A 44-year-old man presented for repetitive epistaxis and marked physical asthenia. The clinical exam revealed only profuse sweating, moderately pale teguments and hepatosplenomegaly.
The CBC at admission showed severe pancytopenia: WBC 3800/mm³, hemoglobin 6.9 g/dl and platelet count 17,000/mm³. The biochemistry was unremarkable, with the exception of increased LDH (> 5x normal) and mild hepatocytolysis.
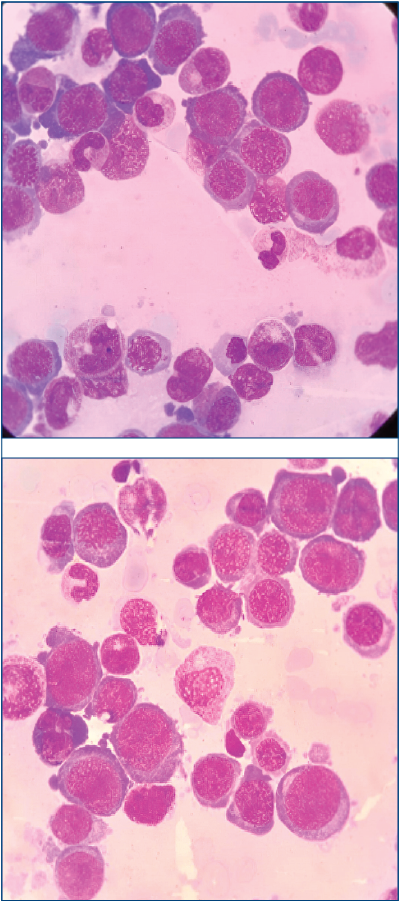
The peripheral blood smear revealed leukoerythroblastosis, with 13% blasts and 35 erythroblasts per 100 nucleated elements. The blast cells were medium-large in size, with basophilic cytoplasm, thin chromatin, nucleoli, some with granulation and rare with Auer bodies.
The bone marrow smear described hypercellular blood marrow, with 10% blast cells and markedly increased erythroblastic lineage (79%). The erythroblastic cells were large, with megaloblastic features, abundant basophilic cytoplasm with cytoplasmic projections and vacuolization, immature nuclear chromatin, and occasional nucleoli. The PAS staining was suggestive for AML6(1).
Immunophenotypic profile: glycophorin A positive, CD71 positive and CD33 positive, being suggestive for erythroleukemia – FAB classification(2) – AML6. This subtype is an exceptionally rare category of acute leukemia (3-8%), usually accompanied by unfavorable prognosis and evolution(1).
The cytogenetic exam revealed loss of the long arm of chromosome 5 – del (5q), associated with an adverse outcome(2).
The patient was successfully treated according to the “3+7” induction protocol(3) and then referred for consolidation with allogeneic bone marrow transplantation, performed from a matched unrelated donor, fortunately with a surprising favorable evolution.
Conflict of interests: The authors declare no conflict of interests.