Factori de risc materni ce pot determina predictibilitatea rezultatelor fetale în cazurile de ruptură prematură de membrane
Maternal risk factors that could determine the predictability of fetal outcome in cases of premature rupture of membranes
Abstract
Objectives. The prevention of preterm birth is one of the highest priorities for international obstetric research. This study aimed to evaluate the maternal factors that may influence the pregnancy outcomes in order to assess the fetal outcomes. The main parameters analyzed were the variables newborn’s Apgar score at 1 minute and Apgar score at 5 minutes. Materials and method. This is designed to be a retrospective, observational and non-randomized study on a sample of 30 pregnant women with ruptured membranes, diagnosed and treated in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital, Romania, between May 2021 and October 2021. We used two simple and multiple univariate linear regressions to achieve the main objective. The dependent variable used the APGAR score at 1 minute and the APGAR score at 5 minutes. Results. We obtained significant results regarding the impact of CRP, leukocytes count at admission, mode of delivery, presence of chorioamnionitis, funisitis, and male sex of the newborn on neonatal outcome. Conclusions. These results support further research in developing feasible multivariable prediction models in women with preterm rupture of membranes below 34 weeks of gestation. These models can help clinicians manage low- or high-risk pregnant women efficiently.Keywords
preterm birthpremature rupture of membraneschorioamnionitisintraamniotic infectionintraamniotic inflammationRezumat
Obiective. Prevenţia naşterii premature este una dintre principalele priorităţi pentru cercetarea din domeniul obstetricii la nivel internaţional. Studiul are ca scop evaluarea factorilor materni care pot influenţa evoluţia sarcinii, în vederea stabilirii prognosticului fetal. Principalii parametri analizaţi au fost variabilele scorului APGAR la 1 minut al nou-născutului, respectiv la 5 minute. Materiale şi metodă. Studiul este retrospectiv, observaţional, nerandomizat, pe un eşantion de 30 de gravide cu membrane rupte, diagnosticate şi tratate în Clinica de obstetrică şi ginecologie din cadrul Spitalului Universitar de Urgenţă din Bucureşti, România, în perioada mai 2021 – octombrie 2021. Pentru realizarea obiectivului au fost folosite două regresii liniare univariate simple şi multiple, cu variabila dependentă scorul APGAR la 1 minut şi la 5 minute de la naştere. Rezultate. Rezultatele obţinute sunt semnificative în ceea ce priveşte impactul pe care îl au: CRP-ul, numărul leucocitelor la internare, modalitatea de naştere, prezenţa corioamniotitei, a funisitei şi sexul masculin al nou-născutului asupra evoluţiei neonatale. Concluzii. Aceste rezultate susţin cercetările ulterioare în dezvoltarea unor modele fezabile de predicţie multivariabile ce pot fi aplicate gravidelor cu membrane rupte prematur înainte de 34 de săptămâni. Aceste modele pot ajuta medicii obstetricieni să gestioneze într-un mod eficient gravidele cu risc scăzut sau ridicat.Cuvinte Cheie
naştere prematurăruptură prematură de membranecorioamniotităinfecţie intraamnioticăinflamaţie intraamnioticăIntroduction
Preterm birth is one of the leading causes of perinatal mortality and morbidity globally, therefore the prevention of preterm birth is one of the highest priorities for international obstetric research(1,2).
Preterm rupture of membranes (PROM) before 37 weeks of gestation is defined as the rupture of fetal membranes and leakage of amniotic fluid. PROM represents one of the most significant obstetrical conditions due to its large number of etiological agents and its essential impact on fetal involvement. PROM occurs in 3-4% of all deliveries and is responsible for 30% of all preterm deliveries(4,5).
Preterm birth is a multifactorial condition. Based on a solid evidence base, infection (mainly polymicrobial) is the etiological agent of preterm birth for the majority of cases(2-4). The most common isolated infectious agents are Ureaplasma spp. and Mycoplasma spp., from the lower genital tract. The most frequent invasion pathway is represented by the ascending path from the lower genital tract (vagina, cervix)(1,6).
The inflammatory changes produced by microorganisms that can cross fetal membranes (invade the amnios and chorion) cause the appearance of chorioamnionitis, funisitis, intraamniotic infection and fetal infection(1-3). Microbiological studies have shown that intraamniotic infection is liable for 25% to 40% of preterm births, although this percentage is underestimated in the conventional bacterial detection methods used. The studies revealed the association between the increased rate of neonatal complications with microbial invasion of the amniotic cavity(6,7).
The roles of differential virulence, polymicrobial interactions, host genetics and immune factors (the role of the maternal systemic immune response to the infection) are intensely debated topics in many recent studies regarding the obstetric and fetal outcome(13).
The study aimed to evaluate the maternal factors that may influence the outcome of pregnancy in order to be able to assess the impact on the fetal outcome. One of the main questions is finding predictor factors on the fetal outcome of pregnant women with PROM below 34 weeks of gestation. We need the predictor factors to develop and validate a multivariable prediction model to improve the clinical management.
Materials and method
1. Study design and sample collection
This is designed to be a retrospective, observational and non-randomized study on a sample of 30 pregnant women with ruptured membranes, diagnosed and treated in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital, Romania, between May 2021 and October 2021. The local ethics committee approved the study design and protocol. The informed consent was obtained from all participants. Eligible pregnant women who meet the following inclusion criteria were included in this study: age >18 years old, singleton pregnancy, PROM between gestational ages 24+0 and 33+6 weeks. The exclusion criteria were: pregestational or gestational diabetes mellitus, chronic hypertension, gestational hypertension, preeclampsia, the fetus signs of fetal growth restriction, congenital structural abnormality, chromosomal abnormality, and active vaginal bleeding. PROM was diagnosed by examination with a sterile speculum by verifying the pooling of amniotic fluid in the vagina. Gestational age was determined by first-trimester fetal biometry. The following laboratory analyses were ordered at admission and serially during the hospital stay in order to evaluate the presence of maternal systemic inflammation or infection: complete blood count, coagulation panel, C-reactive protein (CRP). We collected a cervical swab from all women in the study. All cervical samples were tested for the presence of M. hominis, M. genitalium, U. urealyticum and U. parvum using a multiplex-tandem polymerase chain reaction (MT-PCR) for the amplification of targeted DNA and RNA. The presence of inflammatory modifications in the choriodecidua, chronic plate, umbilical cord and/or amnion was taken into consideration to diagnose histologic chorioamnionitis. The diagnosis of funisitis was related to inflammatory changes in the umbilical cord. The neonatal morbidity was evaluated in this study as the need for intubation, persistent oxygen requirement for more than 6 hours, positive C-reactive protein (CRP), the need for antibiotics treatment, and sepsis was proven by solid clinical suspicion or bacterial culture.
The study aimed to evaluate the maternal factors that may influence the pregnancy outcomes in order to assess fetal outcomes. The main parameters analyzed were the variables APGAR score at 1 minute of the newborn and APGAR score at 5 minutes.
The study’s primary endpoints were: the ordinal variable APGAR score at 1 minute and the ordinal variable APGAR score at 5 minutes; we decided (for a more consistent analysis) that these variables can be considered continuous.
2. Statistical analysis
The R program, version 4.0.2 Copyright (C) 2020, The R Foundation for Statistical Computing, R Core Team (2020), was applied to conduct the statistical analysis. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria (https://www.R-project.org).
Two simple and multiple univariate linear regressions were used to achieve the main objective. The dependent variable used the APGAR score at 1 minute, and the APGAR score at 5 minutes. Simultaneously, the independent variables (predictors) were composed of a series of demographic-clinical parameters followed in the study. Since a premature newborn has lower APGAR scores than a full-term fetus, we did not consider the predictive role of gestational age at the time of pregnancy.
The approach to the descriptive statistical analysis was a usual one: for the categorical variables, there were calculated the absolute and relative frequencies, while for the continuous and ordinal variables, there were calculated the average, the standard deviation (SD), the median and the minimum and maximum distribution. The level of statistical significance a (the threshold for avoiding a type I error) for the study was 0.05, therefore p values lower than 0.05 were considered statistically significant.
3. Results
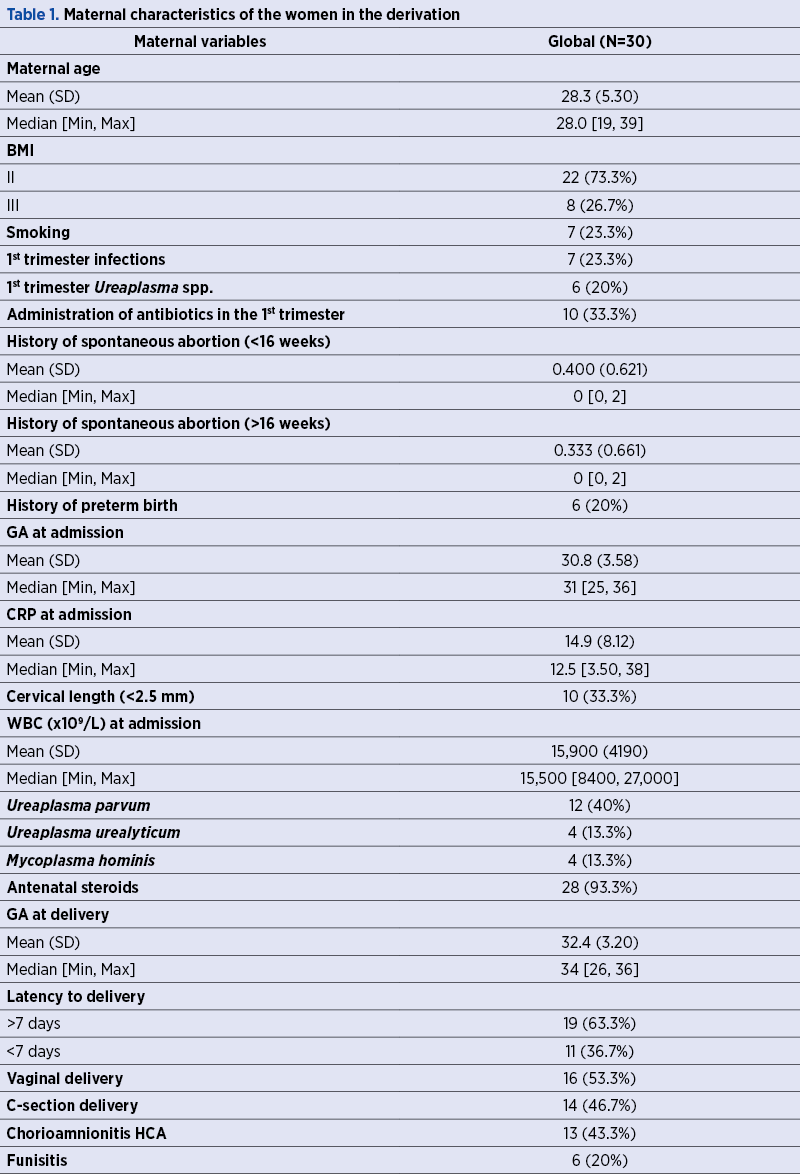
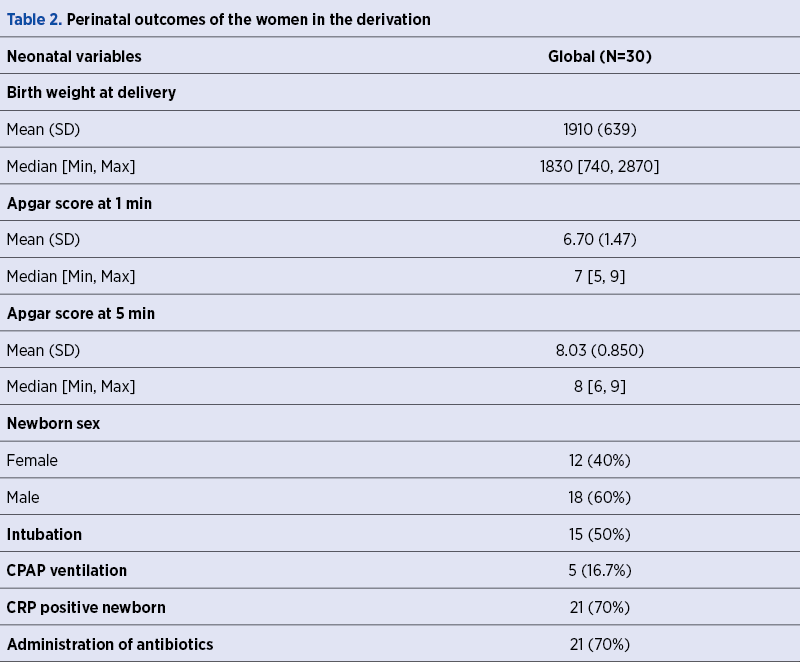
Tables 1 and 2 show the characteristics (demographical and clinical) of the 30 pregnant women included and the characteristics of their newborns. The mean age of women was 28 years old. The average gestational age at admission was 30 weeks. Ureaplasma spp. infection was found in 63.6% of cases (U. parvum 40%, U. urealyticum 13.3%, M. hominis 13.3%). The Gram stain revealed two cases of Escherichia and two cases of SGB. There were six cases of bacterial vaginosis. The mean gestational age of newborns was 32 weeks; 70% had positive C-reactive protein and required antibiotic treatment.
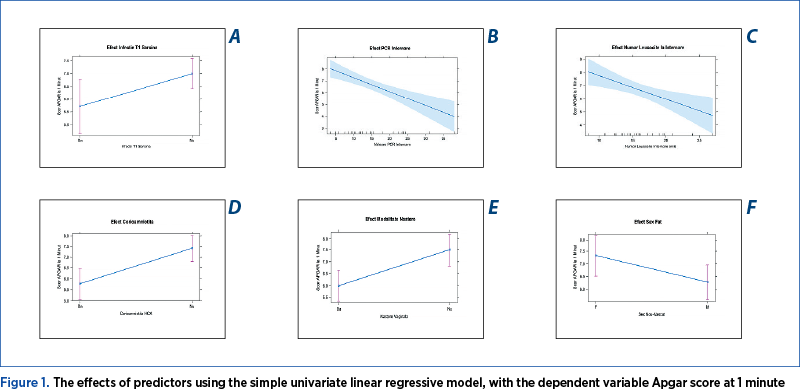
We obtained significant results using the simple univariate linear regressive model, with the dependent variable Apgar score at 1 minute. We observed that newborns of patients who did not have infections in the first trimester of pregnancy had, on average, 1.3 higher Apgar score at 1 minute. One possible explanation is that pregnant women diagnosed with infections in the first trimester of pregnancy tend to have a lower gestational age at birth. In our group, pregnant women with infections in the first trimester of pregnancy had an average gestational age of 30 weeks, while pregnant women without infections in the first trimester had a mean gestational age of 33 weeks, the effect being statistically significant (p<0.05) – Figure 1A.
Our study noticed that an increase of 1 unit of CRP at admission was associated with a decrease of the Apgar score to 1 minute by 0.12, and the effect had a statistical significance (p<0.01) – (Figure 1B). Also, an increase by 1000 leukocytes at admission was correlated with a decrease of 0.18 in the Apgar score at 1 minute. The effect had a statistical significance (p<0.01) – Figure 1C. These statistical associations support the impact of the infectious factor on the newborn outcome.
Among the effects of predictors, we noticed the influence of corticosteroid therapy. Patients who did not receive lung maturation treatment had an Apgar score at 1 minute lower by 1.8 points. However, there is not enough evidence to conclude, the p-value being marginally insignificant (p=0.09).
Pregnant women who gave birth by caesarean section had a 1-minute Apgar score with 1.5 points higher, a statistically significant effect (p<0.01) – Figure 1D.
The presence of chorioamnionitis was associated with an Apgar score at 1 minute of the newborn with 1.6 points higher, the effect being statistically significant (p<0.01) – Figure 1E.
Another aspect that can be considered is that newborns males had a 1-minute Apgar score with 1.1 points lower, the effect being statistically significant (p=0.05 and CI 95% does not contain 0) – Figure 1F.
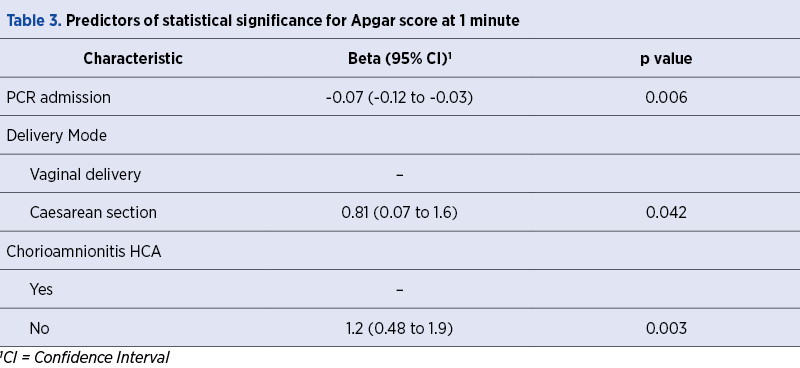
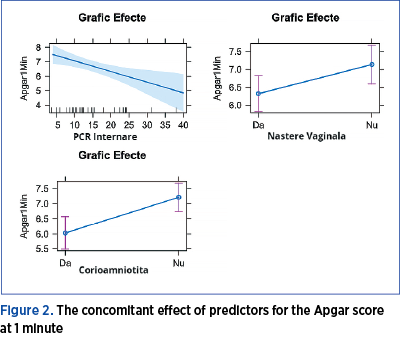
Simple univariate linear regression allows us to quantify the effect of each predictor without considering the effects of other predictive factors (Table 3). We used multiple univariate linear regression with a retrograde selection algorithm to assess the concomitant effect of predictors. The final model allows us to support the following conclusions: independent of the other predictors, an increase of 1 unit of C-reactive protein at admission is associated with a decrease of 0.07 in Apgar score at 1 minute; independent of other predictors, a fetus born by caesarean section has an Apgar score at 1 minute higher, on average, with 0.81; and, also, independent of other predictive parameters, the presence of chorioamnionitis is associated with an average decrease of 1.2 points of the Apgar score at 1 minute (all effects are statistically significant) – Figure 2.
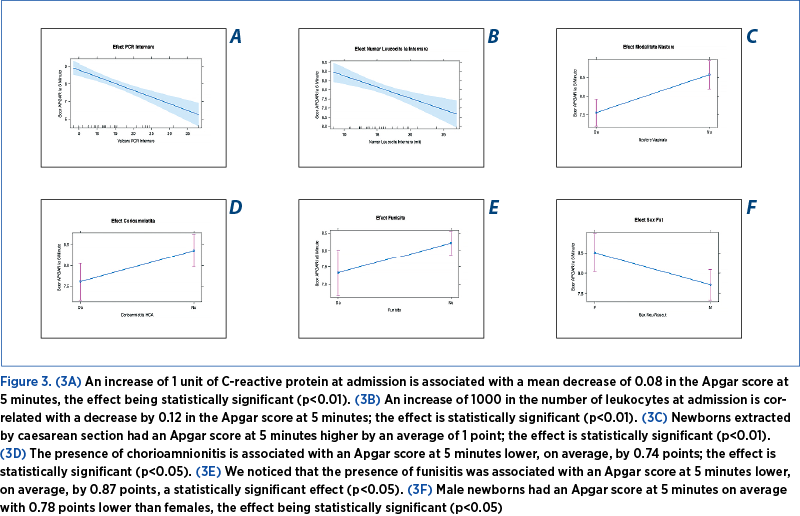
Using the same analysis as the previous one, but taking the Apgar score at 5 minutes as dependent variable, we obtained significant results in terms of the impact of CRP and lekocytes at admission, the delivery mode, funisitis, and male gender of a newborn over the neonatal outcome (Figure 3).
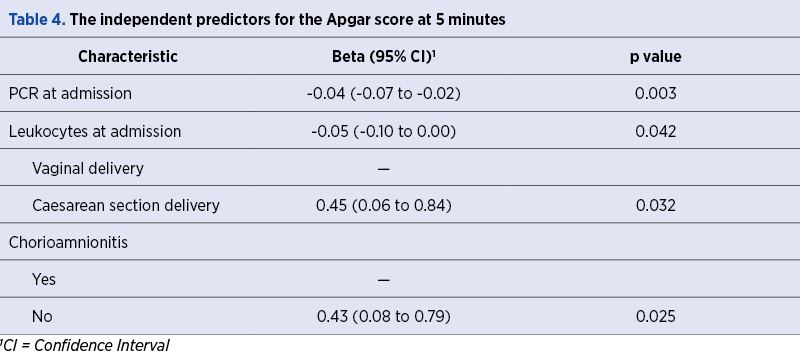
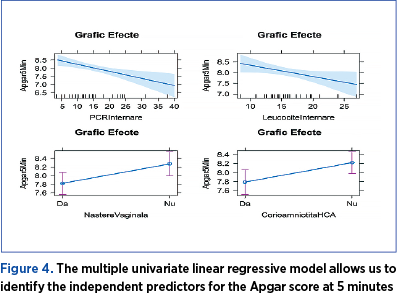
The multiple univariate linear regressive model allows us to identify the independent predictors for the Apgar score at 5 minutes (Table 4). We noticed that an increase of 1 unit of C-reactive protein at admission is associated with a decrease of 0.04 in Apgar score to 5 minutes. The increase of leukocytes by 1000 at admission is associated with a decrease of 0.05 in the Apgar score at 5 minutes. Caesarean section delivery was correlated with a 5-minute Apgar score 0.45 times higher than in case of vaginal delivery. Newborns of pregnant women with chorioamnionitis had a 5-minute Apgar score 0.43 times lower than those of pregnant women who do not have this pathology, all effects being statistically significant (Figure 4).
Discussion
Our research showed that the following factors had a significant impact in determining the neonatal outcome: gestational age at the time of infection, maternal inflammatory status at admission, corticosteroid administration, chorioamnionitis, funisitis and the delivery mode(8,10).
We noticed a significant association between maternal infection and neonatal outcomes regarding our results. Recent research shows that Ureaplasma spp. was among the most frequently detected from amniotic fluid and placenta in patients with PROM(6). Ureaplasma species were the prevalent microorganisms identified in our study in the first trimester of pregnancy and at admission. One of the most significant findings of this study was that infections in the first trimester of pregnancy affect the fetal outcomes. Infectious screening in the first trimester of pregnancy is essential to identify and treat pregnant women with asymptomatic upper genital tract(10-12). It is known that Ureaplasma spp. can begin the synthesis of proinflammatory factors. Because of that, the initiation of the proper treatment before the onset of inflammation in both maternal and fetal territory will likely decrease the incidence of preterm birth and fetal complications significantly(3,7,12). Tedesco et al. reported no significant differences in the neonatal outcome of preterm newborns between women with or without screened infections(8).
In contrast to the aforementioned study, Rittenschiber-Bohm et al. indicate a possible association between vaginal Ureaplasma spp. infection in early pregnancy and adverse psychomotor outcome of the infant at 24 months corrected age(10).
This study further investigated the impact that chorioamnionitis has on fetal outcomes. We observed that chorioamnionitis directly correlates with a decrease in Apgar score. Also, the presence of funisitis was associated with a poor neonatal outcome. Chorioamnionitis is the consequence of the inflammatory response of the maternal organism to aggression that can be infectious or noninfectious (sterile intraamniotic inflammation)(1,4,5).
The diagnosis of chorioamnionitis is the sum of clinical signs by examining the histopathological and microbiological aspect of the placenta. Many cases of chorioamnionitis are subclinical and diagnosed retrospectively by histopathological examination of the placenta(6). This tendency highlights the need to reveal the factors responsible for the occurrence of acute/histological chorioamnionitis. The inflammatory response in the fetal territory (FIRS) is a risk factor and contributes to neonatal injury pathogenesis(10,12). Chorioamnionitis is associated with immediate severe complications (intrauterine growth restriction, fetal death, rapid-onset neonatal sepsis) and with distant sequelae (neurological lesions, intraventricular hemorrhage, bronchopulmonary dysplasia, persistence of the arterial duct, retinopathy of prematurity, cardiovascular disorder, necrotizing enterocolitis, dermatological lesions)(1,4,12). Fetal distress is the consequence of exposure to infectious pathogens, inflammatory mediators of amniotic fluid, and the first organs affected are the lungs, the gastrointestinal tract and the skin(1).
In our study, markers that can support the diagnosis and severity of intraamniotic infection/inflammation were the number of white blood cells and the CRP value at admission. We observed that an increased number of leukocytes and a higher value of CRP at admission were significantly associated with a decrease in Apgar score. Also, we noticed that the administration of antenatal steroids in male newborns had an essential effect on fetal outcomes.
In our study, the antibiotics administered (azithromycin and clarithromycin) did not influence the Apgar Score. Kacerovsky et al. showed that clarithromycin was associated with an attenuation of the intensity of the intraamniotic inflammatory response in patients with PROM(9). Currently, there is no explicit agreement about the specific regime of antibiotics or the optimal combination for patients with PROM to enhance maternal and fetal outcomes(7,9).
We tried to develop a feasible prediction model that can be applied for clinical management. We append to combine parameters with the statistical impact that can be determined at admission (gestational age, cervical length, genital infections in the first trimester of pregnancy) or within a few hours (leukocytes, CRP).
Strengths and limitations
One of the study’s strengths is the active management of PROM in our cohort, with most women delivering after seven days of latency period of membrane rupture. We included a thoroughly characterized cohort and rigorous perinatal follow-up. The diagnosis of infection was based on Multiplex Tandem Polymerase Chain Reaction (MT-PCR) using High-Plex 24 System (Aus Diagnostics).
In addition, the study presents some limitations. It was performed on a small number of patients, and the long-term neonatal outcome was not evaluated. Another limitation is that we did not analyze maternal, fetal or neonatal inflammatory cytokines or the amniotic fluid.
Conclusions
These results support further research in developing feasible multivariable prediction models in women with PROM below 34 weeks of gestation that could help clinicians manage low- and high-risk populations efficiently. In the high-risk group, the expected early delivery should be planned with antenatal strategies that improve the neonatal outcome.
Compliance with ethics requirements. The authors declare that all the procedures and experiments of this study respect the ethical standards in the Helsinki Declaration of 1975, as revised in 2008(5) and the national law. The informed consent was obtained from the patient described in the clinical case and from his parents.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Sweeney EL, Dando SJ, Kallapur SG, Knox CL. The human Ureaplasma species as causative agents of chorioamnionitis. Clin Microbiol. 2017;Rev 30:349-79.
-
Constantin AE, Pătraşcu O, Mehedinţu C, Carp-Velişcu A, Edu A, Frîncu F, Şandru F, Petca A, Dumitraşcu M, Cîrstoiu MM. Amniotic fluid sludge – a marker of intra-amniotic infection and histological chorioamnionitis in cervical insufficiency. Ro J Med Pract. 2021;16(Suppl 6):28-31.
-
Tantengo OAG, Yanagihara I. Current understanding and treatment of intra-amniotic infection with Ureaplasma spp. J Obstet Gynecol Res. 2019;45(9):1796-808.
-
Yoon BH, Romero R, Park JY, OH JK,Lee JH, Conde-Agueldo, Hong JS. Antibiotic administration can eradicate intra-amniotic infection or inflammation in a subset of patients with preterm labor and intact membranes. Am J Obstet Gynecol. 2019;221(2):142.e1-142.e22.
-
Theis KR, Romero R, Motomura K, Galaz J, Winters AD, Pacora P, Miller D, Slutsky R, Florova V, Levenson D, Para R, Varrey A, Kacerovsky M, Hsu CD, Gomez-Lopez N. Microbial burden and inflammasome activation in amniotic fluid of patients with preterm prelabor rupture of membranes. J Perinat Med. 2020;48(2):115–31.
-
Choi SJ, Park SD, Jang IH, Uh Y, Lee A. The prevalence of vaginal microorganisms in pregnant women with preterm labor and preterm birth. Ann Lab Med. 2012;32(3):194-200.
-
OH JK, Romero R, Park JY, Lee JH, Conde-Agueldo, Hong JS, Yoon BH. Evidence that amniotic administration is effective in the treatment of a subset of patients with intra-amniotic infection/inflammation presenting with cervical insufficiency. Am J Obstet Gynecol. 2019;221(2):142.e1-140.e18.
-
Tedesco RP, Galvão RB, Guida JP, Passini-Junior R, Lajos GJ, Nomura ML, et al. The role of maternal infection in preterm birth: evidence from the Brazilian Multicentre Study on Preterm Birth (EMIP). Clinics. 2020;75:e1508.
-
Kacerovsky M, Romero R, Stepan M, et al. Antibiotic administration reduces the rate of intraamniotic inflammation in preterm prelabor rupture of the membranes. Am J Obstet Gynecol. 2020;223(1):114.e1-20.
-
Rittenschober-Böhm J, Habermüller T, Waldhoer T, Fuiko R, Schulz SM, Pimpel B, Goeral K, Witt A, Berger A, Pichler K. Maternal vaginal Ureaplasma spp. Colonization in early pregnancy is associated with adverse short- and long-term outcome of very preterm infants. Children (Basel). 2021;8(4):276.
-
Cobo T, Kacerovsky M, Palacio M, Hornychova H, Hougaard DM, et al. Intra-amniotic inflammatory response in subgroups of women with preterm prelabor rupture of the membranes. PLoS One. 2012;7(8):e43677.
-
Sweeney EL, Kallapur SG, Gisslen T, Lambers DS, Chougnet CA, Stephenson SA, Jobe AH, Knox CL. Placental infection with Ureaplasma species is asssociated with histologic chorioamnionitis and adverse outcomes in moderately preterm and late-preterm infants. J Infect Dis. 2016;213(8):1340–7.
-
Motomura K, Romero R, Xu Y, Theis KR, Galaz J, Winters AD, Slutsky R, Garcia-Flores V, Zou C, Levenson D, Para R, Ahmad MM, Miller D, Hsu C-D, Gomez-Lopez N. Intra-amniotic infection with Ureaplasma parvum causes preterm birth and neonatal mortality that are prevented by treatment with Clarithromycin. mBio. 2020;11:e00797-20.
-
Kim JC, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, Kim MY. Acute chorioamnonitis and funisitis: Definition, pathologic features, and clinical significance. Am J Obstet Gynecol. 2015;213(40):s29-s52.
-
Cobo T, Aldecoa V, Figueras F, et al. Development and validation of a multivariable prediction model of spontaneous preterm delivery and microbial invasion of the amniotic cavity in women with preterm labor. Am J Obstet Gynecol. 2020;223:421.e1-14.




