The orbital tumour pathology is very complex. The most encountered types of malignancies of the region are squamous and basal-cell carcinoma and lymphoma. The surgical methods involved in the curative treatment are tumour resection, exenteration and advanced exenteration. The defects after tumour resection must be reconstructed using flaps that will allow a fast and proper healing, with a good quality of life for patients. The use of local flaps will ensure a good outcome.
Tratamentul tumorilor maligne orbitare
Treatment of orbital malignant tumours
First published: 23 mai 2018
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Orl.39.2.2018.1727
Abstract
Rezumat
Patologia tumorală din sfera orbitară este extrem de variată. Printre cele mai întâlnite tipuri de tumori maligne se numără carcinomul bazocelular, spinocelular şi limfomul. Procedeele de ablaţie chirurgicală cele mai folosite sunt rezecţia simplă, exenteraţia şi exenteraţia extinsă. Reconstrucţia defectelor trebuie să asigure o vindecare rapidă şi stabilă, dar şi o calitate crescută a vieţii, atât din punct de vedere funcţional, cât şi estetic. Lambourile locale de vecinătate asigură o mare parte a acestor deziderate, mai ales o reintegrare rapidă socială a pacienţilor.
Introduction
The orbit is a complex anatomic region containing the eye, muscles, fat, neuro-vascular bundles, glandular tissue and conjunctiva.
The most encountered primary orbital tumours are the lymphomas(1). Among these, the malignant lymphomas are dominant (over 60%). The malignant lymphoma can be solitary tumours or an expression of a systemic disease. Most of the patients diagnosed with solitary masses will develop a systemic condition in the future. Regarding the lymphoma subtype, the non-Hodgkin MALT is one of the most diagnosed.
The adenoid cystic carcinoma is the most important tumour entity diagnosed at the lacrimal gland(2). As with other glands, it has a tendency towards perineural invasion. The prognosis is unfavourable, due to local spreading.
The squamous and basal cell carcinoma are the main malignant processes encountered at the level of the eye lids(3). The squamous carcinoma usually appears on a precedent epithelial lesion, such as actinic keratosis, keratoacantoma or radiation dermatitis. It usually involves the lymph nodes and sends distant metastases.
The primary orbital melanoma is a very rare tumour. It usually appears in older patients with white skin and light coloured iris(4). It probably has its origins in the neural crest. There is no correlation proven regarding onset and UV exposure.
Up to 10% of all orbital tumours are comprised by distant metastasis. Frequently, the main tumour is located in the breasts(5), prostate or in the lungs. They are usually found in the anterior orbit rather than the posterior.
When it comes to imaging these entities, the most inexpensive method is the ultrasound, which can generate details regarding the consistency of the masses either solid or cystic. The computer tomography is an excellent method, allowing a definitive diagnosis and being easily tolerated by the patient. The malignant tumours in the orbit can appear as irregular processes with undifferentiated margins. On a CT scan, we can see the amount of bone infiltration and the extension in to the sinuses.
Although MRI imaging is harder to process, it is an important tool that allows to accurately determine a final diagnosis and also for viewing intracranial extension of the tumours. It is very helpful for tumours that have an important vascular component. The tumour extension can be accurately determined, as most of the orbital masses present with a hyper signal in MRI scanning.
In the vast majority of the cases, the treatment of choice is surgical(6), excepting for the systemic lymphoma. The goal of surgical treatment is mainly a disease-free management of the masses, but also a cosmetic and social pleasing outcome.
Case series
Case I
A 43-year-old female patient presented at examination with a tumour mass that affected the lower eye lid and the medial cant. The CT scan showed that the tumour had not reached the eye or the bony walls of the orbit. The tumour was surgically excised and the defect was covered with a rotated frontal flap. The histological exam was definitive for squamous cell carcinoma, with no extension into the muscles and periorbital fat. The follow-up was positive.

Case II
The second case is of a 66-year-old female which presented with a right eye tumour process. The MRI showed a large invasion in the periorbital tissues. An orbital exenteration was performed and the defect was covered with a frontal flap. The follow-up was positive.

Case III
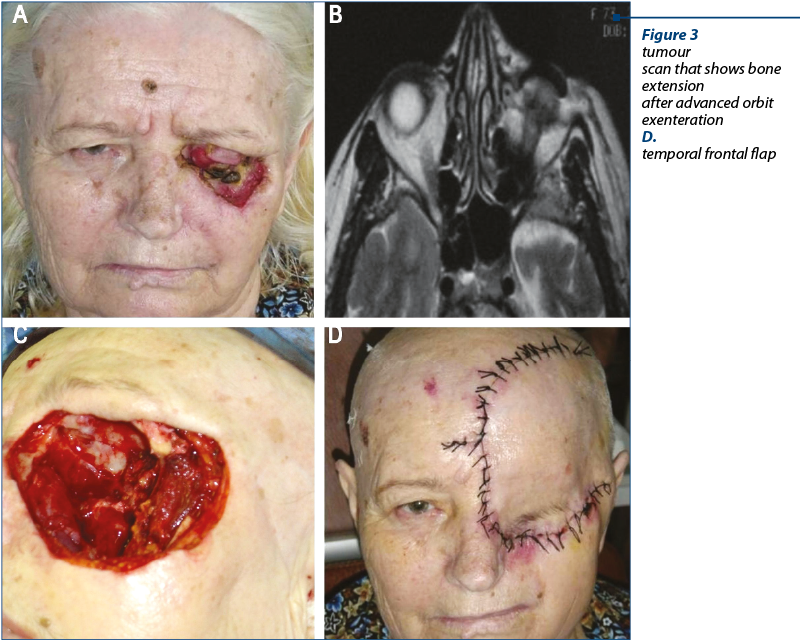
The third case is of a 68-year-old female patient who presented with a local recurrence after the excision of a lower eyelid tumour (squamous cell carcinoma). A large tumour mass was noted that affected the orbit, the lower eye lied and the infraorbital region. There was no lymph nodes invasion. The MRI examination showed extension in the nasal cavity, floor of the orbit and the lateral orbital wall. An advanced exenteration was conducted. The large defected was reconstructed with a Ti mesh, temporal muscle and a temporal and frontal flap. The final histological exam was squamous cell carcinoma. The patient underwent radiotherapy. The follow-up was positive.
Discussion
The malignant orbital tumours can be primary or tumour masses that extend into the orbit from:
-
maxillary sinuses
-
ethmoid sinuses
-
frontal sinus
-
the skin.
The lymphoma is one the most encountered malignant masses in the orbit, usually involving the lachrymal gland, but also can be found everywhere else into the orbit. There are many epithelial origin tumours derived from the lacrimal gland.
The sarcomas are often seen in very different types (angio-, fibro- or chondrosarcoma). In children, the most important tumour is rhabdomiosarcoma(7).
The epitheliomas in the orbit usually are found in white skin patients with long sun exposure and with different skin degenerative processes. The squamous cell carcinoma, although more aggressive, is much rarer.
Depending on tumour size and position, there are many surgical approaches that can be employed(8):
-
Lateral orbitotomy.
-
Transconjunctival approach for small tumours.
-
Supraorbitary approach.
-
For malignant processes of the orbit, the conservative treatment is enucleation: the eye is removed, with the preservation of the muscles, the fat and the conjunctiva.
-
The main surgical method is the orbital exenteration, which represents the complete removal of the eye with the extrinsic muscles, the lachrymal gland, the periorbital fat, and the neuro-vascular bundles. When the tumour is very aggressive and has reached the bony walls or when dealing with recurrence, an advanced exenteration is performed, that includes the paranasal sinuses, the maxilla or the base of the skull up to the anterior cranial fossa.
-
Depending on tumour type and position, the exenteration can be classified as: total, subtotal and advanced. During a total exenteration the incision is carried down to bone, the subtotal preserves the eyelids and the advanced exenteration can include a frontal temporal and sphenoid craniotomy and en bloc excision of the orbit with bony walls(9). For reconstructing these large defects, local flaps can be used, such as temporal muscle flap or pericranium, temporal frontal flap, but also distant free vascularised flaps.
The temporal muscles is one of the most efficient methods for reconstructing the orbit especially when an advanced exenteration is to be performed that will include the superior part of the maxilla, and it also represents a strong base for the frontal median rotated flap(10). It allows for large defects in the middle level of the face to be accurately reconstructed.
Conclusion
The management of the orbit malignant masses is influenced by tumour type and position. The surgical treatment is still the best option for the vast majority of cases. Although the orbit exenteration is a very aggressive method of treatment, with the use of local flaps, the defects can be reconstructed in a manner that will allow a fast social rehabilitation for the patients.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Koopman JH, van der Heiden-van der Loo M, van Dijk MR, Bijlsma WR. Incidence of primary malignant orbital tumours in the Netherlands. Eye. 2011; 25(4):461-465. doi:10.1038/eye.2011.9.
- Bernardini FP, Devoto MH, Croxatto JO. Epithelial tumours of the lacrimal gland: an update. Curr Opin Ophthalmol. 2008; 19(5):409–413.
- Font RL. Eyelids and lacrimal drainage system. In: Ophthalmic Pathology. An Atlas and Textbook. 3rd ed. Philadelphia: WB Saunders. 1996; pp. 2229–32.
- Shields JA, Shields CL, Brotman HK, Carvalho C, Perez N, Eagle RC. Cancer metastatic to the orbit: the 2000 Robert M. Curts Lecture. Ophthal Plast Reconstr Surg. 2001; 17(5):346–354.
- Shields JA, Bakewell B, Augsburger JJ, Flanagan JC. Classification and incidence of space occupying lesions of the orbit. A survey of 645 biopsies. Arch Ophthalmol. 1984; 102: 1606–1611.
- Hassler W, Unsold R, Schick U. Orbital tumours: diagnosis and surgical treatment. Dtsch Arztebl. 2007; 104:A496-A501.
- Darsaut TE, Lanzino G, Lopes MB, Newman S. An introductory overview of orbital tumours. Neurosurg Focus. 2001; 15:E1.
- Park HJ, Yang S-H, Kim IS, Sung JH, Son BC, Lee SW. Surgical Treatment of Orbital Tumours at a Single Institution. Journal of Korean Neurosurgical Society. 2008; 44(3):146-150. doi:10.3340/jkns.2008.44.3.146.
- Ben Simon GJ, Schwarcz RM, Douglas R, Fiaschetti D, McCann JD, Goldberg RA. Orbital exenteraţion: one size does not fit all. Am J Ophthalmol. 2005; 139:11-7.
- Menderes A, Yilmaz M, Vayvada H, Demirdover C, Barutcu A. Reverse temporalis muscle flap for the reconstruction of orbital exenteration defects. Ann Plast Surg. 2002; 48:521-7.
Articole din ediţiile anterioare
Variaţiile morfologice şi morfometrice ale fisurii orbitare inferioare
Importanţa cunoaşterii detaliate a morfologiei şi morfometriei fisurii orbitare inferioare şi a variaţiilor sale anatomice este indispensabilă pe...
Abordul endoscopic transnazal al unui condrosarcom septal extins la rostrumul sfenoidal
O pacientă, în vârstă de 31 de ani, s-a internat în vederea ablaţiei unei formaţiuni tumorale situate la nivelul părţii posterioare a septului naza...
Carcinom orbitar extirpat endoscopic pe cale combinată, transetmoidală şi transcutanată. Prezentare de caz
Tumorile orbitare maligne reprezintă un spectru larg de tumori care includ tumori primare, tumori secundare (extensie de la structurile adiacente) ...
Adenocarcinom nazosinuzal – tratament chirurgical endoscopic
Tumorile maligne nazosinuzale reprezintă un capitol de patologie redutabil pentru practica medicală otorinolaringologică, care continuă să...