Leucemie mieloidă acută M1 FAB secundară sindromului mielodisplazic cu exces de blaşti de tip 2
Acute myeloid leukemia M1 FAB secondary to myelodysplastic syndrome with excess blasts type 2
Abstract
Acute myeloid leukemia occurs naturally in the evolution of myelodysplastic syndrome (MDS), typically in MDS with excess blasts type 2. The risk of progression is around 33%. We present the case of an elderly patient who was diagnosed with MDS single dysplasia in 2016. He was treated with erythropoietin. In 2021, the disease evolved into MDS with excess blast type 2 and then in acute myeloid leukemia in a short period of time.Keywords
myelodysplastic syndromeacute myeloid leukemiaexcess blast type 2Rezumat
Leucemia acută mieloidă reprezintă o complicaţie evolutivă a sindromului mielodisplazic, mai ales în cazul mielodisplaziei cu exces de blaşti de tip 2, la care rata de progresie spre leucemie acută atinge un procentaj de 33%. Prezentăm cazul unui pacient vârstnic, diagnosticat cu sindrom mielodisplazic cu displazie unilineală în anul 2016, în tratament cu eritropoietină. În anul 2021, pacientul evoluează spre sindrom mielodisplazic cu exces de blaşti de tip 2, apoi prezintă o evoluţie rapidă spre leucemie acută mieloidă.Cuvinte Cheie
sindrom mielodisplazicleucemie acută mieloidăexces de blaşti de tip 2Introduction
We report the case of a 76-year-old male patient who was diagnosed in 2016 with myelodysplastic syndrome (MDS) single lineage dysplasia, treated with erythropoietin. Since 2018, the patient was lost from the follow-up. He returned in our department in September 2021. The patient has multiple comorbidities, such as nephrological pathologies – chronic urinary infections, operated urinary bladder tumor –, cystectomy with cutaneous ureterostomy and double J stents, along with chronic renal disease on hemodialysis program.
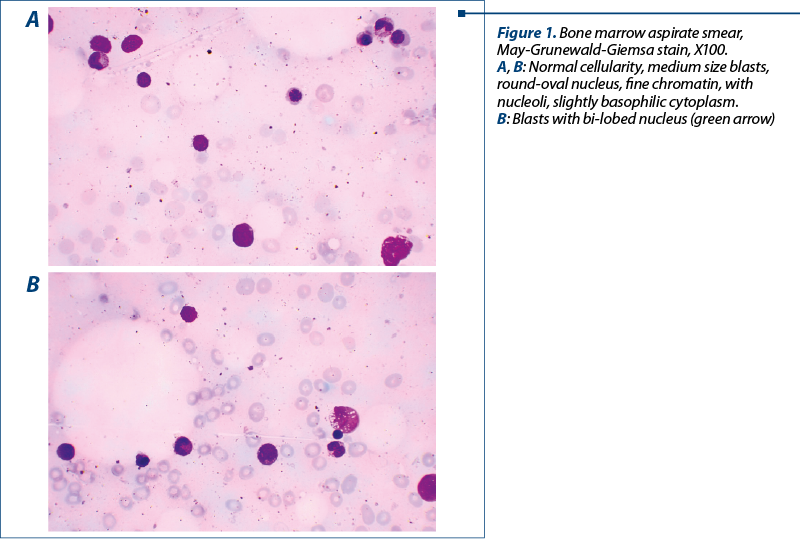
At the end of September 2021, the patient was admitted in our department for pancytopenia. We proceeded with the hematological investigations. The peripheral blood smear was without any blasts. We performed a bone marrow aspiration and biopsy, and both of them showed a medullary infiltrate with 20% blasts (Figure 1), respectively 11-12% blasts. We establish the diagnosis: MDS with excess blast type 2.
After one week, in October 202
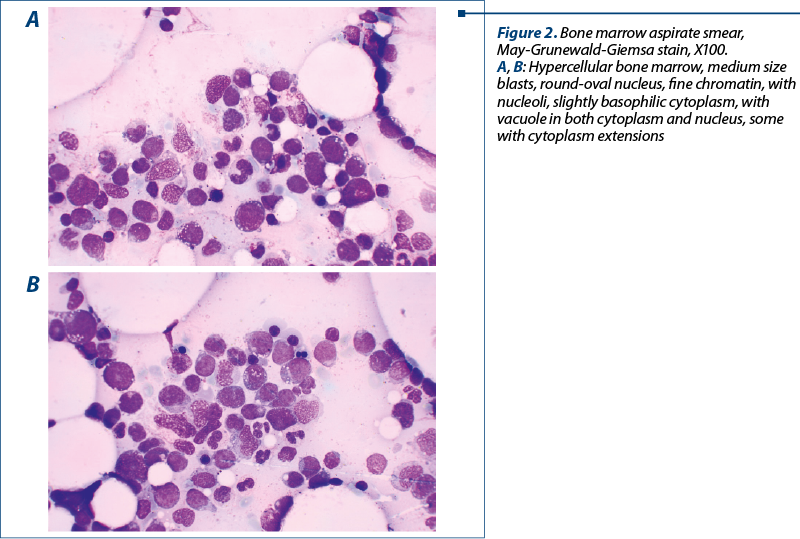
1, the patient came to the emergency unit with asthenia and spontaneous bruises. He was hospitalized in our department. The laboratory tests revealed severe pancytopenia and 6% blasts on the peripheral blood smear. We decided to perform a new medullary aspirate which depicted 73% blasts infiltrate (Figure 2). For a complete diagnosis, we also performed a cytogenetic exam (results not available at the moment) and imunophenotyping by flow cytometry. The flow cytometry revealed the presence of 20% blast with a phenotype suggestive for M1 FAB acute myeloid leukemia: SSC low, CD45 medium, CD34+, CD117+, HLA-DR+/-, cCD3-, CD3-, cCD79-, CD13+, CD11b-, CD36-, CD33+, CD64-, and CD56-. Thus, the progression of the disease was clear and the diagnosis of M1 FAB acute myeloid leukemia post-MDS with excess blasts type 2 was established.
Conclusions
Acute myeloid leukemia occurs in the evolution of MDS, especially in the high-risk types. The prognosis is particularly poor, considering the age, the comorbidities, the clonal evolution and the limited treatment options. We reported the appearance of a MDS case evolving in a full blown picture of acute leukemia in a very short period.
Conflict of interests: The authors declare no conflict of interests.





