The prophylaxis of neurological impairment of premature born infants remains a serious challenge for the neonatologists. The administration of drugs with neuroprotective effect should be considered in order to reduce the risk of cerebral palsy after severe preterm birth. Magnesium sulfate (MgSO4), the objective of this analysis, has been proposed as an important part of the management of unavoidable preterm birth for the prevention of cerebral palsy and neonatal death. The beneficial effects of this inexpensive and simple treatment are observed regardless of the reason for preterm birth, with similar results on different premature gestational ages. MgSO4 has been shown to have a neuroprotective effect by reducing brain metabolism and has also a beneficial hemodynamic effect by stabilizing blood pressure, reducing constriction in the cerebral arteries, and restoring infusion in preterm infants. The administration of MgSO4 should be considered for every patient with gestational age between 23+0 and 31+6 gestational weeks, with high probability of preterm birth within the next 12 hours, premature rupture of membranes before term, or cervical incompetence with high probability of birth within 12 hours. There are two standard regiment proposed: the first one recommends the intravenous administration of MgSO4 on automatic syringe, 4 g during 20 minutes, followed by the administration of 1 g/h until birth or for 24 hours. The second protocol recommends the administration of 6 g of MgSO4 intravenously for 20-30 minutes, followed by a maintenance infusion of 2 g/h. If the birth did not occur after 12 hours and is no longer considered imminent birth, the infusion stops and resumes in case of recurrence of the imminent birth. Both protocols are demonstrated to be efficient, with no maternal side effects.
Prevenirea paraliziei cerebrale la sugarii prematuri - rolul potenţial al sulfatului de magneziu
The prevention of cerebral palsy in preterm infants – the potential role of magnesium sulfate
First published: 17 decembrie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.67.4.2019.2764
Abstract
Rezumat
Profilaxia deficienţei neurologice a nou-născuţilor prematuri rămâne o provocare pentru neonatologi. Administrarea medicamentelor cu efect neuroprotector trebuie luată în considerare pentru a reduce riscul de paralizie cerebrală după naşterea prematură severă. Sulfatul de magneziu (MgSO4), obiectivul acestei analize, a fost propus ca parte importantă a managementului naşterii premature inevitabile pentru prevenirea paraliziei cerebrale şi a morţii neonatale. Efectele benefice ale acestui tratament ieftin şi simplu sunt observate indiferent de motivul naşterii premature, cu rezultate similare la diferite vârste de gestaţie premature. S-a dovedit că MgSO4 are un efect neuroprotector prin reducerea metabolismului creierului şi, de asemenea, are efecte hemodinamice benefice prin stabilizarea tensiunii arteriale, reducerea constricţiei în arterele cerebrale şi restabilirea circulaţiei cerebrale la copiii prematuri. Administrarea de MgSO4 trebuie luată în considerare pentru fiecare gravidă cu vârsta gestaţională între 23+0 şi 31+6 săptămâni de gestaţie, cu probabilitate ridicată de naştere prematură în următoarele 12 ore, cu ruperea prematură a membranelor înainte de termen sau cu incompetenţă cervicală cu probabilitate mare de naştere în termen de 12 ore. Există două regimuri standard propuse. Primul recomandă administrarea intravenoasă de MgSO4 pe seringă automată, 4 g în 20 de minute, urmată de administrarea de 1 g/oră până la naştere sau pentru 24 de ore. Al doilea protocol recomandă administrarea intravenoasă a 6 g de MgSO4 timp de 20-30 minute, urmată de o perfuzie de întreţinere de 2 g/oră. Dacă naşterea nu a avut loc după 12 ore şi nu mai este considerată naştere iminentă, perfuzia se opreşte şi se reia în caz de reapariţie a riscului de naştere iminentă. Ambele protocoale sunt dovedite a fi eficiente, fără efecte secundare materne.
Introduction
Brain lesions of preterm newborns (periventricular leukomalacia, intraventricular/parenchymal hemorrhage, lesions of the white matter) remain an important health care problem, that can lead later in childhood to cerebral palsy (CP) and to neurodevelopmental disorders(1). The mechanisms involved can imply both inflammation and ischemic injury. A percentage of 4 up to 10% of preterms can develop cerebral palsy, even in the absence of patent brain injury at birth. On the other hand, up to 96% of premature infants with cerebral palsy have brain lesions detectable in the early postnatal period by transfontanelar ultrasound(2).
The most commonly involved risk factors for CP are: the presence of genetic abnormalities (such as maternal mental retard or congenital birth defects), birth weight <2000 grams, birth before 32 gestational weeks (GW), and prenatal infection(3-6). Other causes of CP include: fetal anemia, intrauterine transfusions, or fetal alcohol syndrome(4,5). However, preterm birth remains the most important risk factor(3).
In some countries, the incidence of CP has increased in recent years due to improved medical care of the small premature infants, thus increasing their survival rate, but not their neurological prognosis(7). Various studies associate severe intraventricular hemorrhage and periventricular leukomalacia with CP(8).
The cerebral vascular anatomy prior to week 32 of gestation consists of two systems with no anastomoses between them: the ventriculopetally system (which irrigates the cortex) and the ventriculofugal system (it descends to the ventricles). The area between these two systems is vulnerable to ischemia. Due to the fact that through this area pass the pyramidal tracts, an ischemic lesion at this level may cause spastic diplegia(9).
After 32 GWs, the cerebral blood flow is oriented towards the cortex. Therefore, hypoxic lesions occurring after this age will primarily affect the cortical regions of the brain.
Other studies claim that fetal infection may be an important element in the relationship between preterm birth and CP(10). Antenatal infection of the genitourinary tract determines the production of proinflammatory cytokines (IL1, IL6, IL8, TNF) that stimulate prostaglandin production and induce preterm labor(11). The same cytokines have also direct toxic effects on oligodendrocytes and myelin(12).
Vascular rupture, tissue hypoxia, and cytokine-mediated destructions determine a massive neuronal apoptosis. As a consequence, the released glutamate acts upon membranar receptors, allowing the influx of calcium into the neurons cytoplasm. Intracellular hypercalcemia itself has a toxic effect upon white matter. Moreover, glutamate has a direct toxic action on oligodendrocytes(11-13).
Therefore, prospective research has been conducted in order to identify a potential profilactic drug with neuroprotective effect that can reduce the risk of neurodevelopmental disorders of preterms, magnesium sulfate (MgSO4) studies being promising(13). In term of cell biology, neuroprotection translates the inhibition of the biochemical response to ischemia in order to prevent neuronal death.
The role and distribution of magnesium
in the human body
Magnesium is the fourth most widespread ion in the body and contributes to several physiological processes, including cellular and energetic metabolism(14).
Within the human brain, magnesium is mainly linked to chelators such as adenosine triphosphate (ATP) and is a cofactor in more than 300 enzymatic reactions. Magnesium ions are essential for DNA, RNA and protein synthesis. Magnesium also contributes to glycolysis and ATP production, acting as a membranar cell stabilizer(14). In the central nervous system, magnesium acts as a non-competitive blocker of N-methyl-D-aspartate (NMDA) glutamate receptor, modulating calcium influx and preventing excitotoxic injury caused by it. In ischemic conditions, the level of extracellular glutamate decreases, possibly reducing excitotoxicity(15). Magnesium limits calcium influx through voltage-dependent channels, which may reduce apoptosis activation(16).
Magnesium has also intrinsic anti-inflammatory properties, reducing both oxidative stress and the production of pro-inflammatory cytokines: interleukin-6 (IL6) and tumor necrosis factor-a (TNF-a)(17). Magnesium deficiency increases the production of endothelial nitric oxide, which can promote endothelial dysfunction. The exact pathways involved are multiple: decreased calcium influx and phagocyte cell activation, inhibition of neurotransmitter release, or inhibition of nuclear factor kappa B. Its physiological role as a calcium channel blocker and modulator of sodium and potassium flux through its action on ion pumps (e.g., Na +/K+ ATPase) and other membrane receptors (e.g., nicotinic acetylcholine receptor) cause it to intervene in muscle contraction, maintaining vascular tone and driving nerve impulse(16).
The normal concentration of magnesium in adult plasma is 0.75 mmol/L. In newborns, magnesium concentrations increases in the first week after birth (0.91 mmol/L)(18).
The transplacental passage of MgSO4
Fetuses are exposed passively to MgSO4 administered to pregnant women. In animals, the concentration of magnesium in fetal blood increases after maternal administration and has a positive correlation with maternal blood levels(19).
The neuroprotective effects of MgSO4
demonstrated in preclinical studies
Since 1980, animal studies have been conducted to investigate the neuroprotective role of magnesium. Early experiments involved adult animal models.
In 1984, Vacanti and Ames demonstrated the neuroprotective effects of MgSO4 in a model of ischemia of the spinal cord in rabbits(20). In 1987, the administration of MgSO4 to rat hippocampal slices reduced the effect of hypoxia(21). McIntosh et al. demonstrated in 1989 that post-traumatic injection of MgSO4 reduced neurological disorders in a dose-dependent manner(22), and in 1996 Marinov et al. showed that the administration of MgSO4 before a focal ischemic episode in rats could be neuroprotective by blocking NMDA receptors(23). Several studies have reported the importance of intraperitoneal administration of MgSO4 in reducing excitotoxic brain injury in mice, lesions induced by intracerebral injection of ibotenate (a glutamate receptor agonist)(24).
Under hypoxic conditions (5-7% inspired oxygen fraction) in the brains of pigs, MgSO4 administration prevented hypoxia-induced changes in neuronal nuclear membrane function, which reduced apoptotic protein transcription and kinase activity. These effects ultimately prevented programmed cell death(25).
The neuroprotective effect of MgSO4 was also evaluated under inflammatory conditions. In pregnant female rats, lipopolysaccharide-induced inflammation (LPS) affected offspring’s learning capacity and memory capacity at 3 months, which were improved by prenatal treatment with MgSO4(26). In a hypoxic-ischemic injury model, in vitro, MgSO4 was involved in the protection of oligodendrocytes(27).
MgSO4 effects on cerebral blood flow
velocities in premature infants
The developing fetal brain is mainly dependent on sustained blood flow due to the lack of its own nutrient reserves. In the immature brain, the thin peripheral vessels do not have many collaterals or anastomoses, and their walls are immature. Thus, they cannot sustain efficient blood flow, and their limited vasodilation capacity cannot compensate for hypoxic-ischemic injury(27).
Exposure to antenatal magnesium sulfate (MgSO4) and increased concentrations of serum magnesium were associated with a decrease in the incidence of hypoxic brain injury(29).
The biochemical cascade during ischemia is initiated due to impaired microcirculation. Thus, its conservation would have a neuroprotective effect. MgSO4 has been shown to have beneficial hemodynamic effects by stabilizing blood pressure, reducing constriction in the cerebral arteries, and restoring infusion in preterm infants(30).
Cerebral blood flow velocity has been validated as a reliable indicator of brain circulation, and flow changes are assumed to play a key role in the development of different brain lesions in premature infants.
Based on these findings, E.Y. Imamoglu and colleagues developed a study to determine whether magnesium sulfate influences the blood flow rate to the brain(31). The prospective study included 53 newborns, between 26-34 weeks of gestation, 20 of whom were exposed to antenatal MgSO4 (their mothers received antenatal MgSO4, either for preeclampsia, or to induce tocolysis). Mean blood flow velocity measurements were performed on the left and right middle cerebral arteries on days 1, 2, 3, 4 and 5 of life. All measurements were performed after the first 8-12 hours of life to reduce the possible effects of immediate postnatal cardiovascular adaptation on flow data. Doppler measurements of flow through the middle cerebral arteries were performed at the level of the anterolateral fontanel (time window). The study also included a detailed ultrasound scan of the neonatal brain. The degree of intraventricular hemorrhage was reported according to the criteria of Papile et al.(32) Study results showed that the average blood velocity in the medium cerebral artery was significantly increased in the neonates who had previously received MgSO4 compared to the controls. There were no differences in the patency of the arterial duct between the two groups. The authors concluded that one of the possible mechanism of MgSO4 protective effect for hypoxic-ischemic events is represented by the increment of cerebral blood flow velocity.
MgSO4 effects on cerebral oxygen kinetics
Michael J. Stark and colleagues studied the effects of antenatal administration of MgSO4 upon oxygen delivery, consumption and extraction in preterm infants versus control preterms(33). Blood flow measured at the level of internal carotid arteries and the release of oxygen at the cerebral level did not differ between the two groups, at the three moments of the study (24, 48, and 72 hours). In contrast, brain oxygen consumption and cerebral fractional tissue oxygen extraction (cFTOE) were lower in infants exposed antenatally to MgSO4 (p=0.012) compared to infants who were not exposed in the first 24 hours after birth, but the difference did not persist either at 48, or after 72 hours. It was also observed that fewer infants in the group receiving MgSO4 developed peri-/intraventricular hemorrhage within the first 72 hours postnatally (p=0.03). The authors concluded that another mechanism though which MgSO4 can exerts its neuroprotective effect is the reduction of brain metabolism. Focusing mainly on oxygen kinetics at the cerebral level after exposure to prenatal MgSO4, this study did not aim to describe the mechanisms by which brain oxygen consumption and its extraction were altered. MgSO4 is known to rapidly cross the placenta and the blood-brain barrier, blocking N-methyl-D-aspartate receptors and glutamate receptors (receptors involved in neuronal death during hypoxic-ischemic injury)(33).
Animal studies indicate that cerebral oxygen consumption is increased after exposure to inflammation in utero. Therefore, protection against inflammatory processes given by MgSO4 may be manifested by reduced brain oxygen consumption and reduced cFTOE(34).
Anti-inflammatory effects of MgSO4
The neuroprotective effect of MgSO4 is considered to be multifactorial, although the specific molecular mechanism remains unknown.
Magnesium reduces excitotoxic lesions, can regulate uteroplacental blood flow, decrease cerebral vascular resistance, and increase cerebral blood flow(35). In contrast, Mg deficiency is associated with inflammation, susceptibility to injury by reactive oxygen species and impaired energy metabolism, all of which play a role in fetal neuronal injury.
Chorioamniotitis is known to be associated with an increased risk of cerebral palsy in both term and preterm infants(35). In complicated pregnancies with intrauterine infection, the inflammatory reaction in the fetus starts at the level of the umbilical vein and can spread, generating a fetal inflammatory response syndrome (FIRS)(36). Endothelial cells are important mediators of signaling, initiating and propagating inflammatory and immune responses, and are an integral part of sepsis pathogenesis.
The P2X7 receptor (P2X7R) belongs to a family of receptors that contain seven members (P2X1-7)(37). These receptors are abundant in the endothelium, in the immunity involved cells, and in the central nervous system. Human umbilical vein endothelial cells (HUVECs) express only P2X4R and P2X7R, of which only P2X7R are functional(38).
Lipopolysaccharides (LPS), components of the outer membrane of Gram-negative bacteria, through the Toll-4 receptor (TLR4), activate a number of intracellular pathways, leading to pro-IL-1b transcription, while ATP secreted from damaged cells stimulates P2X7R, which will activate various mechanisms that result in the secretion of mature IL-1b. This increases the flow of intracellular ATP and, together with IL-1b, increases inflammation through a vicious circle. IL-1b plays a central role in inflammation-induced fetal brain injury, and its effects can be attenuated through an IL-1 receptor antagonist(39).
In other to investigate the role of MgSO4 in inflammation, Mide Ozen et al. conducted a study in which they used HUVECs (human umbilical vein endothelial cells) cultures and treated them with different doses of LPS, adenosine-5’-triphosphate, and MgSO4 for 3 or 24 hours. After that, they determined cell cytotoxicity, apoptosis, IL-1b mRNA expression, IL-1b production and secretion, and P2X7R expression on these cells(40).
The study results demonstrated that the anti-inflammatory effect of MgSO4 is achieved by the downregulation of P2X7R expression. Furthermore, the study demonstrated that MgSO4 is effective in blocking IL-1b-mediated inflammation in HUVECs in both the initiation and propagation phases of inflammation, effects mediated also by P2X7R. In addition, the data obtained from this study suggest that the attenuation of the inflammatory lesion is dose dependent on MgSO4 used, so that higher doses (10 mM) are significantly better in inhibiting IL-1b production.
Observational studies that demonstrate
the neuroprotective effect of magnesium sulfate in neonates
Given its use in obstetrics for various maternal disorders, its transplacental passage and its neuroprotective action observed in animal studies, several observational studies have focused on the impact of MgSO4 on neurological outcomes in preterm infants.
There are data in literature which reveal that newborns of very low birth weight whose mothers were treated with magnesium sulfate for preterm labor or preeclampsia have a low incidence of CP at 3 years(41).
Randomized studies were designed to investigate the hypothesis that magnesium sulfate would have neuroprotective effects on the fetus.
Crowther and colleagues conducted a randomized study in which they enrolled 1063 patients with an imminent risk (birth was planned or expected within 24 hours) of birth before 30 weeks of gestation(42). Patients were given magnesium sulfate or placebo. The results of the study showed that the rate of neonatal death and cerebral palsy were lower in the group treated with magnesium sulfate, in the absence of any serious adverse effect(42).

BEAM was a placebo-controlled study on a sample of randomized 2241 pregnant women with an imminent risk of preterm birth between 24 and 31 weeks. About 87% had premature rupture membranes and about 1/5 received magnesium sulfate for tocolytic purposes. The study had an excellent follow-up: 96% of the children were monitored up to 2 years. The results of the study revealed that magnesium sulfate infusion prevents CP, regardless of the gestational age at which the therapy is administered(43).
In 2009, Doyle et al. conducted a Cochrane review that contained five randomized trials to evaluate the neuroprotective effects of magnesium sulfate. A total of 6145 children were included, most of them from the largest multicenter studies: Australian, French and the MFMU network. The conclusion was that exposure to magnesium compared to lack of exposure reduced the risk of CP (relative risk of 0.68)(44).
MgSO4 implementation
in neuroprotection-related protocols
In France, in 2015, only 60% of tertiary maternity hospitals used MgSO4 for fetal neuroprotective purposes, with protocols that differed depending on the maximum gestational age, the possibility of resuming administration and monitoring(45).
In Europe, in 2012, only 9 out of 119 tertiary maternities (7.6%) used MgSO4 for fetal neuroprotection. The lack of experience and the absence of a protocol or national guidelines, the environmental contexts or beliefs about the possible consequences seemed to represent barriers to the large-scale application of MgSO4 in women at risk of preterm birth(46).
Studies that evaluated the implementation of MgSO4 protocol showed that almost 70% of eligible women received MgSO4 before preterm birth and about 90% gave birth within the next 24 hours. The main reasons why Mg was not administered were: omission by the medical team and the emergency birth(47).
In an Australian audit, it was shown that the proportion of eligible women who did not receive MgSO4 decreased significantly after the publication of national guidelines, from 69.7% in 2010 to 26.9% in 2011(48).
In Canada, a strategy to update medical knowledge (including national practice guides, online learning modules, barrier assessment, and feasibility studies) was associated with an 84% increase in optimal use of MgSO4. To improve the rates of MgSO4 administration to eligible women, the implementation of educational programs could be effective(49).
In Romania, neuroprotection was introduced starting with the 2019 in the clinical practice guideline for premature birth(50).
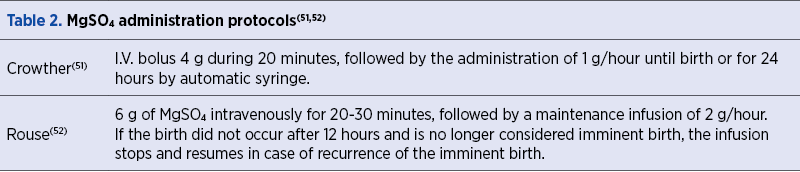
In Table 1 and Table 2, there are presented the main maternal indications and standard protocols for the administration of MgSO4 for neuroprotection.
The protocols efficacy has been proved by two studies(51,52). In the first study realized by Crowther et al., 1062 patients (1255 fetuses) were included, having a gestational age inferior to 30 GW, with imminent birth risk in the next 24 hours(51). The patients were blindly randomized to receive MgSO4 after a protocol depicted in Table 2 or an equal volume of 0.9% saline. The enrolled patients were followed-up to the age of 2 years old. It was found that magnesium sulfate administration decreased the risk of fetal death by 0.81 (95% CI; 0.62±1.07) and the risk of developing cerebral palsy by 0.83 (95% CI; 0.54±1.28) without any maternal side effects.
The second protocol was used by Rouse et al.(51) (Table 2). The patients were also randomized to receive MgSO4 or placebo. The enrolled preterm patients were also followed-up to the age of 2 years old. The magnesium sulfate administration decreased the risk of fetal death by 0.93 (95% CI; 0.62±1.07) and the risk of developing cerebral palsy by 0.93 (95% CI; 0.54±1.28). Again, no maternal side effects were found.
Conclusions
The administration of magnesium sulfate prior to preterm birth for fetal neuroprotection may prevent cerebral palsy and reduce the risk of fetal or infant death. The beneficial effects are observed regardless of the cause of preterm birth, the protective effect being seen regardless the gestational age. We believe that the introduction of such an inexpensive, easy-to-administer treatment with no significant maternal side effects, in the national guidelines, may lead to an important improvement of the preterm infant prognostic and it should be considered a component part of the prenatal prophylactic treatment of preterm infants.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
2. Crowther CA, Middleton PF, Voysey M, Askie L, Duley L, Pryde PG, Marret S, Doyle LW; AMICABLE Group. Assessing the neuroprotective benefits for babies of antenatal magnesium sulphate: An individual participant data meta-analysis. PLoS Med. 2017; 14(10):e1002398. doi: 10.1371/journal.pmed.1002398.
3. Nelson KB, Ellenberg JH. Antecedents of cerebral palsy: multivariate analysis of risk. N Eng J Med. 1986 Jul 10; 315(2):81-6.
4. Lindenburg IT, van Klink JM, Smits-Wintjens EHJ, et al. Long-term neurodevelopmental and cardiovascular outcome after intrauterine transfusions for fetal anaemia: a review. Prenat Diagn. 2013; 33(9):815-22. doi: 10.1002/pd.4152.
5. O’Leary CM, Watson L, D’Antoine H, et al. Heavy maternal alcohol consumption and cerebral palsy in the offspring. Dev Med Child Neurol. 2012; 54(3):224-30. doi: 10.1111/j.1469-8749.2011.04201.
6. Oancea AC, Rotar IR, Dumitru A, Irimescu T, Preda A, Staicu A, Zaharie G, Mureşan D. Analysis of early perinatal morbidity related to preterm birth in a Romanian tertiary obstetrical center. Obstetrica şi Ginecologia. 2018; LXVI, 97-104.
7. Bhasin TK, Brocksen S, Avchen RN, et al. Prevalence of four developmental disabilities among children aged 8 years - metropolitan Atlanta developmental disabilities surveillance program, 1996 and 2000. MMWR Surveill Summ. 2006; 27, 55(1):1-9.
8. Luthy DA, Shy KK, Strickland D, et al. Status of infants at birth and risk for adverse neonatal events and long-term sequelae: a study in low birthweight infants. Am J Obstet Gynecol. 1987; 157(3):676-9.
9. Menshawi K, Mohr JP, Gutierrez J. A Functional Perspective on the Embryology and Anatomy of the Cerebral Blood Supply. J Stroke. 2015; 17(2): 144–158.
10. Burd I, Balakrishnan B, Kannan S. Models of fetal brain injury, intrauterine inflammation, and preterm birth. Am J Reprod Immunol. 2012; 67(4):287-94.
11. Oka A, Belliveau MJ, Rosenberg PA, et al. Vulnerability of oligodendroglia to glutamate: pharmacology, mechanism, and prevention. J Neurosci. 1993; 13(4): 1441–1453.
12. Schmidt AN. Dezvoltarea Sistemului Nervos Central. In: Embriologie Specială. Ed. Intelcredo. 2002; p. 249.
13. Kehrer M, Blumenstock G, Ehehalt S, Goelz R, Poets C, Schöning M. Development of Cerebral Blood Flow Volume in Preterm Neonates during the First Two Weeks of Life. Pediatr Res. 2005 Nov; 58(5):927-30.
14. Elin RJ. Assessment of magnesium status. Clin Chem. 1987; 33(11):1965-70.
15. Kang SW, Choi SK, Park E, Chae SJ, Choi S, Jin Joo H, et al. Neuroprotective effects of magnesium-sulfate on ischemic injury mediated by modulating the release of glutamate and reduced of hyperreperfusion. Brain Res. 2011; 1371:121-8.
16. Iseri LT, French JH. Magnesium: nature’s physiologic calcium blocker. Am Heart J. 1984; 108:188–93.
17. Mazur A, Maier JAM, Rock E, Gueux E, Nowacki W, Rayssiguier Y. Magnesium and the inflammatory response: potential physiopathological implications. Arch Biochem Biophys. 2007 458:48–56.
18. Rigo J, Pieltain C, Christmann V, Bonsante F, Moltu SJ, Iacobelli S, et al. Serum magnesium levels in preterm infants are higher than adult levels: a systematic literature review and meta-analysis. Nutrients. 2017; 16, 9(10). pii: E1125. doi: 10.3390/nu9101125.
19. Hallak M, Cotton DB. Transfer of maternally administered magnesium sulfate into the fetal compartment of the rat: assessment of amniotic fluid, blood, and brain concentrations. Am J Obstet Gynecol. 1993; 169(2 Pt 1):427-31.
20. Vacanti FX, Ames A III. Mild hypothermia and Mg++ protect against irreversible damage during CNS ischemia. Stroke. 1984; 15:695–8.
21. Clark GD, Rothman SM. Blockade of excitatory amino acid receptors protects anoxic hippocampal slices. Neuroscience. 1987; 21:665–71.
22. McIntosh TK, Vink R, Yamakami I, Faden AI. Magnesium protects against neurological deficit after brain injury. Brain Res. 1989; 482:252–60.
23. Marinov MB, Harbaugh KS, Hoopes PJ, Pikus HJ, Harbaugh RE. Neuroprotective effects of preischemia intraarterial magnesium sulfate in reversible focal cerebral ischemia. J Neurosurg. 1996; 85:117–24.
24. Marret S, Gressens P, Gadisseux JF, Evrard P. Prevention by magnesium of excitotoxic neuronal death in the developing brain: an animal model for clinical intervention studies. Dev Med Child Neurol. 1995; 37:473–84.
25. Mami AG, Ballesteros JR, Fritz KI, Kubin J, Mishra OP, Delivoria-Papadopoulos M. Effects of magnesium sulfate administration during hypoxia on CaM kinase IV and protein tyrosine kinase activities in the cerebral cortex of newborn piglets. Neurochem Res. 2006; 31:57–62.
26. Lamhot VB, Khatib N, Ginsberg Y, Anunu R, Richter-Levin G, Weiner Z, et al. Magnesium sulfate prevents maternal inflammation-induced impairment of learning ability and memory in rat offspring. Am J Obstet Gynecol. 2015; 213:851.e1–8.
27. Itoh K, Maki T, Shindo A, Egawa N, Liang AC, Itoh N, et al. Magnesium sulfate protects oligodendrocyte lineage cells in a rat cell-culture model of hypoxic-ischemic injury. Neurosci Res. 2016; 106:66–9.
28. Imamoglu EY, Gursoy T, Karatekin G, Ovali F. Effects of antenatal magnesium sulfate treatment on cerebral blood flow velocities in preterm neonates.
J Perinatol. 2014; 34(3):192-6. doi: 10.1038/jp.2013.182.
29. Ilves P, Blennow M, Kutt E, Magi ML, Kudrjavtseva G, Lagercrantz H, et al. Concentrations of magnesium and ionized calcium in umbilical cord blood in distressed term newborn infants with hypoxic-ischemic encephalopathy. Acta Paediatr. 1996; 85(11): 1348–1350.
30. de Haan HH, Gunn AJ, Williams CE, Heymann MA, Gluckman PD. Magnesium sulfate therapy during asphyxia in near-term fetal lambs does not compromise the fetus but does not reduce cerebral injury. Am J Obstet Gynecol. 1997; 176 (1 Pt 1):18-27.
31. Imamoglu EY, Gursoy T, Karatekin G, Ovali F. Effects of antenatal magnesium sulfate treatment on cerebral blood flow velocities in preterm neonates. Journal of Perinatology. 2014; 34, 192–196.
32. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978; 92(4): 529–534.
33. Stark MJ, Hodyl NA, Andersen CC. Effects of antenatal magnesium sulfate treatment for neonatal neuroprotection on cerebral oxygen kinetics. Pediatr Res. 2015; 78(3):310-4.
34. Andersen CC, Pillow JJ, Gill AW, et al. The cerebral critical oxygen threshold of ventilated preterm lambs and the influence of antenatal inflammation. Journal of Applied Physiology. 2011; 111:775-81.
35. Hirtz DG, Nelson K. Magnesium sulfate and cerebral palsy in premature infants. Curr Opin Pediatr. 1998; 10, 131–137.
36. Kim CJ, et al. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol. 2015; 213, S29–S52.
37. Di Virgilio F, Dal Ben D, Sarti AC, Giuliani AL, Falzoni S. The P2X7 receptor in infection and inflammation. Immunity. 2017; 18;47(1):15-31.
38. Wilson HL, et al. P2X receptor characterization and IL-1/IL-1Ra release from human endothelial cells. Br J Pharm. 2007; 151, 115–127.
39. Leitner K, et al. IL-1 receptor blockade prevents fetal cortical brain injury but not preterm birth in a mouse model of inflammation-induced preterm birth and perinatal brain injury. Am J Reprod Immunol. 2014; 71, 418–426.
40. Ozen M, Xie H, Shin N, Al Yousif G, Clemens J, McLane MW, et al. Magnesium sulfate inhibits inflammation through P2X7 receptors in human umbilical vein endothelial cells. Pediatr Res. 2019; doi: 10.1038/s41390-019-0557-7. [Epub ahead of print]
41. Grether JK, Nelson KB. Possible decrease in prevalence of cerebral palsy in premature infants. J Pediatr. 2000; 136(1):133.
42. Crowther CA, Hiller JE, Doyle LW, Haslam RR, Australasian Collaborative Trial of Magnesium Sulphate Collaborative G. Effect of magnesium sulfate given for neuroprotection before preterm birth: a randomized controlled trial. JAMA. 2003; 290(20):2669-76.
43. Rouse DJ, Hirtz DG, Thom E, Varner MW, Spong CY, Mercer BM, et al. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N Engl J Med. 2008; 359(9):895-905.
44. Doyle LW, Crowther CA, Middleton P, Marret S, Rouse D. Magnesium sulphate for women at risk of preterm birth for neuroprotection of the fetus. Cochrane Database Syst Rev. 2009; 21 (1):CD004661. doi: 10.1002/14651858.CD004661.pub3. Review.
45. Chollat C, Le Doussal L, de la Villéon G, Provost D, Marret S. Antenatal magnesium sulphate administration for fetal neuroprotection: a French national survey. BMC Pregnancy Childbirth. 2017; 17:304.
46. Bain E, Bubner T, Ashwood P, Van Ryswyk E, Simmonds L, Reid S, et al. Barriers and enablers to implementing antenatal magnesium sulphate for fetal neuroprotection guidelines: a study using the theoretical domains framework. BMC Pregnancy Childbirth. 2015; 18;15:176. doi: 10.1186/s12884-015-0618-9.
47. Ow LL, Kennedy A, McCarthy EA, Walker SP. Feasibility of implementing magnesium sulphate for neuroprotection in a tertiary obstetric unit. Aust NZJ Obstet Gynaecol. 2012; 52:356–60.
48. Siwicki K, Bain E, Bubner T, Ashwood P, Middleton P, Crowther CA. Nonreceipt of antenatal magnesium sulphate for fetal neuroprotection at the Women’s and Children’s Hospital, Adelaide 2010-2013. Aust NZJ Obstet Gynaecol. 2015; 55:233–8.
49. De Silva DA, Synnes AR, von Dadelszen P, Lee T, Bone JN; MAG-CP, CPN and CNN Collaborative Groups, Magee LA. MAGnesium sulphate for fetal neuroprotection to prevent Cerebral Palsy (MAG-CP)-implementation of a national guideline in Canada. Implement Sci. 2018; 13(1):8. doi: 10.1186/s13012-017-0702-9.
50. Seria ghiduri clinice pentru Obstetrică şi Ginecologie. Naşterea înainte de termen. https://sogr.ro/wp-content/uploads/2019/02/Na-terea-%C3%83%C2%AEnainte-de-termen.pdf. downloaded on 13.12.2019
51. Crowther CA, Hiller JE, Doyle LW, Haslam RR. Effect of magnesium sulfate given for neuroprotection before preterm birth: a randomized controlled trial. JAMA. 2003; 290(20):2669±76. https://doi.org/10. 1001/jama.290.20.2669 PMID: 14645308.
52. Rouse DJ, Hirtz DG, Thom E, Varner MW, Spong CY, Mercer BM, et al. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N Engl J Med. 2008; 359(9):895±905, doi.org/10.1056/NEJMoa0801187 PMID: 18753646.
Articole din ediţiile anterioare
Evaluarea RMN-ului post-mortem de 7T în comparaţie cu autopsia convenţională: un studiu morfometric
Obiective. Scopul studiului nostru a fost de a stabili dacă RMN-ul post-mortem la 7T poate efectua măsurători tridimensionale ale inimii fetale şi ...
COVID-19 în sarcină – dificultăţi şi progrese
The newly emerging coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is spreading gl...
Consilierea în agenezia ductului venos secundară venei cave inferioare întrerupte
The ultrasound (US) examination of the fetal venous system has exposed a wide spectrum of malformations.
Managementul prenatal şi postnatal în tetralogia Fallot
Anomaliile morfologice ale aparatului cardiovascular reprezintă o cauză majoră de morbiditate şi mortalitate neonatală. O ecografie fetală de rutin...