The impact of cough on patients and relatives is often underestimated. Patients may need symptomatic treatment when cough is persistent or affects sleep and quality of life. When considering other treatment methods to control cough caused by cancer, there are available for clinicians a variety of pharmacologic agents to relieve cough. Early recognition of cancer-related symptoms can improve management strategies, patient compliance and quality of life.
Tratamentul tusei cronice în cadrul îngrijirilor paliative. O permanentă provocare
Management of chronic cough in palliative care. Always a challenge
First published: 07 martie 2017
Editorial Group: MEDICHUB MEDIA
Abstract
Rezumat
Impactul tusei asupra pacienţilor şi rudelor este adesea subestimat. Pacienţii pot necesita tratament simptomatic când tusea este persistentă sau le afectează somnul şi calitatea vieţii. Înainte de a decide asupra altor tipuri de tratament pentru controlul tusei legate de cancer, clinicienilor le rămâne un spectru larg de agenţi farmacologici cu scopul de a ameliora tusea. Recunoaşterea timpurie a simptomelor legate de cancer poate îmbunătăţi strategiile de tratament, complianţa şi calitatea vieţii pacientului.
Background
1. Incidence
Unlike pain, cough is not a symptom that is being measured regularly in terminal cancer patients. Because of the intermittent nature of the symptom, it may not draw the attention it deserves.Cough is a common symptom in about 23-37% of general cancer patients and in 47-86% of lung cancer patients(1).In the UK, the frequency of cough was 80% in small cell lung cancer and 70% in non-small cell lung cancer. Male patients reported 7% more cough and 12% more haemoptysis than females.
There are other types of cancers in which cough was a frequent symptom: for 22% of patients with colon cancer, for 26% of patients with prostate cancer, for 28% of patients with ovarian cancer and 37% of patients with breast cancer(2).
Cough of moderate to severe intensity occurred in 13% of general cancer patients and in 17-48% of lung cancer patients. Cough can cause distress to cancer patients, although there are few studies that examined it quantitatively; in one series of 240 patients, of whom 21.3% had lung cancer, cough was present in 33%, and among all patients, 13% had moderate to severe cough and 18% of all patients suffered from severe distress due to cough(4).
When is cough in cancer patients a new symptom of the disease? A case-control study on Czech women with newly diagnosed lung cancer published in March 2001 in Lung Cancer Magazine investigated this issue. Chronic cough and sputum for at least three months per year was associated with excess risk only if their duration was less than two years before diagnosis of lung cancer and, therefore, they were suspected of being more likely early symptoms of preclinical lung cancer rather than its cause.
But does cough has prognostic value for the survival of advanced disease cancer patients?
According to a study from January 2010 published in Cancer Magazine, that included a total of 94 patients with advanced non-small cell lung cancer and an Eastern Cooperative Oncology Group performance status of 0 to 2 for those who qualified for chemotherapy, using the M.D Anderson Symptom Inventory before and after their first chemotherapy cycle, apparently it does have. Prognostic values of baseline symptoms and changes in symptom severity were examined by Cox proportional hazard models.
The conclusion of the study was that patients with advanced non-small cell lung cancer during their first line chemotherapy cycle experienced moderate to severe coughing or increased fatigue or shortness of breath, indicating an increased risk for shorter survival.
2. The significance of cough in palliative care setting
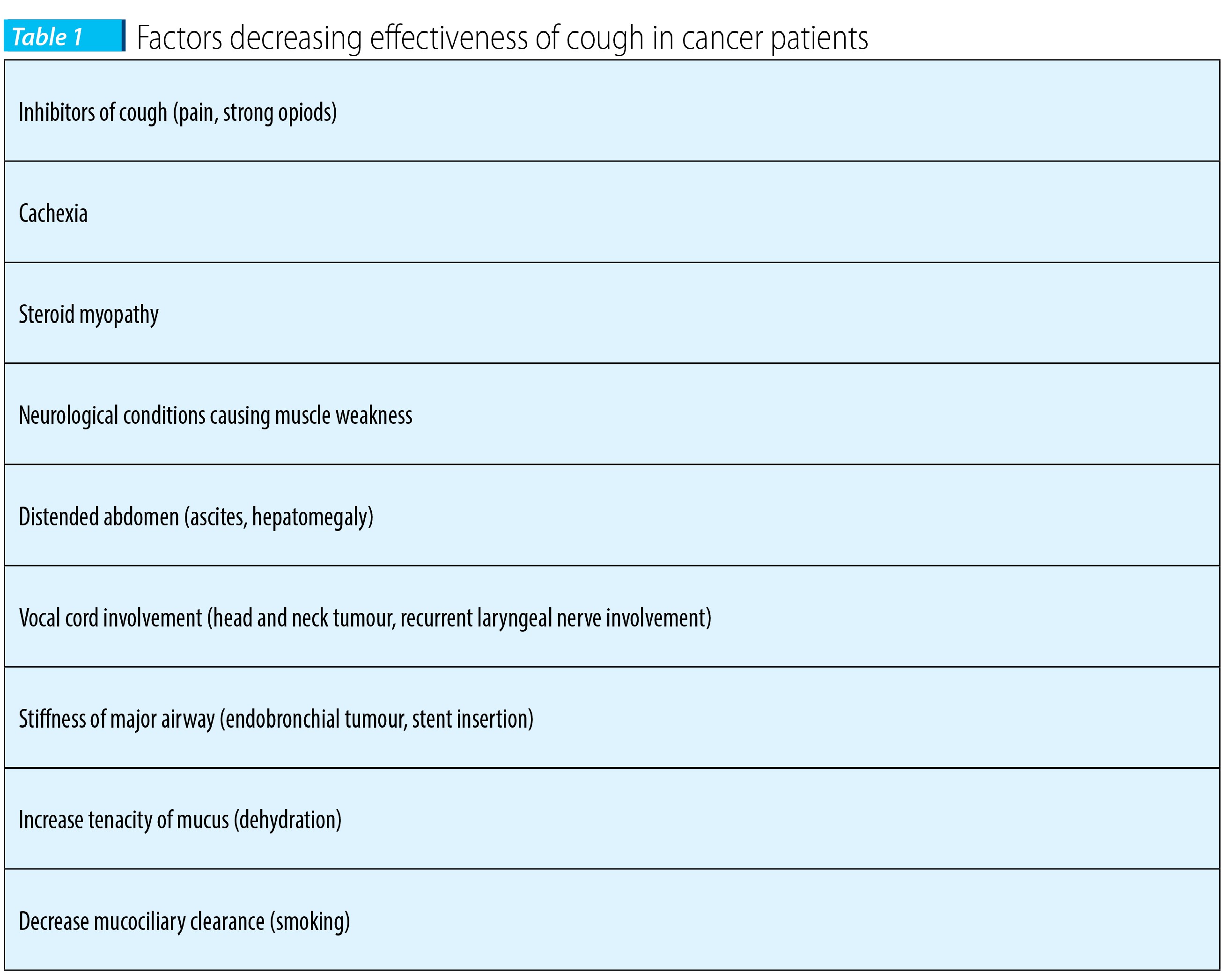
Cough is a complex physiological mechanism that protects the airways and lungs by removing mucus and foreign matter from the larynx, trachea and bronchi. The expulsion is made possible by the high intrathoracic and high airflow velocity generated during the cough reflex(5).In literature, cough is classified as:
- productive cough in a patient able to cough effectively;
- productive cough in a patient not able to cough effectively;
- nonproductive cough.
3. The pathophysiology of cough - neuroanatomy and cough reflex
The cough receptors are widespread in the tracheobronchial tree, but the highest density is in the larynx, trachea and main bronchi. The receptors are also located in the nose, pharynx, paranasal sinus, ears, pleura, diaphragm and pericardium. The cough receptors are stimulated by mechanical stimulus (pressure, deformation, touch), and chemical stimulus (smoke, mucus, endogenous chemical mediators).Impulses travel via the internal laryngeal nerve, a branch of the superior laryngeal nerve which stems from the vagus nerve to the medulla of the brain, that represents the afferent neural pathway.
The efferent neural pathway begins with the signals transmitted from the cerebral cortex and medulla via the vagus nerve and superior laryngeal nerves to the glottis, external intercostals muscles, diaphragm and other inspiratory and expiratory muscles.
The mechanism of cough is as follows(12):
- first, it starts with a deep and rapid inspiratory effort;
- diaphragm (innervated by the phrenic nerve) and external intercostals muscles (innervated by segmental intercostals nerves) contract, creating a negative pressure around the lung;
- air rushes into the lungs in order to equalize the pressure;
- the glottis closes (muscles innervated by recurrent laryngeal nerve) and the vocal cords contract to shut the larynx;
- the abdominal muscles contract to accentuate the action of the relaxing diaphragm;
- this increases the pressure of air within the lungs;
- the vocal cords relax and the glottis opens, releasing air at over 100 mph;
- the bronchi and non-cartilaginous portions of the trachea collapse to form slits through which the air is forced;
- this clears out any irritants attached to the respiratory lining.
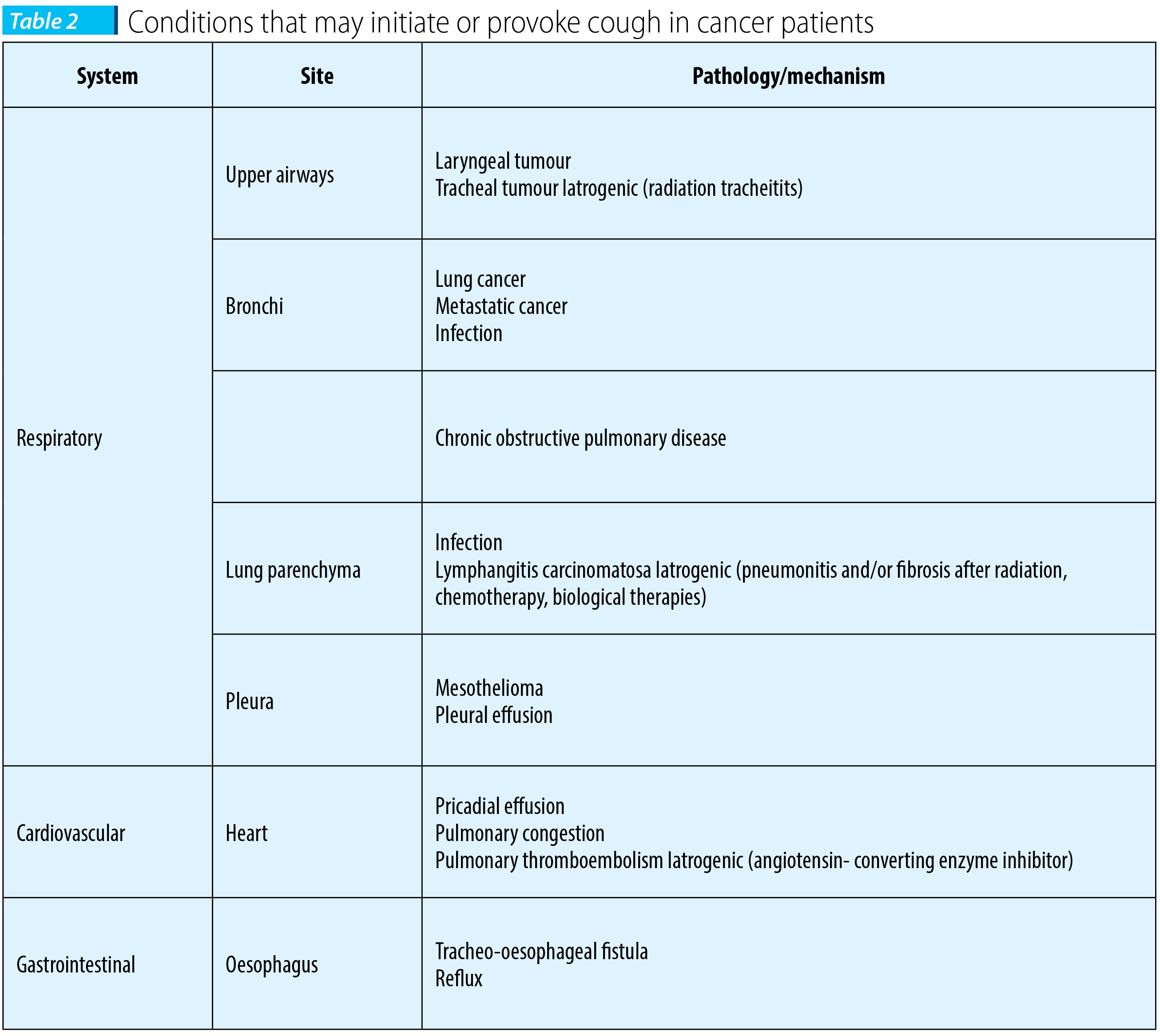
4. Causes of cough in cancer patients
Infections of the respiratory tract and chronic obstructive pulmonary disease at a smoker patient with lung cancer are frequently encountered in clinical practice. Immunocompromised patients are likely to develop invasive pulmonary aspergilosis. Symptomes included cough (54%), fever (54%), hemoptysis (30%) and shortness of breath (8%). Cough associated with upper respiratory tract infection might be elicited by a voluntary (cortical) pathway with the sensation of airway irritation acting as a trigger(7).There are also several complications of lung cancer which give rise to increased coughing, like pleural or pericardial effusion, bronchopleural fistula, lymphangitis carcinomatosa, or superior vena cava obstruction.
The mechanism of dry non-productive cough in pleural effusion is not completely understood, but apparently the lung compression by the fluid may bring opposing bronchial walls into contact, stimulating cough reflex.
Cough is a side effect of ACE inhibitors that cause increased levels of bradykinin which may be the cause of hyper reactivity of the cough reflex.
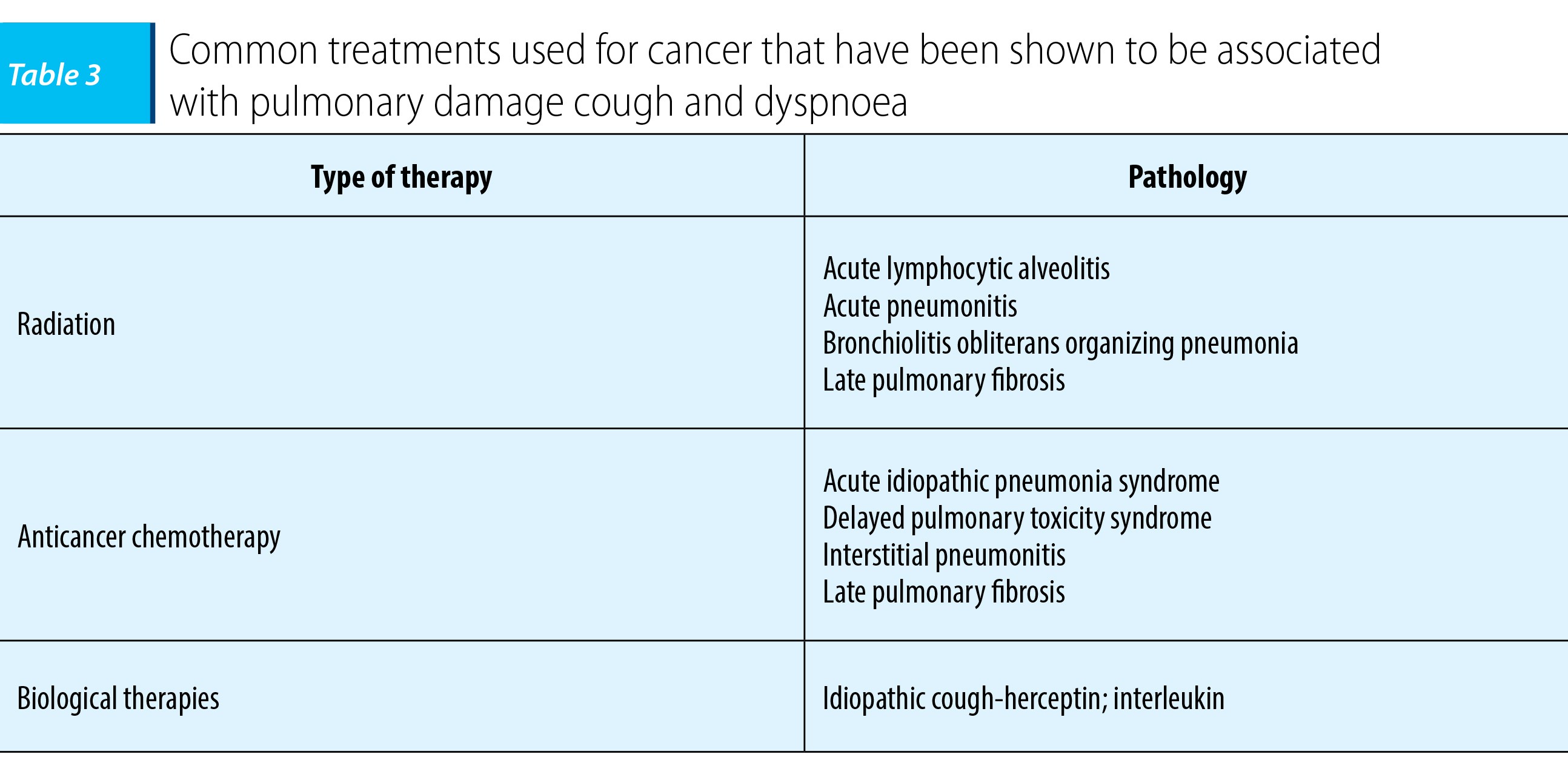
Busulfan-based chemotherapy used in autoloug peripheral blood stem cell transplantation causes acute or subacute idiopathic pneumonia syndrome, a condition characterized by cough and pulmonary infiltrates, and hypoxemia.
Anticancer drugs and radiotherapy are associated with pulmonary fibrosis manifested by persistent cough. Phase I study of paclitaxel as a radiation sensitizer in the treatment of mesothelioma and non-small cell lung cancer was initiated to determine the maximum tolerated dose and dose limiting toxicities of paclitaxel with concurrent thoracic irradiation. Six patients had grade 2 lung injury manifested by a persistent cough that required antitussives(8).
Irinotecan used in the management of colorectal cancer initiates interstitial pneumonitis that doesn’t respond to corticosteroid therapy. Data from a study - “Irinotecan-associated pulmonary toxicity” - suggest that cough and dyspnea were reported in approximately 20% of patients in USA(9).
Radiation therapy may lead to hypersensitivity pneumonitis and lymphocytic alveolitis, according to an article about lung toxicity following chest irradiation in patients with lung cancer. After clinical fractioned irradiation, acute radiation pneumonitis consisting in cough, and shortness of breath occurred in less than 10% of patients.
There are also iatrogenic causes of iatrogenic cough in cancer patients in palliative care. Twenty-nine patients with non-resectable stage IV head and neck cancer who participated in a Phase I study of radiation therapy with 70 Gy/7 weeks, concurrent with weekly gemcitabine, developed aspiration prior, soon after therapy and late post-therapy. After intensive chemo-radiotherapy, significant objective swallowing dysfunction in prevalent. It promotes aspiration which may lead to a cough reflex and may be associated with pneumonia(11).
The diminished cough reflex was the result of a disordered epiglottal and pharyngeal muscle coordination that delayed cough and was ineffective in expectorating the aspirated material.
Mediastinal encroachment of a bronchial cancer or simply during thoracic surgery for lung cancer, or unilateral vocal cord paralysis can lead to reduced cough effectiveness.
5. Assesment of cough in cancer patients
There are a series of tools in order to measure specific symptoms for cancer patients that helps the physician to evaluate the impact of cough on the quality of life: the Lung Cancer Symptom Scale; the Functional Assessment of Cancer Treatment (FACT); the EORTC LC-13.Imaging can be also useful to identify the cause of cough: X-ray, CT scan or ultrasound in case of suspected pleural or pericardial effusion.
According to latest studies, bronchoscopy may be indicated to complete the assessment of cough in non-smokers with normal chest radiograph to diagnose bacterial suppurative disease and other non-malignant airway disease. However, a patient who smokes cigarettes, who has a new cough, or a changing character of the cough that persists for months should have a bronchoscopic examination even when the chest radiograph findings are negative(17).
Dyspnea accompanies cough: if it is an intraluminal airway tumour, it will stimulate cough receptors and obstruct airflow to produce dyspnea; if it is an extraluminal tumour compression of a large airway, it may not associate cough, however the obstruction of the airway may lead to post-obstructive pneumonia that accentuates cough.
6. Management of cough in cancer patients
6.1. Radiation therapyOne of the primary purposes of the radiotherapy is palliation of symptoms. One of the studies on this subject had the objective to investigate the changes in respiratory symptoms and quality of life in patients with locally advanced and metastatic non-small cell lung cancer receiving radiotherapy. Assessments were performed before radiotherapy and two weeks, six weeks and three months after radiotherapy. The quality of life response rates were good for cough in 49% of patients(13).
In the last few years, there has been a tendency to use a continuous hyperfractionated radiotherapy and focused on the outcome on long term treatment. The randomized multicentre trial of continuous hyperfractionated accelerated radiotherapy versus conventional radiotherapy in patients with head and neck cancer on a total of 615 patients showed that there were significantly worse symptoms of cough and hoarseness at six weeks in those treated conventionally(14).
After examining ten published randomized trials of palliative lung cancer from Cochrane databased, it was concluded that there was no regime that gave better symptom resolution and the patients should be treated with the minimum dose in one or two fractions (hypofractination). A total of 47 patients with advanced non-small cell lung cancer were treated with four weekly fraction of 5 Gy to a total dose of 20 Gy - cough was relieved in 68% of patients(15).
When lung cancer recurs after a course of radiotherapy, it is possible to offer a second course of radiotherapy. The conclusion of a study with forty-eight lung cancer patients who were reirradiated was that 60% of patients achieved improvement in cough, and 73% in dyspnoea(16).
6.2. Chemotherapy
Gemcitabine- and cisplatin-based combinations chemotherapy has concentrated on specific symptoms including cough.
Gemcitabine used as a single agent treatment for inoperable non-small cell lung cancer has given relief of cough in 44% of patients, and of dyspnoea in 26% of patients(18).
A study in poor prognosis (performance status 2) of non-small cell lung cancer patients comparing combination chemotherapy (carboplatin and paclitaxel) versus single agent therapy (gemcitabine or vinorelbine) showed that a good palliation of symptoms was achieved (median time to progression was 4.6 months in the combination arm and 3.5 months in the single agent arm)(19).
6.3. Pharmacologic treatment of cough
Cough may persist in the setting of lung cancer despite all other treatments directed at cancer and the associated symptom of cough. There are two classes of antitussive drugs used: with central activity (opioids and nonopioids) and with peripheral activity.
The drugs that have been studied in the setting of cancer and improvement in cough related to cancer are hydrocone, dihydrocodeine, levodropropizine, sodium cromoclycate and benzonatate.
Opioids like dyhidrocodeine and hydrocodone are the best cough suppressants in patients with lung cancer. In a phase II study of hydrocodone for cough in advanced cancer, twenty-five patients with cough from irreversible causes and no previous use of this drug were given 5 mg of hydrocodone twice daily and then titrated daily maximum 60 mg/day. Cough severity frequency associated symptoms and complications and activities of daily living improved significantly with mild side effects. The best median response was 70% in cough frequency which was achieved with a dose of 10 mg/day(21).
Further research in this topic led to a study on the efficacy and tolerability of levodropropizine drops (75 mg) and dihydrocodeine (10 mg) on non-productive cough in primary and metastatic lung cancer. Subjective cough severity was reduced during treatment with either of the drugs, the antitussive effect and time profile being similar for both drugs. The percentage of patients experiencing somnolence in the group receiving levodropropizine (8%) was lower as compared with that of dihydrocodeine group (22%)(22).
Disodium cromoglycate produces antitussive effects via an inhibitory activity on sensory nerves and to suppress sensory C fiber activation by capsaicin. It induces a long lasting chloride dependent nerve depolarization and reduces the firing of action potentials following desensitization of the nerve(23). The study regarding the treatment of cough in advanced lung cancer with inhaled sodium cromoglycate stressed the fact that it can reduce cough in non-small cell lung cancer patients and appears to be cost-effective and safe(24).
Benzonatate is a peripheral antitussive that decreases the sensitivity of the mechanical pressure or distortion receptors in the lower airway and lung. In a case series, benzonatate controlled cough in 80% of 21 patients with malignant pulmonary involvement(25).
An important issue arises when a cancer patient is already receiving opioid treatment for pain and then complains of cough. In this case, it would be appropriate to use another class of drug or another approach like external beam radiation.
Some centers of palliative care in United States use nebulized lidocaine or bupivacaine for intractable unproductive cough. Lidocaine given systemically is very effective in inhibiting cough, but only at high plasma concentrations. Lidocaine penetrates rapidly through the blood brain barrier and inhibits the neural activity of the central nervous system, contributing to the antitussive effect.
The mechanism of action is anaesthesizing sensory nerve endings in the hypopharynx, larynx and upper airways but it also has a short duration of action.
6.4. Endobronchial treatment to relieve cough
The endobronchial therapies are given during bronchoscopy. These methods are used in order to remove or shrink the obstructive tumour. The bronchial debridement, stent placement, laser surgery, electrocoagulation, as well as photodynamic therapy, brachytherapy and cryosurgery are some of the techniques of endobronchial treatment.
All endobronchial techniques have the potential to provide relief of cough, but because neither of the endobronchial treatments methods eradicate the tumour, it is troublesome to manage cough.
Brachytherapy is proved to be effective and a safe palliative treatment for endobronchial malignancies, but further investigations are necessary to determine the optimal dose scheme and its efficiency in bronchogenic carcinoma and combined with external beam radiation therapy or surgery or other endobronchial procedures such as laser or cryotherapy(26).
American guidelines recommend that patients with dyspnea or hemoptysis due to endobronchial tumours cough may also be present. Endobronchial methods should be considered for the palliation of these symptoms, but cough alone is seldom a reason to offer such a treatment.
Bibliografie
2. Portenoy RK, Thaler HT, Kornblith AB et al., Symptom prevalence, characteristics and distress in cancer population. Qual Life Res, 1994; 3: 183-9.
3. Wang XS, Shi Q, Lu C, Basch EM, Johnson VE, Mendoza TR, Mobley GM, Cleeland CS, Prognostic value of symptom burden for ovarall survival in patients receiving chemotherapy for advanced nonsmall lung cancer, Cancer 2010 January 1 ; 116 (1); 137-45.
4. Catane R., Cherny N. I, Kloke M, Tanneberger S, Schrijvers D, European Society for Medical Oncology Handbook of Advance Cancer Care, Taylor & Francis Group 2006.
5. Irwin RS et al., Managing Cough as a Defense Mechanism and as a Symptom, Chest Vol 114 No 2, August 1998, supplement p133S-181S.
6. Kubik A, Zatloukal P, Boyle P, Robertson C, Gandini S, Tomasek L, Nigel G, Havel L, Lung Cancer, March 2001 volume 41, issues 2-3, 111-122.
7. Pidhorecky I, Urshel J, Anderson T, Annals of Surgical Oncology Resection of Invasive Pulmonary Aspergilosis in Immunocompromised Patients; 2000 May; 7 (4): 312-7.
8. Herscher L, Hahn SM, Kroog G, et al. Phase I study of paclitaxel as a radiation sezitizer in the treatment of mesothelioma and non-small cell lung cancer, Journal of Clinical Oncology 1988; 16:635-41.
9. Madarnas Y, Webster P, Shorter AM et al. Irinotecan-associated pulmonary pulmonary toxicity. Anticancer Drugs 2000; 11: 709-13.
10. Abratt RP, Morgan GW Lung toxicity following chest irradiation in patients with lung cancer. Lung cancer 2002; 35:103-9.
11. Eisbruch A, Lyden T, Bradford CR et al. Objective assesment of swalowing dysfunction and aspiration after radiation concurrent with chemotherapy for head and neck cancer, Int J Radiat Oncol Biol Phys 2002 May 1; 53 (1); 23-8.
12. Harsolya M.S, Patel V.M, Pathan J.KK, Singh S., Rahman A. A Review - Mechanism of Cough, International Journal of Pharmaceutical &Biological Archives 2011; 2(3): 840-846.
13. Laengendijk J.A, Velde G.P.M et al. Quality of life after palliative radiotherapy in non-small cell lung cancer-a prospective study, International Journal of Radiation Oncology Biology Physics, Volume 47, 1 April 2000, pages 149-155.
14. Griffiths GO, Parmar MK, Bailey AJ. Physical and psychological symptoms of quality of life in the CHART randomized trial in head and neck cancer: short term and long term patient reported symptoms. CHART Steering Committe. Continuous Hyperfractionated accelerated radiotherapy, Br J Cancer 1999, Dec; 81 (7): 1196-205.
15. Bhatt ML, Mohani BK, Kumar L, Chawla S, Sharma DN, Rath GK. Palliative treatment of advanced non-small cell lung cancer with weekly fraction radiotherapy, Indian J Cancer 2000 Dec; 37 (4): 148-52.
16. Kruser T J, Bradley P McCabe et al. Reirradiation for locoregionally recurrent lunc cancer outcomes in small cell and non small cell lung cancer Am J Clin Oncol 2014 Feb; 37 (1): 70-76.
17. Paul A, Kyale MD, FCCP Chronic Cough Due to Lung tumours: ACCP Evidence Based Clinic Practice Guidelines, Chest 2006: 129 (1 suppl); 147S-153S.
18. Hoskin P, Ahmedzai SH, Assessment and management of respiratory symptoms of malignant disease. In Ahmedzai SH Muers M Supportive Care of Respiratory Disease Patient, Oxford University Press 2003.
19. Lilenbaum R, Villaflor VM, Langer C et al. Single agent versus combination chemotherapy in patients with advanced non-small cell lung cancer and a performance status of 2: prognostic factors and treatment selection based on two large randomized clinical trials, J Thorac Oncol 2009 Jul; 4(7): 869-74.
20. Twycross R, Wilcock A, Respiratory symptoms In Twycross R, Wilcock A, Symptom Management in Advanced Cancer, 2nd edition, Oxford Radcliffe Press, 1997: 141-79.
21. Homsi J, Walsh D, Nelson KA, Sarhill N et al. A phase II study of hydrocone for cough in advanced cancer, Am J Hosp Palliat Care 2002 Jan-Feb; 19(1): 49-56.
22. Luporini G, Barni S, Marchi E, Daffonchio L, Efficacy and safety of levodropropizine and dihydrocodeine on nonproductive cough in primary and metastatic lung cancer, Eur Respir J, 1988 Jul, 12 (1): 97-101.
23. Jackson DM Pollard CE, Roberts SM, The effect of nedocromil sodium on the isolated rabbit vagus nerve, Eur J Pharmacol 1992; 221: 175-7.
24 Moroni M et al., Inhaled sodiul cromoglycate to treat cough in advanced lung cancer patients, Br J Cancer 1996 Jul; 74 (2) :309-11.
25. Doona M, Walsh D, Benzonatate for opioid resistant cough in advanced cancer, Palliat Med 1998 Jan; 12 (1): 55-8.
26. Sheski FD, Mathur PN, Cryotherapy, electrocautery and brachytherapy, Clin Chest Med 1999 Mar; 20 (1): 123-38.
Articole din ediţiile anterioare
Iron, ferroptosis and association with tumoral evolution and potential therapeutic impact
Articolul îşi propune să arate tendinţele moderne de redefinire a rolului fierului în procesele metabolice normale şi patologice, reamintind ...
Cancerul, o problemă nerezolvată
Pornind de la ideea că eşecul nostru de a vindeca cancerul vine din lipsa noastră de a înţelege complexitatea sa, ştiinţa contemporană priveşte tre...
Carcinom renal cu celule clare - evoluţia bolii metastatice şi supravieţuirea după patru linii de terapie ţintită. Prezentare de caz
În prezentarea de față vă aducem în atenție cazul unui pacient cu carcinom renal cu celule clare și boală extinsă prin metastaze multiple pulmonare...
Reiradierea cancerelor de cap şi gât în era imunoterapiei
Cu toate că în ultimii ani s-au înregistrat progrese semnificative în ceea ce priveşte terapia modernă multidisciplinară pentru cancerele de cap ş...