The correct and complete excision of lower eyelid carcinomas, with adequate histopathological control, leads to complex and unpredictable post-excisional defects regarding shape and size. Under these circumstances, the reconstruction decision can be difficult, considering that the treated areas must be both functional and respect the aesthetical principles, along with satisfying symmetry and proportions.
Reconstrucţia defectelor post-excizionale de pleoapă inferioară toată grosimea după chirurgia oncologică a carcinoamelor de piele
Reconstruction of post-excisional full thickness defect of the lower eyelid after oncological surgery for skin carcinomas
First published: 23 mai 2018
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Orl.39.2.2018.1728
Abstract
Rezumat
Excizia corectă şi completă a carcinoamelor de pleoapă inferioară, cu controlul histopatologic al marginilor, duce la defecte complexe şi imprevizibile în ceea ce priveşte forma şi dimensiunea. În aceste condiţii, decizia de reconstrucţie poate fi dificilă, întrucât aria interesată trebuie să îşi păstreze funcţionalitatea şi, în plan secund, să respecte principiile estetice, simetria şi proporţiile corecte.
Introduction
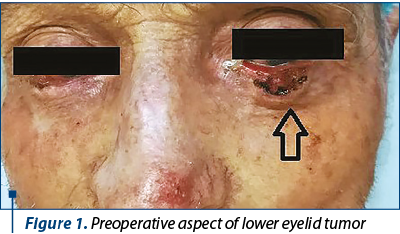
A 73-year-old male presented to our clinic, in the Plastic and Reconstructive Surgery Department, for bilateral lower eyelid masses. The first assessment of the patient identified ulcerated lesions, occupying approximately 80% of the left lower eyelid and approximately 60% of the right one (Figure 1), unpainful, with progressive evolution for three years, with irregular margins, described classically as an initially small lesion that did not heal, and kept on growing. The patient’s medical history describes several basal cell carcinomas either cauterized or surgically removed in the last 10 years; he declines smoking and alcohol abuse, but admits sun exposure for over 15 years. The patient was currently under treatment for hypertension.
We decided to surgically treat the left lower eyelid, considering the size and evolution in comparison with the right eyelid, under general anesthesia. The tumor was excised with 3 mm safety lateral limits, in full thickness of the lower eyelid (Figure 2). The post-excisional defect included both anterior (cutaneous) and posterior (tarsus) lamella in approximately 90% of the lower lid. Therefore, we considered the options which would replace tissue from the external lateral two thirds of the lower eyelid resulting from the tumor excision, involving both lamellae.

Discussion
Full thickness lower eyelid reconstruction is challenging, mostly because of the need to replace both the anterior and the posterior lamellae.
Considering the extent of the anatomical defect, the options for reconstructing the posterior lamella (tarsus), which is the only structure holding the eyelid in place, included:
-
Hard palate chondro-mucosal graft, which is now considered the gold standard for tarsal reconstruction.
-
Hughes tarsoconjuctival flap(1).
-
Contralateral eyelid tarsus graft.
-
Autologous concha cartilage graft.
-
Nasal septum cartilage graft.
Hard palate chondro-mucosal graft is – as we mentioned – the gold standard for tarsus reconstruction, due to the similar consistency to the actual tarsus, ease to harvest and low morbidity at the donor site.
Hughes flap should be avoided in cases where MOHS excision is not available due to the potential for relapses in both lower and upper lid of the operated eye.
Harvesting tarsus from the contralateral eyelid was not possible due to the presence of the mass in the right lower lid.
Autologous concha cartilage is easy to harvest, but do not match the consistency of the tarsus.
Nasal septum graft is technically difficult to harvest, and patients often complain of postoperative discomfort at the donor site.
For the reconstruction of the anterior lamella in cases where the posterior lamella reconstruction requires grafting, it is mandatory to use flaps in order to provide vascular support for the graft.
We considered:
-
Periorbital cutaneous flaps, including Fricke flap and Tenzel flap(2,3).
-
Modified Fricke flap.
-
Modified Mustarde flap(4).
-
Cheek V-Y Advancement Skin Flap to the Lower Eyelid(5).
-
Nasolabial flaps(6).
Periorbital and nasolabial flaps would not cover the defect entirely, due to anatomic particularities of the patient’s face subunits.
Mustarde flap requires extensive dissection and laborious inset to prevent postoperative ectropion.
“V-Y” advancement flap for full thickness lower eyelid defect was not precisely suitable for our patient, since the lateral extent of the “Y” must be sutured to both canthal ligaments and the weight of the flap can be a trigger for postoperative ectropion.
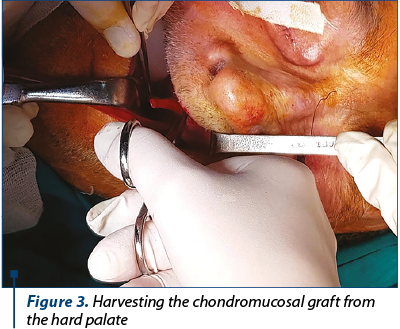
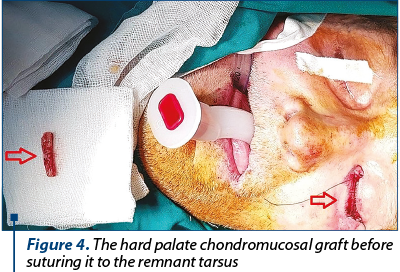
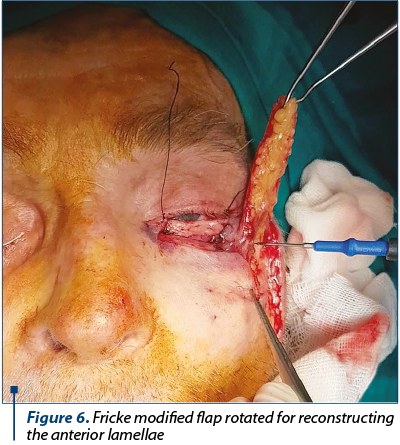
For our patient, we decided to harvest chondro-mucosal graft (Figure 3) from the hard palate for reconstructing the posterior lamella (Figure 4 and Figure 5) and to use a modified Fricke flap (cutaneous flap tailored for the defect harvested from the cheek based at the lateral portion of the orbicularis muscle) for the anterior lamellae.

Conclusions
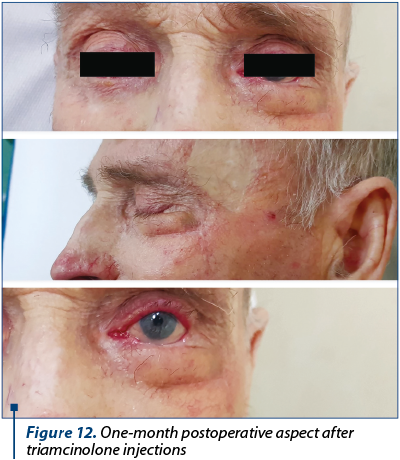
Due to the short operative time (very important, considering the patient’s age) and to our choice for simple reconstruction, the patient recovered fast and there were no intra- or postoperative complications (Figure 8). The eye’s functionality was properly restored and cosmesis was satisfying for the patient (Figure 9, Figure 10). The harvesting zone recovered well after per secundam healing in approximately 10 days after surgery (Figure 11). Three weeks postoperatively we observed “pin-cushioning” of the flap and decided to inject triamcinolone every four to six weeks. The results were favourable (Figure 12). The patient is scheduled to undergo surgery for the contralateral lower eyelid carcinoma.





Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Hughes WL. Reconstructive surgery of the eyelids, 2nd Ed. St. Louis: Mosby. 1954; 135.
- Hagerty RF, Smoak RD. Reconstruction of the lower eyelid. Plast Reconstr Surg. 1966; 38:52.
- McGregor IA. Eyelid reconstruction following subtotal resection on upper or lower lid. Br J Plast Surg. 1973; 26:346.
- Macomber WB, Wang MK. Total reconstruction of upper and lower eyelids in the treatment of cancer. Clin Plast Surg. 1978; 5:501.
- Gillies H. Plastic surgery of the face. London: Frowdes, Hodder & Stoughton. 1920; 20.
- Paletta FX. Lower eyelid reconstruction. Plast Reconstr Surg. 1973; 51:653.