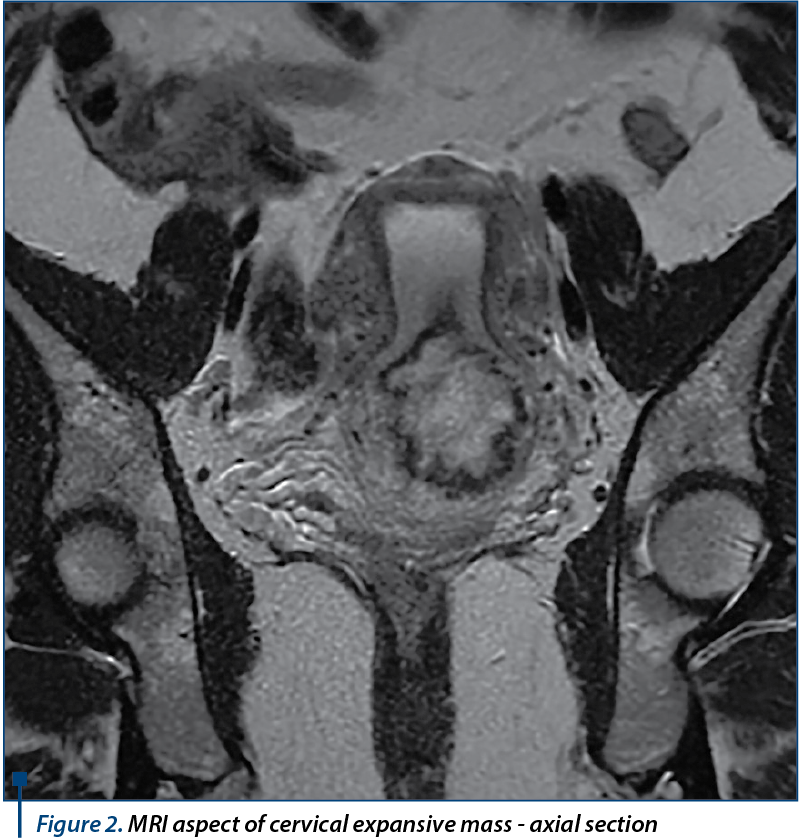
MRI showed normal dimension uterus in intermediate position, with normal myometrial thickness presenting several intramural and subserosal leiomyomas on the anterior wall, the largest of 12 millimeters in diameter; at the level of the posterior uterine wall origins an expansive corporeal originated bulky, round-oval, well defined mass, of approximatively 58/57/53 millimeters, which shows a long pedicle with a diameter of approximately 14 millimeters and 20 millimeters length that protrudes into the cervical cavity, which is completely occupied and expanded; it completely obstructs the cervix, with secondary accumulation of parafluid - hematic content into the uterine cavity. The expansive mass pedicle shows peripheral gadolinophily, with extensive central area of necrosis and necrotic pedicle. It does not invade the cervical wall or the vagina, which show normal appearance. Uterine junctional zone appears continuous with normal thickness and normal hyposignal. The ovaries and the rest of abdominal pelvic organs appeared normal, with no lymph nodes involvement, ascites, abdominopelvic collections or bone lesions with secondary character in the examined segments. The conclusion of the contrast MRI exam was the presence of a bulky pediculate mass developed within the uterine cavity, locally noninvasive (junctional zone, cervix), which obstructs and protrudes in the cervical cavity - MRI appearance suggests a cervical pregnancy, an endometrial polyp or a submucosal pediculate leiomyoma (Figures 1, 2, 3).

For the differential diagnosis it is recommended the dosage of serum bHCG, which shows a very high value of 63291 mUI/mL on 11 June. This paraclinical finding brings into attention the diagnosis of primary cervical choriocarcinoma, according to its location. The surgical excision of the tumor is decided, given the fact that no secondary lesions have been found. Distance dissemination, which occurs on hematogeous way most frequently in cases of choriocarcinoma as it is a highly vascularized tumor, has been investigated in our case with chest X-ray and contrast enhanced abdomen and pelvis MRI. Pulmonary X-ray showed no sign of metastasis, while abdomen MRI described normal ovaries, urinary bladder, rectum, sigmoid, liver, spleen, pancreas and kidneys with no abdominal lymph node involvement and no sign of ascites, collections or secondary bone lesions. Given the fact that no sign of metastasis was found, on 16 June an exploratory laparotomy is performed, with the finding of a slightly enlarged uterus with a much increased cervix, with a diameter of 7-8 centimeters and macroscopically normal adnexa. A trachelectomy was practiced with an extemporaneous exam of the excised cervix, which showed polypoid tumor formation with a diameter of 4/4 centimeters, soft texture, spongy appearance on sectioning with massive hemorrhage and fibrous cervical wall which shows in the surface polypoid hemorrhagic proliferation that seems to interest the wall.
The histopathological extemporaneous exam had an uncertain result, showing fragments of wide necrotic hemorrhagic area with chronic inflammation and the presence of pleomorphic cells, hyperchrome atypical cervical wall with fibro-conjunctive structure showing tumor infiltrates with high malignancy suspicion and haemorrhagic areas. Thus, the high suspicion of malignancy called for the certainty paraffin exam. After that, an abdominal uterine cerclage was performed and the bHCG repeated. Its value on the first postoperative day dropped significantly, being 14808 mUI/mL, and continued to drop the following day - 9001 mUI/mL.
The paraffin exam described malignant proliferation of trophoblastic cell made up of pleomorphic confounding cyto and syncytiotrophoblast cells and intermediate trophoblast cells, with hyperchromic nuclei that separate vascular spaces and have trabecular disposition infiltrating the cervical wall until near the endocervical lining. Bizarre intermediate trophoblast cells, some multinucleated, were present, as well as large areas of intratumoral and peritumoral hemorrhage and necrosis and chronic inflammation and bleeding at the level of the endocervical mucosa.
The cervix presented acanthosis, parakeratosis and subepithelial chronic inflammation, the tumor proliferation interesting the smooth muscle, while chorionic villi were absent. The histopathological results correlated with the increased levels of bHCG suggest choriocarcinoma with large necrotic and hemorrhagic areas that interested the endocervical wall until near the endocervical mucosa and adjacent smooth muscle fibers (Figure 4).
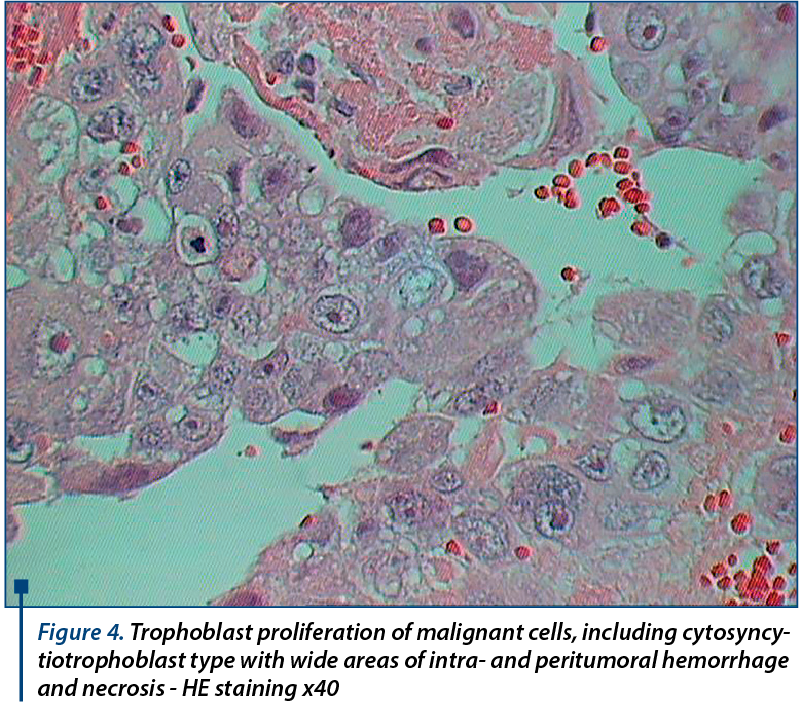
Immunohistochemistry testing was recommended for certainty diagnosis. It revealed AE1-AE3 diffusely positive in tumor cells; bHCG diffusely positive in the syncytiotrophoblast; HPL diffusely positive in the syncytiotrophoblast; MUC4 positive zonal type in intermediate trophoblast; Ki-67 positive in 97% of tumor cells. The positive was established as trophoblastic tumor proliferation in the type of choriocarcinoma. It was recommended the interpretation of the result in anatomical, clinical and imaging context, correlated with the dynamic bHCG dosing (Figure 5).

Postoperative evolution of the patient was good, being discharged from the hospital three days later. She underwent 6 cycles of Methotrexate 1 mg/kgc after the discharge, the serum bHCG levels continuously dropping, and becoming negative after 3 rounds of chemotherapy. The last 3 rounds were recommended for stabilization. The follow-up of the patient revealed normal clinical and ultrasound exams, until 3 months postoperative.
Discussions
Choriocarcinoma is a highly aggressive tumor, which depending on the association with pregnancy has two different forms. It usually appears after a malignant alteration in a molar gestation, only rarely after an abortion or normal or ectopic pregnancy(9). If associated with gestation, it is the most aggressive, malignant form of GTN and bears the name of gestational choriocarcinoma. If it appears in the absence or preceding pregnancy, the term used is non gestational choriocarcinoma, appearing most frequently in the ovary in women or testes in men. CCA usually arises in association with genital organs such as: the uterus, which is the most common site, the cervix, the fallopian tubes, the ovary, the vagina, the vulva or the vulvar region. It can also occur extremely rare outside the reproductive system, the sites of appearance where it has been described including: the brain, the lungs, the pulmonary arteries, the stomach, the small intestine or the pancreas. Even more rare cases of intrauterine pregnancy associated with placental CCA have been reported(10). Trophoblastic tumor cells have great affinity for blood vessels, which is why the tumors frequently metastasize by hematogenous route(11).
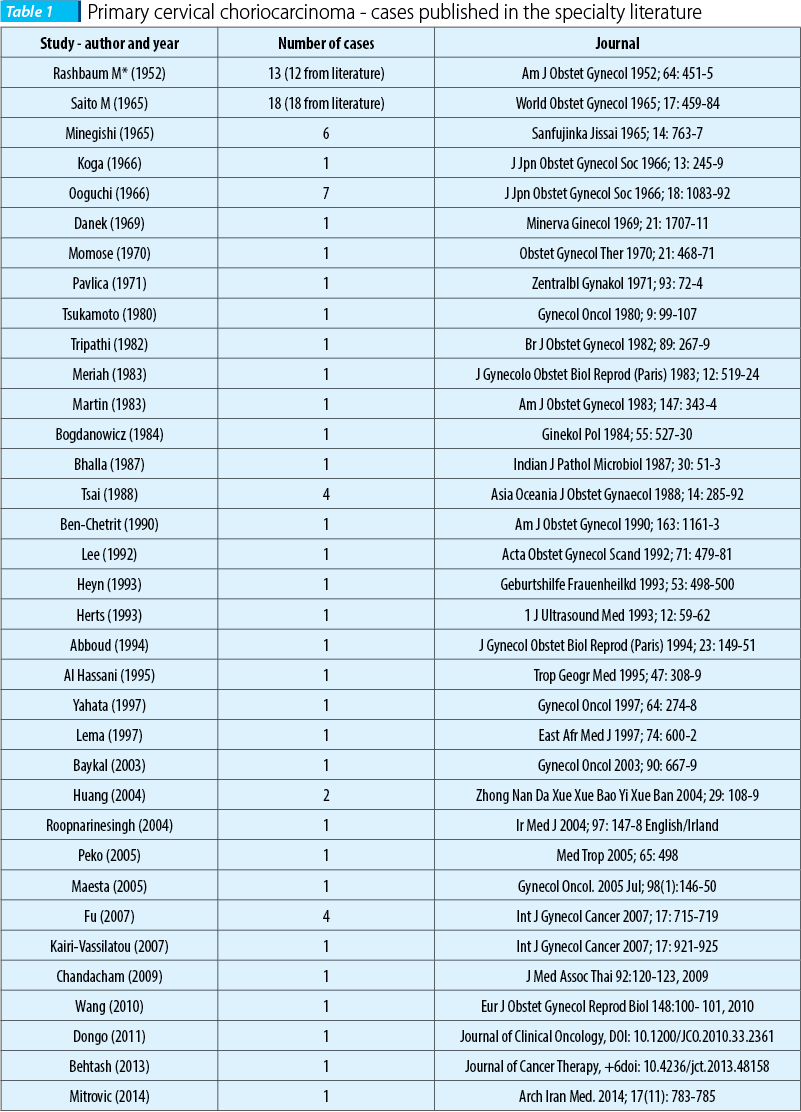
Saito et al. established the diagnostic criteria for extrauterine CCA, which include the absence of tumor inside the uterine cavity, the anatomopathological exam confirming the diagnosis, the exclusion of molar pregnancy and of coexisting normal intrauterine pregnancy(12). Although an extremely rare pathology with only 87 cases reported in literature until present (Table 1), from all types of extrauterine CCA, the cervical one is the most common, and several hypotheses have been developed in order to explain its physiopathology(13). Some authors say it could be a metastasis of a vanishing uterine choriocarcinoma, others a malignant transformation of a cervical pregnancy, others describe it as the result of the implantation of trophoblasts in the cervix after an abortion with malignant change after a dormant period(14,15).
The risk of fetal teratogenicity from chemotherapy is present only if conception occurs during or immediately following the treatment cycles. Fertility is not impaired following chemotherapy. Successful pregnancies have occurred in women who have had widespread GTN, including cerebral metastases(16).
After a search on PubMed on “primary cervical choriocarcinoma”, we found 36 published papers from 1950 untill now, most of them being case reports.
The prevalence of CCA has decreased in the recent years according to the improvement of the social and economic conditions, remaining higher in Africa, Asia and South America compared to the United States and Europe(17,18).
The diagnosis of cervical CCA is a difficult one considering its rare incidence, the differential diagnosis including isthmus or cervical leiomyomas, cervical cancer, endocervical polyp, abortion and cervical pregnancy(19-21). In our case, the cervical CCA was first suspicioned to be a uterine leiomyoma protruding into the cervical cavity.
The suggestive ultrasound aspect showing intense vascularization was the diagnosis element that determined us to measure the bHCG serum level, knowing that trophoblastic malignant cells produce up to 100 times more hormone than normal cells(22). That is why its measurement has a great diagnostic value and is a useful tool in the follow-up of the patient, as it is the most important recurrence predictor factor of the disease(23).
Although in very rare cases its value is not very elevated, in our patient the extreme level of serum bHCG correlated with the rich vascularization was the decisive factor that inclined the balance towards considering cervical CCA as the positive diagnosis.
Usually the diagnosis of a primary extrauterine CCA is difficult because of the non-specific clinical presentation that can mimic other conditions(24). Persistent vaginal bleeding of small to moderate intensity present in our patient, correlated with the clinical exam, suggested the suspicion diagnosis of a posterior uterine leiomyoma, which is a frequent confusion when confronting with extrauterine CCA. The cervical CCA suspicion diagnosis was established based on imaging aspect - transvaginal ultrasound showing a parenchymatous area that protrudes into the cervical canal with intense peripheral vascular network and contrast-enhanced MRI describing an expansive bulky, round-oval, well defined mass with a long necrotic pedicle and extensive central area of necrosis.
Given the clinical status of the patient, uterus conservative surgical excision was decided with histopathological extemporaneous exam. Trophoblast cells surrounded by extensive necrosis are typical aspects of the CCA on microscopic evaluation.
A trachelectomy was performed, followed by abdominal uterine cerclage, in order to preserve the patient’s ability to carry a future pregnancy until term. This type of approach, with conservative management of primary cervical choriocarcinoma, was also reported by Ben-Chetrit and his co-workers and by Roopnarinesingh et al.(25,26). In literature, most of the cases of cervical CCA were treated by total hysterectomy due to massive bleeding. Nowadays, selective uterine arterial embolization may represent a useful tool in order to control important bleeding from cervical CCA, and surgical excision tends to be more conservative, as in our case, in women that want to procreate in the future(27). Given the fact that CCA is a highly chemosensitive tumor, having generally a good prognosis even in advanced stages, the conservation of reproductive function should be considered if possible(28).
The therapeutic response to Methotrexate in our case was very good, serum bHCG level becoming zero after three cycles, which is a common aspect in this type of tumor.
Accurate positive diagnosis of CCA is realized through immunohistochemistry evaluation (IHC), the AE1-AE3 markers, bHCG, HPL, MUC4 and Ki-67 diffusely positive in tumor cells confirming the diagnosis of primary cervical gestational choriocarcinoma. IHC is the only diagnostic tool that can separate the origin on CCA whether gestational or non-gestational(29).
Conclusions
Primary cervical choriocarcinoma is an extremely rare condition that should be considered in the differential diagnosis of a cervical mass with profuse bleeding particularly due to intense vascularity, especially in young women. Serum bHCG dosage, transvaginal color Doppler ultrasonography and contrast MRI represent the paraclinical panel in these cases. Interpretation of the results in anatomical, clinical and imaging context, correlated with patient’s clinical history and bHCG dynamic is required in order to correctly diagnose it and recommend the optimum treatment. Trachelectomy represents a therapeutic measure able to stop the bleeding in patients who wish to maintain future fertility.
Bibliografie
2. Biscaro A, Braga A, Berkowitz RS. Diagnosis, classification and treatment of gestational trophoblastic neoplasia.Rev Bras Ginecol Obstet. 2015; 37(1):42-51.
3. Benirschke K, Kaufmann P, Baergen RN, Pathology of the Human Placenta, Springer, New York, 2006:191.
4. Goldstein DP, Berkowitz RS. Current management of gestational trophoblastic neoplasia. Hematol Oncol Clin North Am. 2012; 26(1):111-31.
5. Osborne R, Dodge J. Gestational trophoblastic neoplasia. Obstet Gynecol Clin North Am. 2012; 39(2):195-212.
6. Mitrovic S, et al. Gestational choriocarcinoma of the cervix. Arch Iran Med, 2014, 17(11):783-5.
7. Lurain JR. Gestational trophoblastic disease II: classification and management of gestational trophoblastic neoplasia. Am J Obstet Gynecol, 2011; 204(1):11-8.
8. Seckl MJ, Sebire NJ, Fisher RA, Golfier F, Massuger L, Sessa C, et al. Gestational trophoblastic disease: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24 Suppl 6:vi39-50.
9. Dehner LP. Gestational and nongestational trophoblastic neoplasia: a historic and pathobiologic survey. Am J Surg Pathol, 1980; 4:43-58.
10. Fox H. Gestational trophoblastic disease: neoplasia or pregnancy failure? BMJ, 1997; 314:1363-4.
11. Robboy SJ, Anderson MC, Russell P. Pathology of the female reproductive tract. Philadelphia; Churchill Livingstone, 2002.
12. Saito M, Azuma T, Nakamura K. On ectopic choriocarcinoma. World Obstet Gynecol. 1965; 17:459-84.
13. Kairi-Vassilatou E, Papakonstantinou K, Grapsa D, Kondi-Paphiti A, Hasiakos D. Primary gestational choriocarcinoma of the uterine cervix: Report of a case and review of the literature. Int J Gynecol Cancer. 2007; 17:921-5.
14. Maestá I, Michelin OC, Traiman P, Hokama P, Rudge MV. Primary non-gestational choriocarcinoma of the uterine cervix: A case report. Gynecol Oncol, 2005; 98:146-50.
15. Wang D, He Y, Hu Y, Xie C, Yin R. Placental site trophoblastic tumor with unusual presentation in the uterine cervix. Eur J Obstet Gynecol Reprod Biol, 2010; 148:100-1.
16. Welsnd PY, Ouyang PC. Trophoblastic Disease in Taiwan: A Review of 157 Cases on a 10-Year Period. Am J Obstet Gynecol, 85; 1963:844-9.
17. Fu Y, Lu W, Zhou C, Xie X. Primary Cervical Choriocarcinoma: Report of Four Cases and Literature Review. Int J Gynecol Cancer, 2007; 17(3):715-9.
18. Maesta I, Michelin OC, Traiman P, Hokama P, Rudge MV. Primary non-gestational choriocarci-noma of the uterine cervix: a case report. Gynecol Oncol, 2005; 98:146-5.
19. Baykal C, Tulunay G, Bulbul D, Boran N, Kose MF. Primary choriocarcinoma of the uterine cervix in a postmenopausal patient: a case report. Gynecol Oncol 2003; 90: 667-9.
20. Lee JD, Chang TC, Lai YM, Hsueh S, Soong YK. Choriocarcinoma of the cervix. Acta Obstet Gynecol Scand, 1992; 71:479-81.
21. Pavelka JC, Bryant DA, Vaccarello L. Adenocarcinoma of the uterine cervix with choriocarcinomatous metastasis. Gynecol Oncol, 2006; 101:346-8.
22. Yahata T, Kodama S, Kase H, Sekizuka N, Kurabayashi T, Aoki Y, et al. Primary choriocarcinoma of the uterine cervix: clinical, MRI and color Doppler ultrasonographic study. Gynecol Oncol, 1997; 64:274-8.
23. Speroff L, Fritz, MA. Clinical gynecologic endocrinology and infertility. 7th eds. Philadelphia: Lippincott Williams & Wilkins; 2005.
24. Chen MJ, Yang JH, Lin MC, Ho HN, Yang YS. An unusual gestational choriocarcinoma occurring primarily on the surface of a subserous leiomyoma. BJOG. 2004; 111:188-90.
25. Ben-Chetrit A, Yagel S, Ariel I, Zacut D, Shimonovitz S, Ceinikier-Hochner D. Successful Conservative Management of Primary Nonmetastatic Cervical Choriocarcinoma, Am J Obstet Gynecol, 1990, 163(4):1161-3.
26. Roopnarinesingh R, Igoe S, Gillan JE. Choriocarcinoma Presenting as a Primary Lesion of the Cervix. Irish Medl J, 2004(97):147-8.
27. Telerman A. Germ cell tumors of the ovary. In: Kurman RJ, editor. Blaustein’s pathology of the female genital tract. 5th ed NY Springer-Verlog; 2002:967-1033.
28. Chandacham A, Kietpeerakool C, Khunamornpong S, et al. Successfully conservative treatment of large cervical choriocarcinoma with profuse vaginal bleeding. J Med Assoc Thai, 2009; 92:120-3.
29. Zhao J, Xiang Y, Wan XR, Feng FZ, Cui QC, Yang XY. Molecular genetic analyses of choriocarcinoma. Placenta. 2009; 30:816-20.