The aim of this paper is to analyze the bone stability of calvarium bone grafts in the atrophied edentulous ridges. The success of graft incorporation is over 98%. During a 5-year interval, the bone volume remains almost unaltered, implant bone resorption being very low. The complications are scarce, the main being wound dehiscence, especially in mandibular sites.
Reconstrucţia maxilarelor atrofiate cu grefe parietale
Calvarium bone graft in severe maxilla atrophy
First published: 30 noiembrie 2018
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Orl.41.4.2018.2120
Abstract
Rezumat
Scopul acestei lucrări este de a analiza stabilitatea transplanturilor osoase parietale în defectele severe ale maxilarelor edentate. Succesul integrării osoase este de peste 98%. Pe o perioadă de cinci ani, stabilitatea volumetrică osoasă este foarte bună, resorbţia periimplantară fiind redusă. Rata de complicaţii este redusă, iar dehiscenţa rămâne principala complicaţie, în special în situsurile mandibulare.
Introduction
Oral rehabilitation using dental implants has a high rate of success. There are many cases where severe bone atrophy impinges dental implants insertion. There are many procedures described to overcome this issue. There are many bone substitutes, but when the atrophy is important, the autologous bone remains the gold standard(1). There are intraoral donor sites (posterior mandible, chin) for smaller defects limited to a dental quadrant. For larger defects such as bimaxillary, the clinicians must use extra oral donor sites. The favourite regions are the parietal calvarium and the iliac crest(2). The calvarium offers the clinician a generous volume of bone and has the same type of ossification as the jaws. The bone stability is enhanced compared to ileum due to the cortical nature of the bone.
Method
Case selection
A group of 36 patients was taken into consideration. They all received different bone blocks. Five cases (four females, one male) were selected for the study which met the following criteria:
-
severe bone atrophy
-
bone reconstruction with calvarium grafts
-
at least five-year clinical and radiological follow-up.
The mean age was 51 years old (43-61 years old).
Surgical protocol
The patients who were diagnosed with bone atrophy class V and beyond were subjected to bone transplants form the calvarium and the ileum. There were excluded from the study those who underwent oncological treatment and those who had a history of bisphosphonates administration. In the present study, only those who received calvarium grafts were included.
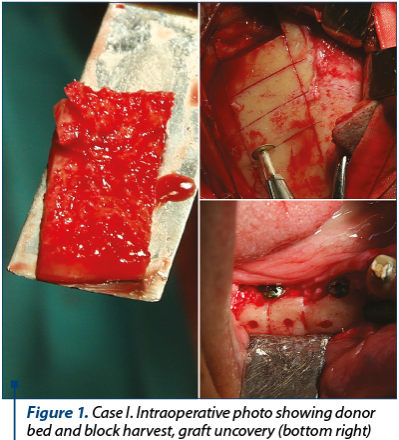
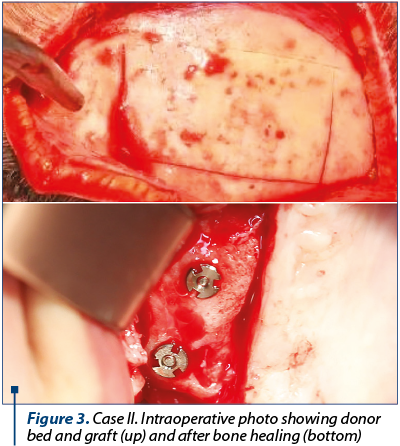
The transplant procedure was undertaken in ingoing patients, under general anaesthesia, usually nasal intubation. The incision at the donor site was tailored in a straight or curved line, the length varied upon the amount of bone needed. The bone blocks were harvested ensuring a safe distance from the sagittal and coronal suture. Only the outer cortex was harvested. The remaining bone defect can be filled with orthopaedic cement. There was no need for drainage tubes.
After bone harvest, the transplants were intimately adapted at the recipient sites to ensure proper fitting. They were fixed with osteosynthesis screws. The patients were instructed not to wear removable dentures throughout the healing phase.
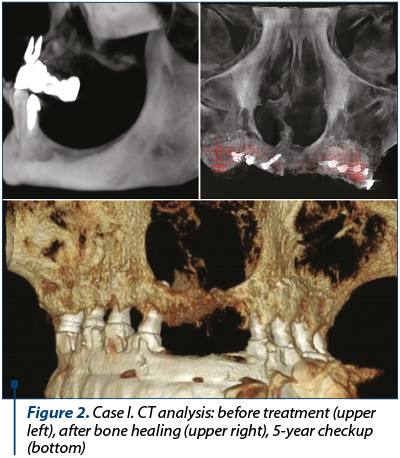
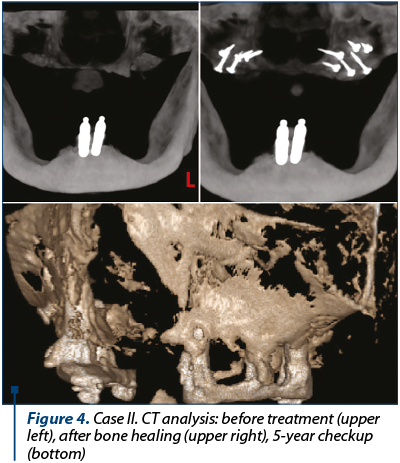
After three months, a tomography was taken, the screws were removed and dental implants were inserted in the reconstructed sites. After three months, a definitive prosthesis was delivered.
The check-ups were taken on a yearly base; clinical and radiological examination was undertaken every time.
Graft success
A total of 48 blocks were fixed to recipients sites. There was no record of total graft resorption. In one case, there was a wound dehiscence which led to partial bone resorption, but it did not jeopardize the overall treatment plan.
The success criteria were(3): the lack of dehiscence during the healing phase, graft incorporation at the recipient site and adequate bone volume for prosthetic implant placement. Before the grafts, the average width of the ridge was 3.10 mm measured by CBCT (cone beam computer tomography), and after graft healing the average width of the ridge was 9.25 mm. At the moment of prosthesis delivery, there was 1 mm bone resorption in 4% of the cases. After one year from the bone transplant, there was 1 mm bone resorption in 6% of the cases and 1-2 mm resorption in 4% of the cases. At the three-year checkup, there was 1 mm bone resorption in 8% of the cases and 1-2 mm resorption in 6% of the cases. At the five-year checkup, there was 1 mm bone resorption in 10% of the cases and 1-2 mm resorption in 6% of the cases. There was no severe resorption that could compromise the stability of the dental prosthesis.
At the donor site, there were no complications observed.
Discussion
The parietal calvarium offers a copious amount of bone in transplant surgery with straight forward access. The overall complications rate is pretty low. Improper use of the technique could lead to puncture of the inner cortex and cerebral fluid leak, extra Dural haematoma or even cerebral cortex trauma(4). The recovery is fast and in contrast with tibia or ileum bone harvest there are no functional impairments. The ileum bone grafts have a higher resorption rate when used intraoral(5).
The bone blocks can be harvested using standard instruments or with the help of piezosurgery devices.
The membranous ossification of calvarium corresponds to ossification of the jaws and bone incorporation is improved compared to the ileum grafts. Being mainly a cortical graft with a small spongy, the transplant maintains its volume even after the bone is set in function by the implant prosthesis(6). The main disadvantages derive from the need of a second surgical site and the need for general anaesthesia.
Conclusion
Autologous bone blocks are net superior to synthetic, mineral or animal grafts. Although the lot was small, when dealing with severe bone atrophy of edentulous ridges, the calvarium seems to be the appropriate donor site.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Sakkas A, Wilde F, Heufelder M, Winter K, Schramm A. Autogenous bone grafts in oral implantology-is it still a "gold standard"? A consecutive review of 279 patients with 456 clinical procedures. Int J Implant Dent. 2017;3(1):23.
- Crespi R et al: "Calvarial versus iliac crest for autologous bone graft material for a sinus lift procedure: a histomorphometric study." The International journal of oral & maxillofacial implants, vol. 22, no. 4, 2007 Jul-Aug, pp. 527-32.
- Friedmann A, Gissel K, Soudan M, Kleber BM, Pitaru S, Dietrich T, Randomized controlled trial on lateral augmentation using two collagen membranes:morphometric results onmineralized tissue compound. J Clin Periodontol. 2011, 38:677–685.
- Scheerlinck, Laura & Muradin, Marvick & Bilt, Andries & Meijer, Gert & Koole, Ronald & Cann, Ellen, Donor Site Complications in Bone Grafting: Comparison of Iliac Crest, Calvarial, and Mandibular Ramus Bone. The International journal of oral & maxillofacial implants. 2013, 28. 222-7. 10.11607/jomi.2603.
- Sbordone, Carolina et al, Volume Changes of Iliac Crest Autogenous Bone Grafts After Vertical and Horizontal Alveolar Ridge Augmentation of Atrophic Maxillas and Mandibles: A 6-Year Computerized Tomographic Follow-Up, Journal of Oral and Maxillofacial Surgery, Volume 70 , Issue 11 , 2559–2565.
- Smolka W, Bosshardt DD, Mericske-Stern R, Iizuka, Reconstruction of the severely atrophic mandible using calvarial split bone grafts for implant-supported oral rehabilitation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006,101:35–42.