Renal cell carcinoma represents the most frequent type of kidney cancer and accounts for 2-3% of all adult malignant tumors. Papillary renal cell carcinoma (pRCC) is the second most common type of renal carcinoma. RCC usually metastasizes to the lungs, lymph nodes, bones, brain and liver. Renal carcinoma dissemination to the ovaries is an exceptional occurrence. A 60-year-old woman was admitted in January 2018 due to acute back pain and abdominal discomfort. An abdominal computed tomography (CT) scan with intravenous contrast revealed a solid mass with malignant features located on the left kidney, multiple enlarged lymph nodes, and pulmonary metastases – cT3N1M1(pul). The patient underwent radical left nephrectomy and para-aortic lymphadenectomy followed by treatment with pazopanib. The pathologic study revealed papillary renal cell carcinoma. In June 2018, the patient presented with abdominal pain, postprandial bloating, nausea, vomiting and abdominal distension (ECOG 3). CT imaging showed stable pulmonary metastases and left ovarian mass. An exploratory laparotomy was performed, revealing a 8x7 cm ovarian mass, followed by left adnexectomy. The histopathological report described carcinomatous infiltration of the left ovary and fallopian tube, while the immunohistochemical staining could not clearly differentiate between a primary ovarian tumor and a metastasis. Corroborating the histopathological and immunohistochemical reports with the clinical status, the diagnosis of a synchronous primary ovarian tumor was decided. The treatment was continued with paclitaxel 125 mg/m2 + carboplatin AUC 6, q3w, and pazopanib 800 mg/daily, with clinical benefit after the first administration, although before the fifth cycle the patient’s clinical status rapidly deteriorated.
Tumoră primară ovariană sau metastaze ale unui carcinom cu celule renale – prezentare de caz
Ovarian primary or renal cell cancer metastases – a case report
First published: 30 martie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.50.1.2020.2957
Abstract
Rezumat
Carcinomul cu celule renale reprezintă tipul cel mai frecvent de cancer renal şi cuprinde 2-3% din tumorile maligne ale adulţilor. Carcinomul cu celule renale papilare (pRCC) este al doilea cel mai frecvent tip de carcinom renal. CCR metastazează de obicei în plămâni, ganglioni, oase, creier şi ficat. Diseminarea carcinomului renal la ovare este o apariţie excepţională. O pacientă de 60 de ani a fost internată în ianuarie 2018 în urgenţă cu dureri de spate şi abdominale. Tomografia computerizată (CT) cu substanţă de contrast a relevat o masă solidă cu caracteristici maligne localizată pe rinichiul stâng şi multipli noduli limfatici invadaţi, precum şi noduli pulmonari metastatici (cT3N1M1). Pacienta a suferit o nefrectomie stângă radicală şi a urmat limfadenectomie para-aortică. A urmat tratament cu pazopanib. Examenul histologic a relevat carcinom cu celule renale papilare. În iunie 2018, pacienta s-a prezentat cu durere abdominală, balonare postprandială, greaţă, vărsături şi distensie abdominală (ECOG3). Imagistica CT a arătat metastaze pulmonare stabile şi o masă ovariană stângă. O laparotomie exploratorie a fost efectuată, relevând o masă ovariană de 8x7 cm care a fost rezecată. Raport histopatologic: tumoră carcinomatoasă a ovarului stâng şi trompei falopiene, în timp ce imunohistochimia nu a putut diferenţia în mod clar între o tumoră ovariană primară şi o metastază. Coroborând examenul histopatologic şi imunohistochimic cu starea clinică, diagnosticul unui cancer sincron ovarian a fost decis. Tratamentul a fost continuat cu paclitaxel 125 mg/m2 + carboplatin AUC 6, q3w, şi pazopanib 800 mg/zi, cu beneficiu clinic după prima administrare, deşi înainte de al cincilea ciclu starea clinică a pacientei s-a deteriorat.
Introduction
Renal cell carcinoma (RCC) represents the most frequent type of kidney cancer and accounts for 2-3% of all adult malignant tumors(1). It is considered the most lethal genitourinary cancer(2), defined by an asymptomatic disease course, with late and uncharacteristic symptoms, leading to a poor survival prognosis(3). Based on histological features, RRC is categorized into clear cell, papillary and cromophobe types.
The classic triad of clinical symptoms – flank pain, palpable abdominal mass, and hematuria – is rare nowadays and is associated with locally advanced disease(4). Early diagnosis is rare, although the discovery of a renal mass can be incidental due to advances in imaging techniques.
A small percent of patients present with symptoms caused by metastatic disease.
Renal cell carcinoma usually metastasizes to the lungs, lymph nodes, bones, brain and liver, and only very rarely to the ovary (23 cases known worldwide to date).
Case report
A 60-year-old woman, with a history of stage 2 hypertension therapeutically controlled and with surgery for herniated disc in the lumbar region, was admitted in January 2018 due to acute back pain and abdominal discomfort.
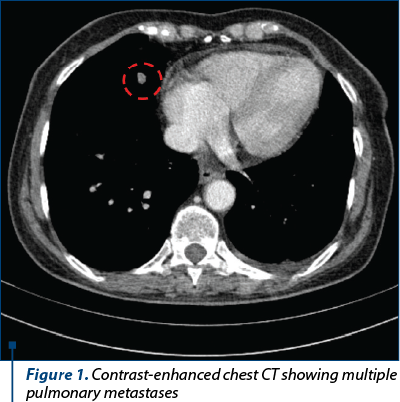
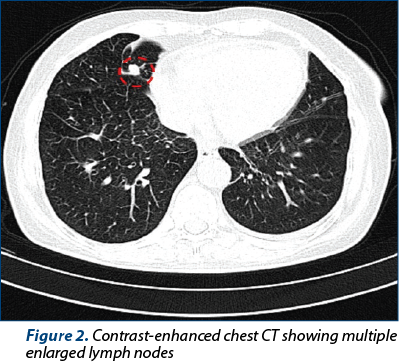
A computed tomography (CT) scan with intravenous contrast revealed a solid mass with malignant features located on the left kidney, multiple enlarged lymph nodes, and pulmonary metastases – cT3N1M1(pul) (Figures 1 and 2). The patient underwent radical left nephrectomy and para-aortic lymphadenectomy on January 17, 2018 (Figure 3). The pathologic study revealed papillary renal cell carcinoma (pT4pN1M1pul,lym) with subsequent immunohistochemical (IHC) results, as follows: PAX8 (+), vimentin (+), CD10 (+), AMACR (+), WT1 (-), calretinin (-).
After the surgery she was referred to the Oncology Clinic of the “Filantropia” Municipal Hospital Craiova. According to the International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) criteria, the patient was categorized into the intermediate-risk group. The preferred choice of treatment with immunotherapy is not available as first line in our country (nivolumab + ipilimumab), so TKI (tyrosine kinase inhibitor) treatment with pazopanib was initiated in mid-February. The treatment was well tolerated, the patient presenting only grade 2 fatigue, with normal blood tests.
In June 2018, the patient presents with abdominal pain, postprandial bloating, nausea, vomiting and abdominal distension (ECOG 3). Contrast-enhanced chest-abdomen-pelvis CT showed stable pulmonary metastases and left ovarian mass (Figure 4).
The serum cancer antigen 125 (CA-125) level (65 U/mL) was higher than the normal range (1.9-16.3 U/mL). In July 2018, an exploratory laparotomy was performed, revealing chylous ascites and a 8x7 cm ovarian mass, followed by left adnexectomy.
The histopathological report described carcinomatous infiltration of the left ovary and fallopian tube, while the immunohistochemical staining could not clearly differentiate between a primary ovarian tumor and a metastasis: ER (-), CK7 (+), napsin A (+), PAX8 (+), CD10 (+), WT1 (-), ki 67 (+) in 10% of the tumor cells.
Corroborating the histopathological and immunohistochemical reports with the clinical status, the diagnosis of a synchronous primary ovarian tumor was decided.
The treatment was continued with paclitaxel 125 mg/m2 + carboplatin AUC 6, q3w, and pazopanib 800 mg/daily, with clinical benefit after the first administration, the patient accusing fatigue as the only symptom.
However, before the fifth cycle, the patient’s clinical status rapidly deteriorated: ECOG 3, abdominal pain, abdominal distension, nausea, vomiting, suggesting a subocclusive intestinal syndrome. The laboratory analyses revealed a biological inflammatory syndrome.
Paracentesis was performed and 2.5 l of hemorrhagic, chylous ascites were evacuated. Subsequently, the symptomatic treatment had limited benefit.
Discussion
Renal cell carcinoma is categorized into clear cell (ccRCC) – the most prevalent, consisting of 75-80% of cases – and non-clear cell RCC, according to its histological characteristics. The most common variant of non-clear cell RCC is represented by papillary RCC (pRCC), accounting for 10-15% of all RCCs(5,6). Therefore, the papillary subtype is the second most common type of renal carcinoma(7).
Secondary involvement of the ovaries represents 7% to 15% of the ovarian neoplasms(8), the most frequent primary sites of the malignancies being the stomach, the colon, the breast, the endometrium and the endocervix(9).

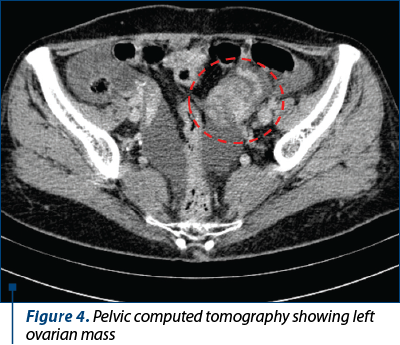
Renal carcinoma dissemination to the ovaries is an exceptional occurrence. The predominance of RCC in males(10), the vascular sclerosis of the postmenopausal ovary, rare events of tumor emboli to the ovaries, as well as the misdiagnoses of certain metastases as primary ovarian neoplasms(11) can account for this low incidence. Therefore, the diagnosis may sometimes prove challenging. First, ovarian metastases from other organs are generally bilateral, whereas metastases from renal tumors to ovaries are typically unilateral due to the distinct venous anatomy of renal-ovarian axis, the latter draining directly into the left renal vein(12), consistent with our case. In addition, its unilaterality could suggest the diagnosis of an ovarian primary tumor.
Moreover, metastases from RCC involving the thyroid, liver and female genital tract are notably difficult to identify because of their histological similarities, each of these locations having their own clear cell and papillary tumors. Particularly, pRCC can mimic other papillary tumors, such as ovarian clear cell carcinoma (OCCC) and ovarian serous carcinoma(13,14). The immunohistochemical staining is used to ascertain the nature of the tumor in difficult cases. Serous carcinoma tests positive for Wilms’ tumor 1 (WT-1), while negative staining for WT-1 supports the metastatic carcinoma(14). The ovarian tumor was positive for CD10, PAX8 and napsin, which favored its renal origin(15,16). Furthermore, cytokeratin 7 (CK7) tested positive, which is consistent with the immunoprofile of pRCC(17).
However, the inconclusive histopathological and immunohistochemical reports recommended correlating the results with the clinical context. Considering the rare incidence of renal carcinoma dissemination to the ovaries and the disadvantages of second-line immunotherapy for disease progression (response rate ~25%, delayed response, symptomatic patient), the diagnosis of a synchronous primary ovarian tumor was established.
As a result, the patient received platinum-based chemotherapy, carboplatin and paclitaxel, while continuing the treatment with the tyrosine kinase inhibitor, with clinical benefit after the first administration. The concomitant use of pazopanib and paclitaxel increases the AUC and Cmax of the latter by 26% and 31%, respectively, pazopanib inhibiting the CYP450-mediated metabolism. Due to drug interactions, a lower dose of paclitaxel was given. Despite the clinical improvement, before the fifth cycle, the patient’s condition deteriorated, with symptomatic treatment having limited benefit.
Conclusions
Considering the major therapeutic and prognostic differences between ovarian metastases and ovarian primary tumor, it is critical to make a distinction between the two entities using primarily microscopic analysis with subsequent immunohistochemical study.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
- Cohen HT, McGovern FJ. Renal-cell carcinoma. N Engl J Med. 2005; 352(23), 2477-90.
- Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. 2018; 68(1), 7-30.
- Gudbjartsson T, Thoroddsen A, Petursdottir V, Hardarson S, Magnusson J, Einarsson GV. Effect of incidental detection for survival of patients with renal cell carcinoma: results of population-based study of 701 patients. Urology. 2005; 66(6), 1186-91.
- Courthod G, Tucci M, Di Maio M, Scagliotti GV. Papillary renal cell carcinoma: A review of the current therapeutic landscape. Crit Rev Oncol Hematol. 2015; 96(1), 100-12.
- Patard JJ, Leray E, Rioux-Leclercq N, Cindolo L, Ficarra V, Zisman A, De La Taille A, Tostain J, Artibani W, Abbou CC, Lobel B, Guillé F, Chopin DK, Mulders PF, Wood CG, Swanson DA, Figlin RA, Belldegrun AS, Pantuck AJ. Prognostic value of histologic subtypes in renal cell carcinoma: a multicenter experience. J Clin Oncol. 2005; 23(12), 2763-71.
- Beck S, Patel M, Snyder M, Kattan M, Motzer R, Reuter V, Russo P. Effect of papillary and chromophobe cell type on disease-free survival after nephrectomy for renal cell carcinoma. Ann Surg Oncol. 2004; 11(1), 71-7.
- Akhtar M, Al-Bozom IA, Al Hussain T. Papillary Renal Cell Carcinoma (PRCC): An Update. Adv Anat Pathol. 2019; 26(2), 124-132.
- Turan T, Aykan B, Koc S, Boran N, Tulunay G, Karacay O, Erdogan Z, Kose F. Analysis of metastatic ovarian tumors from extragenital primary sites. Tumori. 2006; 92(6), 491-5.
- Petru E, Pickel H, Heydarfadai M, Lahousen M, Haas J, Schaider H, Tamussino K. Nongenital cancers metastatic to the ovary. Gynecol Oncol. 1992; 44(1), 83-6.
- Toquero L, Aboumarzouk OM, Abbasi Z. Renal cell carcinoma metastasis to the ovary: a case report. Cases J. 2009; 2, 7472.
- Kostrzewa M, Zyła M, Władziński J, Stetkiewicz T, Stachowiak G, Wilczynski J. Metastases of renal clear cell carcinoma to ovary – case report and review of the literature. Eur J Gynaecol Oncol. 2015; 36(2), 219-22.
- Bhaskar V, Kumar M, Goel S, Sankhwar S. Papillary renal cell carcinoma with synchronous ovarian metastasis: a rare entity. BMJ Case Rep. 2017; pii: bcr-2017-220764.
- Stolnicu S, Borda A, Rădulescu D, Puşcaşiu L, Berger N, Nogales FF. Metastasis from papillary renal cell carcinoma masquerading as primary ovarian clear cell tumor. Pathol Res Pract. 2007; 203(11), 819-22.
- Liang L, Huang H, Dadhania V, Zhang J, Zhang M, Liu J. Renal cell carcinoma metastatic to the ovary or fallopian tube: a clinicopathological study of 9 cases. Hum Pathol. 2016; 51, 96-102.
- Ordi J, Romagosa C, Tavassoli FA, Nogales F, Palacin A, Condom E, Torné A, Cardesa A. CD10 expression in epithelial tissues and tumors of the gynecologic tract: a useful marker in the diagnosis of mesonephric, trophoblastic, and clear cell tumors. Am J Surg Pathol. 2003; 27(2), 178-86.
- Ozturk Sari S, Ozluk Y, Taskin OC, Polat B, Ozturk I, Ekenel M, Kilicaslan I, Bilgic B. Papillary Renal Cell Carcinoma Arising in a Lymph Node Metastasis of a Testicular Teratoma: A Very Rare Occurrence. Int J Surg Pathol. 2016; 24(5), 468-72.
- Alshenawy HA. Immunohistochemical Panel for Differentiating Renal Cell Carcinoma with Clear and Papillary Features. Pathol Oncol Res. 2015; 21(4), 893-9.
Articole din ediţiile anterioare
Tumoare germinală testiculară nonseminomatoasă cu prognostic rezervat
Prezentăm cazul unui pacient în vârstă de 37 de ani, fără antecedente patologice semnificative, care s-a prezentat la camera de gardă cu dispnee ...
Variability of response to multimodal therapy in a stage IV bronchial carcinoid: a case report
Neoplasmele pulmonare neuroendocrine (NEN) se clasifică în tumori neuroendocrine (NET) şi carcinoame neuroendocrine (NEC). NET cuprind tumo...
Giant solitary lung metastasis from an osteosarcoma (malignant fibrous histiocytoma-like) of the spine
Prezentăm cazul unui bărbat nefumător, în vârstă de 69 de ani, care a venit la spital pentru dispnee, dureri toracice, hemoptizie, pierderea pof...
Metastaze pancreatice hipervasculare: sunt un diagnostic imagistic uşor?
Obiectiv. De a revizui caracteristicile computer-tomografice (CT) şi de imagistică prin rezonanţă magnetică (IRM) ale metastazelor pancreatice hi...