Introduction. International medical students have an increased risk for mental health difficulties, through exposure to academic stress, competitiveness, low peer support, language barriers, paired with major life changes: temporary migration, acculturation, homesickness. Previous studies also reported high levels of psychological distress. Our aim was to assess the levels of perceived stress and reported well-being in a sample of foreign medical first year students enrolled in Romania.
Materials and methods. We included 91 participants, mean age 20.9 ± 3.7 years, 52.7% females, 71.4% Europeans, enrolled in the first year at the Faculty of Medicine, English Section, at “Iuliu Haţieganu” University of Medicine and Pharmacy, Cluj-Napoca. We used the Perceived Stress Scale to measure the level of perceived stress, and the 5-item World Health Organization Well-Being Index to assess the perceived well-being.
Results. Female students reported a higher level of perceived stress than males, total score 29.05 ± 6.46 vs. 24.19 ± 8.19 (p<0.05 – t Student Test), but there were no statistically significant differences concerning well-being (p>0.05 – t Student Test). The levels of perceived stress and well-being were negatively correlated both in male participants (Pearson’s= -0.685, p<0.01) and female participants (Pearson’s = -0.673, p<0.01). The strongest negative correlation between perceived stress and well-being was found in non-European participants (Pearson’s= -0.85, p<0.01).
Conclusions. Female participants reported a significantly higher level of perceived stress and a similar level of perceived well-being, compared with males. The negative correlation between perceived stress and well-being was stronger in male participants, compared to females, and strongest in non-Europeans. This suggests that perceived stress may be more detrimental on well-being in male students and in more acculturated ones.
Stresul perceput şi starea de bine la studenţii medicinişti străini de anul I din România
Perceived stress and well-being among international first year medical students in Romania
First published: 27 aprilie 2018
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.52.1.2018.1634
Abstract
Rezumat
Introducere. Studenţii medicinişti străini au un risc crescut de dificultăţi de sănătate mintală, prin expunere la stres academic, competitivitate, sprijin social scăzut, bariere de limbaj, dar şi prin schimbări majore de viaţă (migrare temporară, aculturaţie, dor de casă). Studii anterioare au raportat un nivel crescut de distres psihologic la studenţi. Scopul acestei cercetări a fost evaluarea asocierii dintre stresul perceput şi starea de bine raportată de studenţii medicinişti străini din România din anul I, de la secţia de limbă engleză.
Materiale şi metodă. Au participat 91 de studenţi de anul I de la secţia de limbă engleză a Facultăţii de Medicină din cadrul Universităţii de Medicină şi Farmacie „Iuliu Haţieganu”, Cluj-Napoca (vârsta medie: 20,9±3,7 ani; 52,7% femei; 71,4% europeni). Am evaluat nivelul de stres perceput prin scala stresului perceput (PSS) şi starea de bine percepută prin scala de 5 itemi a Organizaţiei Mondiale a Sănătăţii (WHO-5).
Rezultate. Studentele au raportat un nivel semnificativ crescut al stresului perceput, comparativ cu studenţii (scorul total 29,05±6,46 vs. 24,19±8,19; p<0,05, testul t Student), dar nu au fost diferenţe semnificative privind starea de bine raportată (p>0,05, testul t Student). Am identificat o corelaţie negativă semnificativă între nivelul stresului perceput şi nivelul stării de bine la participanţii de sex masculin (Pearson’s= -0,685; p<0,01), la cei de sex feminin (Pearson’s= -0,673; p<0,01), respectiv non-europeni (Pearson’s= -0,85; p<0,01).
Concluzii. Studentele au raportat un nivel al stresului perceput semnificativ mai mare comparativ cu studenţii. Corelaţia negativă între stresul perceput şi starea de bine a fost mai puternică la studenţi, comparativ cu studentele, respectiv cea mai puternică la non-europeni. Aceste date sugerează că stresul perceput afectează în mai mare măsură starea de bine a studenţilor de sex masculin şi a celor mai aculturaţi.
Background and aims
Medical students are a risk group for mental health difficulties(1), with high levels of stress and high prevalence of anxiety and depression(2,3,4). The level of stress and depression during medical training are significantly higher than before the onset of medical training(1). Thus, 4.4% of medical students have anxiety, 1.9% panic disorder, 4.7% major depression, 5.8% other depressive symptoms, and 15.7% have psychosomatic complaints(5). Poor sleep awareness, poor sleep quality, and sleep deprivation (sometimes self-imposed) are also common in this population. Sleep-related difficulties may be a result or a precipitating factor of stress(6).
External factors such as medical school workload, family expectations(7), the demand to develop their professional identity(8), and internal factors such as perfectionism potentially leading to self-imposed excessive workload are associated with mental health difficulties in medical students(7).
However, only a small proportion of medical students seek help, because of the perceived social pressure that they should be ‘invincible’(9), while 10.7% of the medical students reported regular psychotropic substance use, for different reasons: “to calm down”, “to improve their sleep”, “to elevate mood”, “to improve cognitive performance”(5).
Medical training is a suboptimal environment for the students’ psychological health(1,10) due to high academic standards(11,12), study burden(2,13), frequent examinations(12), busy schedule(2), competitive environment(11,14) and rigors of medical education(15). In addition to medical student status, foreign medical students are more vulnerable to mental health difficulties, due to major life changes(2), temporary migration(16), homesickness(17), language barriers(18), sociocultural differences(19), challenges in maintaining religious practices(20), impaired sense of shared social identity(8,10), low peer support(14).
Due to all these issues, studies on student well-being and institutional efforts of universities have increasingly focused on mental health awareness in foreign medical students.
The current study aims to assess the relationship between the level of perceived stress and reported well-being in a sample of foreign first year medical students enrolled in Romania.
Method
Study population. The target population consisted of 201 students enrolled in the first year at the Faculty of Medicine, English Section, at “Iuliu Haţieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania, in the 2015/2016 academic year. Between May 1st and May 15th 2016, 150 of these students were approached; 120 agreed to participate in the study, and 91 filled in the questionnaire. One questionnaire was excluded from the data analysis due to the student’s age (48 years), which deemed him an outlier.
The mean age of participants was 20.9 ± 3.7 years. 52.7% of participants were women; based on geographic criteria, 71.4% of participants were Europeans.
Instruments. The Perceived Stress Scale (PSS) was used to measure the level of perceived stress. The 14-item self-assessment version of PSS is the most widely used measure of perceived stress(21). Eighty-one students provided complete data for this scale.
The 5-item World Health Organization’s Well-Being Index (WHO-5) was used to assess the perceived well-being. The WHO-5 questionnaire is a brief, comprehensive and easy to employ self-assessment measure for psychological well-being(22). Eighty-nine students provided complete data for this scale.
The statistical analysis was carried out with the IBM Statistical Package for Social Sciences™ (SPSS) version 20.0. Non-parametric tests Kolmogorov-Smirnov and Mann-Whitney U were used to test for distribution and compare variables across two samples. Spearman’s correlation was used to assess the correlation between non-normally distributed discrete variables.
Results
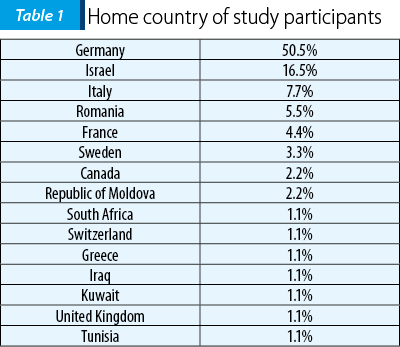
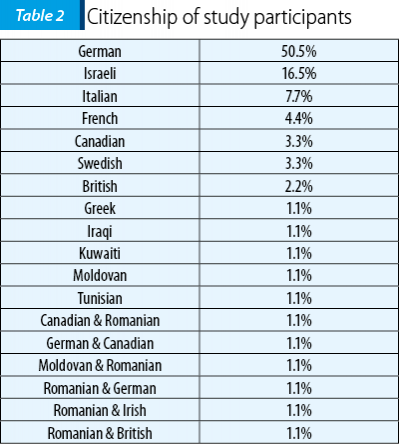
Most of our study participants were born in Germany (see Table 1). The most frequent citizenship was also German; some participants reported double citizenship (see Table 2).
Female students reported a significantly higher level of perceived stress than male ones, as measured by PSS total score: 29.05 ± 6.46 vs. 24.19 ± 8.19 (p<0.01 – Mann Whitney U). However, levels of reported well-being were similar in female and male students included in our study, as measured by WHO-5 total score: 15.21 ± 4.42 vs. 15.93 ± 3.93 (p>0.05 – Mann Whitney U Test).
European and non-European students reported similar levels of perceived stress (PSS total score 26.73 ± 7.18 vs. 27.6 ± 9.34, p>0.05 - Mann-Whitney U Test), and well-being, respectively (WHO-5 total score 15.73 ± 3.32 vs. 15.08 ± 5.9, p>0.05 - Mann-Whitney U Test).
39.6% of participants considered themselves religious persons, while 59.3% identified as not religious. Self-declared religious students and self-declared non-religious ones reported similar levels of perceived stress (PSS total score 26.55 ± 7.03 vs. 26.88 ± 8.16, p>0.05, Mann-Whitney U Test), and well-being (WHO-5 total score 16.08 ± 3.46 vs. 15.20 ± 4.66, p>0.05 - Mann-Whitney U Test).
The level of perceived stress and well-being were negatively correlated both in male participants (Spearman’s R=-0.662, p<0.01) and female ones (Spearman’s R=-0.594, p<0.01), both the religious ones (Spearman’s R=-0.593, p<0.01), and non-religious ones (Spearman’s R =-0.594, p<0.01). The strongest negative correlation between perceived stress and well-being was found in non-European participants (Spearman’s R=-0.85, p<.01), while the least strong was found in European ones (Spearman’s R=-0.542, p<0.01).
Discussion
The current study shows that female foreign first year medical students report higher levels of stress and similar levels of well-being, compared with male ones. Moreover, the level of perceived stress has a higher negative impact on well-being in male participants of our study. These results may be explained by the various gender-specific mediating factors of stress. Some studies show differences in coping mechanisms most frequently used by female and male medical students: denial and behavioral disengagement for women, and self-blame for men(23).
Our study also shows that the level of stress has a significant negative impact on well-being regardless of geographical area of origin. Nevertheless, the highest negative impact of perceived stress on well-being was observed in non-European participants. This finding may be explained through differences in risk factors for stress in non-European students. Several studies acknowledge the lack of social and family support(14), homesickness(17), adjustment difficulties(8,10,16,18,19), academic difficulties(11,12) as risk factors for stress in international students. These may result in higher levels of stress, loss of social contacts, and reduced quality of life(18). Moreover, foreign medical students may experience adjustment issues due to acculturation(16). Protective measures could be providing applied medical language courses, and programs for fostering connectedness and intercultural exchanges(18).
Our study also shows that the level of stress has a significant negative impact on well-being both in religious and non-religious students. Other studies, however, cite religious affiliation as one of the most frequent coping mechanisms used among physicians(24). Religious/spiritual medical students reported less frequent conflicts within the medical team, less work-life imbalance and less emotional stress arising from patient suffering; on the other hand, they may experience more inner struggle, self-doubt, or inadequacy generated by differences between medical training curriculum and personal religious beliefs(25). Other studies show that spiritual and existential well-being are associated with lower levels of perceived stress and depression(26).
An increasing body of data draws attention towards the mental health status of care providers. A recent study shows that depression scores decrease with every year of medical training(9). This may be due to the fact that years of experience and effectiveness of coping are positively correlated in physicians. Given the fact that most medical students are young adults with little experience, their coping mechanisms may be less effective, compared to experienced physicians. Maladaptive coping strategies, such as self-blaming, denial, and giving up, were cited as main predictors of depression, anxiety, and distress(12).
Mental health of medical trainees is a public health issue from enrollment and the first years of medical training, and this is when prevention should begin. Some universities have already started implementing mental-health supporting changes in the educational programs (such as adjustment of the curricula and the human anatomy exam difficulty, a pass/fail grading system in preclinical years, longitudinal and shorter electives), with good outcomes. Additional strategies focused on personal level, by implementing a resilience and mindfulness program, and organizing social events for all medical students(27). Mental health programs should also focus on modern technology-based cognitive behavioral therapy(28), and increasing emotional intelligence. Higher levels of emotional intelligence are associated with higher levels of satisfaction and lower perceived stress levels among all medical students, and better academic performance amongst final year medical students(29). Lastly, but maybe the most important intervention, mental health first aid courses and anti-stigma programs improved the quality of first aid intentions towards a person experiencing depression, decreased stigmatizing attitudes and desire for social distance from a person with depression, and increased mental health literacy and confidence in providing help to someone who is experiencing depression(30).
The current study has several important limitations. Firstly, the sample was divided into Europeans and non-Europeans based on geographical criteria. Nevertheless, some states – e.g., Israel (where 16.5% of the participants were from) – are European Union trade agreement members, so they are spared of some bureaucracy issues regarding official documents for travel and stay, which could in turn generate less stress compared to students from other non-European states. The study sample was small and the study design was cross-sectional. Also, the questionnaire was in English; all assessed students study in English, but with few exceptions this is not the first language of participants.
The originality of the study consists in the fact that it addresses the relationship between perceived stress and well-being in a sample of foreign medical students by gender, geographical area of origin and religiosity. A larger sample, an assessment of number and type of stress factors, paired with measures of personality and coping mechanisms and a prospective study design may provide a comparative assessment of factors mediating stress and well-being before and after the onset of the medical training. Further data on how these factors combined with coping mechanisms impact well-being may support specific mental health prevention strategies for this academic population.
Conclusions
The current study supports that the negative relationship between perceived stress and well-being of first year international medical students in Romania is mediated by gender and non-European origin. Our study did not ascertain any difference regarding the relationship between perceived stress and well-being of religious vs. non-religious first year international medical students in Romania.
Acknowledgment
The authors wish to thank the students who participated in this study.
Bibliografie
- Yusoff MSB, Abdul Rahim AF, Baba AA, Ismail SB, Mat Pa MN, Esa AR. The impact of medical education on psychological health of students: a cohort study. Psychol Health Med. 2013;18(4):420–30.
- Kulsoom B, Afsar NA. Stress, anxiety, and depression among medical students in a multiethnic setting. Neuropsychiatr Dis Treat. 2015;11:1713–22.
- Rosiek A, Rosiek-Kryszewska A, Leksowski Ł, Leksowski K. Chronic Stress and Suicidal Thinking Among Medical Students. Int J Environ Res Public Health. 2016;13(2):212.
- Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354–73.
- Wege N, Muth T, Li J, Angerer P. Mental health among currently enrolled medical students in Germany. Public Health. 2016;132:92-100.
- Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, Turin TC. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015;11(1):69–74.
- Johnson KM, Simon N, Wicks M, Barr K, O’Connor K, Schaad D. Amount of Sleep, Daytime Sleepiness, Hazardous Driving, and Quality of Life of Second Year Medical Students. Acad Psychiatry [online] 2017 [cited 2017 May]. Doi: 10.1007/s40596-017-0668-6. Available from: URL: https://link.springer.com/article/10.1007%2Fs40596-017-0668-6.
- Hardeman R, Perry S, Phelan SM, Przedworski JM, Burgess DJ, van Ryn M. Racial identity and mental well-being: The experience of African American Medical Students: A Report from the Medical Student CHANGE Study. J Racial Ethn Health Disparities. 2016;3(2):250–8.
- Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50(4):456-68.
- Brazeau CM, Shanafelt T,Durning SJ, Massie FS, Eacker A, Moutier C, Satele DV, Sloan JA, Dyrbye LN. Distress Among Matriculating Medical Students Relative to the General Population. Acad Med. 2014;89(11):1520-5.
- Goebert D, Thompson D, Takeshita J, Beach C, Bryson P, Ephgrave K, Kent A, Kunkel M, Schechter J, Tate J. Depressive symptoms in medical students and residents: a multischool study. Acad Med. 2009;84:236–41.
- Mahmoud JS, Staten R, Hall LA, Lennie TA. The Relationship among Young Adult College Students’ Depression, Anxiety, Stress, Demographics, Life Satisfaction, and Coping Styles. Issues Ment Health Nurs. 2012;33:149–56.
- Chowdhury R, Mukherjee A, Mitra K, Naskar S, Karmakar PR, Lahiri SK. Perceived psychological stress among undergraduate medical students: Role of academic factors. Indian J Public Health. 2017;61(1):55-7.
- Yamada Y, Klugar M, Ivanova K, Oborna I. Psychological distress and academic self- perception among international medical students: the role of peer social support. BMC Med Educ. 2014;14:256.
- Smith CK, Peterson DF, Degenhardt BF, Johnson JC. Depression, anxiety, and perceived hassles among entering medical students. Psychol Health Med. 2007;12(1):31-9.
- Buzoianu AD, Popescu CA, Suciu S, Armean SM. Correlates of depression, anxiety and stress among foreign medical students studying general medicine in Romania. Eur Psychiatry. 2016;33:S230.
- Poyrazli S, Lopez MD. An exploratory study of perceived discrimination and homesickness: a comparison of international students and American students. J Psychol. 2007;141(3):263-80.
- Huhn D, Huber J, Ippen FM, Eckart W, Junne F, Zipfel S, Herzog W, Nikendei C. International medical students’ expectations and worries at the beginning of their medical education: a qualitative focus group study. BMC Med Educ. 2016;16:33.
- Riemenschneider H, Balázs P, Balogh E, Bartels A, Bergmann A, Cseh K, Faubl N, Füzesi Z, Horváth F, Kiss I, Schelling J, Terebessy A, Voigt K. Do socio-cultural factors influence medical students’ health status and health-promoting behaviors? A cross-sectional multicenter study in Germany and Hungary. BMC Public Health. 2016;16:576.
- Chen YL, Liu MC, Tsai TW, Chen YH. Religious practices in cross-cultural contexts: Indonesian male science students’ adjustment in Taiwan. J Couns Psychol. 2015;62(3):464-75.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health SocBehavi. 1983;24:386-96.
- Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother Psychosom. 2015;84:167–76.
- Al-Sowygh ZH. Academic distress, perceived stress and coping strategies among dental students in Saudi Arabia. Saudi Dent J. 2013;25(3):97–105.
- Tavakoli Z, Montazeri A, Farshad AA, Lotfi Z, Hassim IN. Sources of Stress and Coping Strategies among Iranian Physicians. Glob J Health Sci. 2017;9(1):120-9.
- Balboni MJ, Bandini J, Mitchell C, Epstein-Peterson ZD, Amobi A, Cahill J, Enzinger AC, Peteet J, Balboni T. Religion, Spirituality, and the Hidden Curriculum: Medical Student and Faculty Reflections. J Pain Symptom Manage. 2015;50(4):507-15.
- Lee Y. The relationship of spiritual well-being and involvement with depression and perceived stress in Korean nursing students. Glob J Health Sci. 2014;6(4):169-76.
- Slavin SJ, Schindler DL, Chibnall JT. Medical Student Mental Health 3.0: Improving Student Wellness Through Curricular Changes. Acad Med. 2014;89(4):573-7.
- Farrer L, Gulliver A, Chan JK, Batterham PJ, Reynolds J, Calear A, Tait R, Bennett K, Griffiths KM. Technology-Based Interventions for Mental Health in Tertiary Students: Systematic Review. J Med Internet Res. 2013;15(5):e101.
- Ranasinghe P, Wathurapatha WS, Mathangasinghe Y, Ponnamperuma G. Emotional intelligence, perceived stress and academic performance of Sri Lankan medical undergraduates. BMC Med Educ. 2017;17:41.
- Bond KS, Jorm AF, Kitchener BA, Reavley NJ. Mental health first aid training for Australian medical and nursing students: an evaluation study. BMC Psychology. 2015;3(1):11.
Articole din ediţiile anterioare
Nevoi de sănătate mintală pentru o construcţie corectă a managementului psihiatriei instituţionale şi comunitare
Sănătatea mintală este un domeniu important al sănătăţii publice, impactul tulburărilor psihice fiind costisitor pentru societate. De aceea trebuie...
Trauma – experienţa individuală, contextul şi trasee de dezvoltare
Acest articol trece în revistă definiţiile furnizate de-a lungul timpului pentru unele concepte specifice asociate cu expunerea la adversităţi, pre...
Modele teoretice actuale ale sănătăţii mintale
Formularea definiţiilor sănătăţii mintale şi ale tulburărilor mintale are consecinţe majore în domeniile sociale şi financiare, din moment ce perso...
Alianţa Română de Psihiatrie şi Psihoterapie, între memorii, propuneri, speranţe…
Acordarea de îngrijiri psihiatrice de înaltă calitate pacienţilor, în special în cadrul Uniunii Europene, este o obligaţie a statului, o datorie a ...