Tipare de infertilitate. Un studiu de asistenţă medicală primară
Patterns of infertility. A primary care clinical study
Abstract
Background. Infertility represents a major medical and economic issue worldwide. There are few data regarding the pattern of infertility causes in Romania. Objective. The aim of this study was to determine if there is a pattern of the infertility causes in the Romanian population similar to those found in other countries. Materials and method. The charts of 67 couples referred to the Filantropia Clinical Hospital of Obstetrics and Gynecology, Bucharest, for infertility, between the 1st of January 2019 and the 1st of March 2020, were analyzed. Results. The average women’s age was 31.96 years old (standard deviation ± 3.6), while the average male age was 34.9 years old (standard deviation ± 5.87). The average duration of infertility was 2.5 years (standard deviation ± 2.37). In our study, an increased prevalence of the female factor (80.59%) was observed. Whilst in the female group the most frequent cause was the anovulatory disorders, including polycystic ovary syndrome (47.76%), the least frequent factor was the cervical factor (5.97%). Female-only factor was encountered in 47.76% of the couples. Regarding male infertility, after summing the isolated and mixed groups, the overall prevalence was 43.27%. Mixed infertility causes were observed in 32.83% of the couples. The idiopathic infertility was established after diagnostic procedures in 6 couples, representing 8.9% of the study group. Conclusions. Although it is difficult to establish, the identified pattern of infertility causes are similar to those presented in other developing countries, with a high prevalence of the female infertility. Further research is needed to establish a national pattern of infertility.Keywords
infertilityfemale factorsmale factorspatterns of infertilityRezumat
Introducere. Infertilitatea reprezintă o problemă medicală şi economică majoră în întreaga lume. Există puţine date referitoare la tiparele cauzelor de infertilitate în România. Obiectiv. Scopul acestui studiu este de a determina dacă există un model al cauzelor de infertilitate în populaţia din România, similar celor din alte ţări. Materiale şi metodă. Am analizat foile de observaţie a 67 de cupluri trimise la Spitalul de Obstetrică şi Ginecologie Filantropia din Bucureşti, pentru probleme de infertilitate, între 1 ianuarie 2019 şi 1 martie 2020. Rezultate. Media de vârstă a femeilor a fost 31,96 ani (deviaţie standard ± 3,6), în timp ce vârsta medie a bărbaţilor a fost 34,9 ani (deviaţie standard ± 5,87). Durata medie a infertilităţii a fost 2,5 ani (deviaţie standard ± 2,37). În studiul nostru am observat o creştere a prevalenţei factorului feminin (80,59%). În timp ce în grupul pacientelor cea mai frecventă cauză a fost considerată a fi cea a disfuncţiilor anovulatorii, incluzând sindromul ovarelor polichistice (46,76%), cel mai puţin frecvent factor a fost considerat factorul cervical (5,97%). Factorul feminin, ca unic factor de infertilitate, a fost întâlnit la 47,76% din cupluri. În ceea ce priveşte infertilitatea masculină, după sumarea grupurilor izolate şi mixte, prevalenţa globală a fost de 43,27%. Cauzele mixte de infertilitate au fost întâlnite la 32,83% din cupluri. Infertilitatea idiopatică a fost stabilită, după efectuarea procedurilor diagnostice, la şase cupluri, reprezentând 8,9% din grupul studiat. Concluzii. Deşi sunt dificil de stabilit, tiparele cauzelor de infertilitate identificate sunt similare celor descrise în alte ţări în curs de dezvoltare, cu o prevalenţă mare a infertilităţii feminine. Sunt necesare studii viitoare care să stabilească un model naţional de infertilitate.Cuvinte Cheie
infertilitatefactori femininifactori masculinitipare de infertilitateIntroduction
Infertility is considered a disease with important medical, psychosocial, demographic and economic consequences. It is defined as the inability of a couple to conceive after one year of unprotected intercourse(1). According to World Health Organization (WHO), in the developing countries, one in four couples faces infertility, while in developed countries this could rise to one in seven couples(1).
In Europe, the fertility rate has registered a decline since 1960 due to social dynamics: people are more career-oriented and the partnerships are also more unstable. People choose to postpone conception until after their thirties, when the risk of abortions, the fetal anomalies and the pregnancy risks are higher(1,2,4).
The infertility causes may vary amongst couples and is very dependent on socioeconomic factors. Nevertheless, there are some common patterns which can be identified. The most frequent causes of infertility are ovulatory disfunction (20-30%), tubal factor (15-20%), unknown/idiopathic infertility (15-28%), male factor (14-25%), endometriosis (6-11%), and sexual disfunctions (3-6%)(2-4).
Objective
Our objective was to evaluate the pattern of infertility causes in a Romanian population group, and to compare it to that reported in other countries.
Materials and method
We performed an observational, retrospective study which included 67 couples who were under evaluation for infertility in the Filantropia Clinical Hospital of Obstetrics and Gynecology, Bucharest, between the 1st of January 2019 and the 1st of March 2020. The infertility couples must have at least one year of failure of natural conception, except couples with known polycystic ovary syndrome (PCOS), endometriosis, or those older than 35 years of age, which we considered infertile after 6 months of unsuccessful natural conception(5).
We recorded age (for both women and men), weight, and height (for women).
At the time of clinical evaluation, we assigned each couple to an infertility diagnosis, primary or secondary.
We classified and registered female causes of infertility in the following: ovulation disorders, tubal factors, congenital anomalies, myomas and endometriosis. The ovulation disorders were classified using WHO criteria, including PCOS, which was defined using the Rotterdam criteria. Although it is still controversial, we decided to analyze the data which may indicate a low ovarian reserve with potentially poor ovarian response by using the antral follicle count (AFC) below 5/6 and AMH values under 1 ng/ml(5).
The male factor was assessed using the WHO 2010 criteria for semen analysis, being divided into four categories: number anomalies (oligospermia), motility anomalies (asthenospermia) and combinations (oligoasthenoteratozoospermia and asthenoteratozoospermia)(6).
We used Microsoft Windows Excel for the statistical evaluation of the data collected from the 67 couples. The data are presented as mean and standard deviation (SD) for quantitative variables and as percentages for nominal variables.
Body Mass Index (BMI) was calculated as kg/m2.
Results
General characteristics of the population
Women had an average age of 31.96 years old (SD±3.6), while the average male age was 34.9 years old (SD±5.87).
Regarding women’s BMI, this was 23.99 kg/m2 (SD±5.32).
There were only three cases of secondary infertility according to WHO definition of infertility.
The average duration of infertility was 2.5 years (SD±2.37).
Female causes of infertility
In the study group, there were 54 cases of women with at least one factor of infertility, representing 80.59%. Among them, the anovulatory infertility was responsible for 31 cases (47.7%), low ovarian reserve was discovered in 13 patients (19.4%), and tubal factor was discovered in 18 patients (33.9%). There were 5 congenital uterine abnormalities (7.46%), 9 patients had fertility associated with myomas (13.4%), cervical factor was implied in 4 cases (6,6%), and endometriosis was detected in 7 women (10%) – Figure 1.
Male causes of infertility
Semen analysis was performed using WHO 2010 criteria(7). Male factor alone was responsible for couple infertility in 7 cases (10.44%), while in mixt causes it was involved in 22 cases (32.83%).
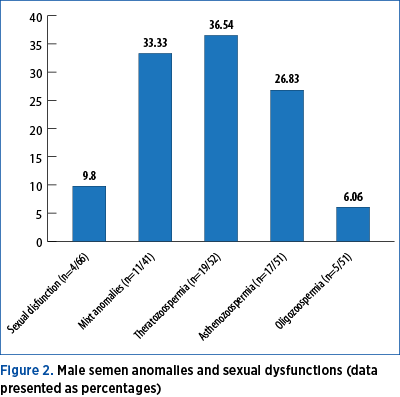
From the semen analysis, 5 cases (9.8%) had oligozoospermia, 17 cases (33.33%) had asthenospermia, 19 had teratozoospermia (36.63%), and 11 cases (26.8%) had combinations (asthenoteratozoospermia and oligoasthenoteratozoospermia). The couple’s history identified 4 cases with coital disorders (5.97%). The pattern is represented in Figure 2.

Infertility profile
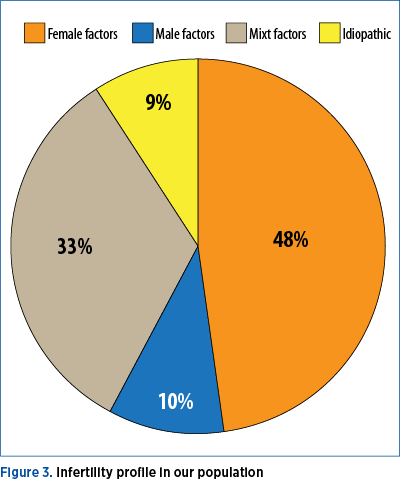
In our study, we observed an increased prevalence of the female factor (80.59%), whilst in the female group the most frequent cause was considered anovulatory disorders, including PCOS (47.76%), and the less frequent was the cervical factor, represented by stenosis (5.97%). Female factor as unique cause was encountered in 47.76% of the couples.
Regarding male infertility, after summing the isolated and mixed groups, the overall prevalence was 43.27%.
Mixed infertility causes were observed in 32.83% of the couples.
The idiopathic infertility was established, after diagnostic procedures, in 6 couples, representing 8.9% of the study group. The distribution is represented in Figure 3.
Discussion
Although its prevalence is constant all over the world, infertility has become a major public health issue due to demographic decline. This happens even in the developing countries. Addressing not only to one person but to the couple, infertility becomes a complex problem difficult to analyze and define. There is a myriad of variable data which have to be taken into consideration. The definition of the causes varies widely among the studies, making it problematic to create a pattern of infertility for a certain population.
In our study, the average age was 31 years old for women and 35 years old for men, while the average infertility duration was 2.5 years. The average age is matching the one found in the developed countries(7,8). We observed a delay in the parenthood decision and, sometimes, even a reduced desire of childbearing if this does not naturally occur. In contrast with the developed countries, there is a delay in addressing to specialised medical care, as well(9).
As expected, the female causes prevalence increased with age(10).
The prevalence of female causes appears to be very high (80.59%), but this may be correlated with the fact that the Filantropia Clinical Hospital is a center of primary care for infertility patients and they are not selected, as it happens in in vitro fertilization (IVF) clinics. Often, the female causes are not clearly defined among the studies. There could be a difference between their simple presence versus the actual contribution to the couple infertility.
The female infertility pattern found in our study matched the worldwide established intervals and is similar to those found in the developing countries(10).
The most frequent female factors were ovulation disorders, which are estimated to 47.77%.
These rates were comparable to those reported in Russia, North-Eastern Africa and Israel (28.43-37.46%)(11-13). Recent studies report the highest prevalence of anovulatory disorders in the Mexican population (82.7%)(14).
A special group of patients were those with reduced ovarian reserve, with AMH, FSH, LH and estradiol levels and AFC, which will predict a poor response to ovarian stimulation. They also had cycle anomalies, which reveal inconstant ovulation(5).
The tubal factor was responsible for 33.9% of the women, which matches to the global pattern ranging from 13.80% in Israel to a maximum of 39.50% in Nigeria(13,15).
Uterine and cervical factors represent 18.40% of the analyzed population. This exceeds a little the rate mentioned by NICE guidelines, which ranges between 10% and 15%(4). The infertile Mexican population has one of the highest rates of uterine anomalies (15%)(14).
Endometriosis prevalence was 10%, but we only included those women who underwent laparoscopy with histopathological confirmation. The rate appears to be much higher if we agree that many patients were highly suspicious of endometriosis, but they did not have laparoscopy.
The prevalence of endometriosis among infertile women varies widely, between 2.5% and 50%(14,16,17).
Male factor was involved in 43.26% of the cases. This rate is similar to those reported in Israel, North-East of Africa and Mongolia(12,13,19). The prevalence ranges from 6.5% to 50% worldwide(7,15,19,20).
Motility and morphology anomalies were the most frequent, with a rate of 33.33% and 36.63%, respectively. Regarding combinations, astenoteratozoospermia and oligoteratozoospermia shared almost the same number of cases and, combined, reached a total of 26.8%. No azoospermic male was identified. This is probably correlated with the low number of couples analyzed or due to the meticulous application of standardized centrifugation procedures on the semen samples.
Idiopathic infertility is still a matter of debate. The European Society of Human Reproduction and Embryology (ESHRE) establishes that a couple should be labelled with unknown infertility after the general tests have failed to find a cause, but that does not mean that there is none. It is the limit of our knowledge and the limits of tests we perform which made this diagnosis possible. The present theoretical causes (oocyte and sperm quality, tubal function, impaired endometrial receptivity) will probably become certainties tomorrow. After applying the ESHRE recommended standard tests (ovulation, uterine and tubal patency, and semen analysis), our study revealed only six couples with idiopathic infertility (8.9%), a rate comparable to those found in India and Mexico(14,19).
Conclusions
Infertility is a disease with major medical and socioeconomic impact, a demographic burden in the developing countries. It is a complex and fluid concept with a lot of causes, and sometimes it can be difficult to determine a specific pattern. The major observation of this study was that the pattern discovered in the primary care clinics was slightly different to that found in fertility clinics. This pattern resembles the one found in the general unselected population. Therefore, further studies are needed to create a realistic image of the distribution of the infertility causes in the general population.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
1. Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren R, Sullivan E, Vanderpoel S, for ICMART and WHO. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertility and Sterility. 2009; vol 92, No.5, available at: www.who.int.
2. Kuohung W, Barbieri R, Eckler K. Overview of infertility. UpToDate. Available at: www.uptodate.com, last updated February 27, 2020.
3. Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PI, Hinton RA, Coulson C, Lambert PA, Watt EM, Desai KM. Population study of cases, treatment, and outcome of infertility. Br Med J (Clin Res Ed). 1985; 291(6510): 1693.
4. Fertility: Assessment and treatment for people with fertility problems. February 2013, NICE Clinical Guideline.
5. Infertility workup for the women’s health specialist. ACOG Committee Opinion No. 781. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2019; 133:e377–84.
6. WHO laboratory manual for the examination and processing of human semen. Fifth edition, 2010.
7. Wilkes S, Chinn DJ, Murdoch A, Rubin G. Epidemiology and management of infertility: a population-based study in UK primary care. Fam Pract. 2009 Aug; Volume 26, Issue 4, 269–274.
8. Swift BE, et al. The Effect of Age, Ethnicity, and Level of Education on Fertility Awareness and Duration of Infertility. Journal of Obstetrics and Gynaecology of Canada. 2014; Volume 36, Issue 11, 990–996.
9. World Health Organization. Recent advances in medically assisted conception: report of a WHO scientific group meeting of the WHO scientific group on recent advances in medically assisted reproduction held in Geneva from 2 to 6 April 1990. Geneva: World Health Organization; 1992.
10. Female age-related fertility decline. Commitee Opinion No. 589. American College of Obstetricians and Gynecologists. 2014; 123 719-21.
11. Philippov OS, et al. Estimation of the prevalence and causes of infertility in Western Siberia. Bulletin of the World Health Organization. 1998; vol. 76, 2: 183-7.
12. Elhussein OG, Ahmed MA, Suliman SO, et al. Epidemiology of infertility and characteristics of infertile couples requesting assisted reproduction in a low-resource setting in Africa, Sudan. Fertil Res and Pract. 2019; 5:7.
13. Farhi J, Ben-Haroush A. Distribution of causes of infertility in patients attending primary fertility clinics in Israel. Isr Med Assoc J. 2011; 13(1):51-54.
14. Vite J, Ortiz D, Hernández I. Análisis epidemiológico de la Infertilidad en una población mexicana. México: Ginecol Obstet. 2005 Jul; 73(7):360-4.
15. Sule JO, Erigbali P, Eruom L. Prevalence of Infertility in Women in a Southwestern Nigerian Community. Afri J Biomed Res. 2008; 11:225–7.
16. Ozkan S, Murk W, Arici A. Endometriosis and Infertility. Annals of the New York Academy of Sciences. 2008, 1127: 92-100.
17. Bablok L, Dziadecki W, Szymusik I, Wolczynski S, Kurzawa R, Pawelczyk L, et al. Patterns of infertility in Poland – a multicenter study. Neuro Endocrinol Lett. 2011; 32:799–804.
18. Bayasgalan G, Naranbat D, Tsedmaa B, Tsogmaa B, Sukhee D, Amarjargal O, et al. Clinical patterns and major causes of infertility in Mongolia. J Obstet Gynaecol Res. 2004; 30:386–93.
19. Oberoi S, Khaira R, Rai SK. Aetiology of Infertility: An Epidemiological Study. Ntl J Community Med. 2017; 8(1):17-21.
20. Jarvi K, Lo K, Grober E, Mak V, Fischer A, Grantmyre J, et al. The workup and management of azoospermic males. Can Urol Assoc J. 2015; 9:229–35.




