We present the case of a 69-year-old non-smoker male who came to the hospital for dyspnea, thoracic pain, hemoptysis, loss of appetite and involuntary weight loss, evolving for two months. The thorax-CT scan revealed a giant lung tumor involving the right upper lobe and part of the middle lobe, with pleural invasion. The patient was known with an osteosarcoma (malignant fibrous histiocytoma-like; MFH-like) of the spine surgically removed 10 years ago and treated with chemotherapy. The initial biopsy of the tumor that invaded the anterior parietal pleura was not conclusive, this fact requiring a surgical intervention with both a diagnostic and therapeutic role. Thus, superior bilobectomy was performed, which was associated with a complete right mediastinal lymph node dissection. The postoperative course was favorable and uneventful. The histopathological findings and immunohistochemistry staining revealed a giant lung osteosarcoma metastasis, MFH-like subtype, and no metastasis in the mediastinal lymph nodes. The peculiarity of the case is represented by the evolution of a single osteosarcoma metastasis with very large dimensions after more than 10 years.
Giant solitary lung metastasis from an osteosarcoma (malignant fibrous histiocytoma-like) of the spine
Metastază pulmonară solitară voluminoasă de osteosarcom (cu aspect de histiocitom fibros malign) al coloanei vertebrale
First published: 31 mai 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.59.2.2022.6537
Abstract
Rezumat
Prezentăm cazul unui bărbat nefumător, în vârstă de 69 de ani, care a venit la spital pentru dispnee, dureri toracice, hemoptizie, pierderea poftei de mâncare şi scădere involuntară în greutate, simptomatologie în progresie de două luni. Tomografia computerizată toracică relevă o formaţiune tumorală pulmonară gigantică ce ocupă lobul superior drept şi invadează parţial lobul mediu şi pleura parietală adiacentă. Pacientul este cunoscut cu un osteosarcom (histiocitom fibros malign-like; HFM-like) al coloanei vertebrale, operat (rezecţie completă) în urmă cu 10 ani şi tratat cu chimioterapie adjuvantă. Biopsia iniţială a tumorii care invadează pleura parietală anterioară nu a fost concludentă, acest fapt necesitând o intervenţie chirurgicală atât cu rol diagnostic, cât şi terapeutic. Astfel, s-a efectuat bilobectomie superioară, care a fost asociată cu limfadenectomie mediastinală completă. Evoluţia postoperatorie a fost favorabilă şi fără complicaţii. Rezultatul histopatologic şi testele imunohistochimice au arătat o metastază pulmonară gigantă de osteosarcom, subtipul MFH-like; ganglionii limfatici mediastinali nu au fost metastazaţi. Particularitatea cazului este reprezentată de evoluţia unei metastaze unice de osteosarcom cu dimensiuni foarte mari, după mai bine de 10 ani.
Introduction
Osteosarcoma is a rare primary malignant tumor of bone that is characterized by an osteoid matrix produced by the malignant cells(1,3). Bone tumors make up about 3-5% of childhood cancers and less than 1% of cancers in adults. Of these, osteosarcoma is the most common primary malignancy of bone in children as well as adolescents and young adults (AYAs) aged 15 to 19(4-6). Osteosarcoma (OS) has a well-recognized double peak of incidence. The majority arise in adolescence, but there is a significant second peak in the seventh and eighth decades of life. Osteosarcoma that arises in patients older than 40 years of age can be associated with Paget disease, a focal skeletal disorder characterized by an accelerated rate of bone turnover(6,7). There is a wide variety of osteosarcoma subtypes, but in adults over the age of 40 the most common subtypes are conventional osteosarcoma and malignant fibrous histiocytoma-like (MFH-like)(8). The five-year survival rate is higher in patients with MFH-like osteosarcoma compared with patients with conventional osteosarcoma. The relapse of osteosarcomas is usually as lung metastasis observed within 2 to 3 years after the initial treatment. A relapse is rarely observed at more than 10 years(9).
Case report
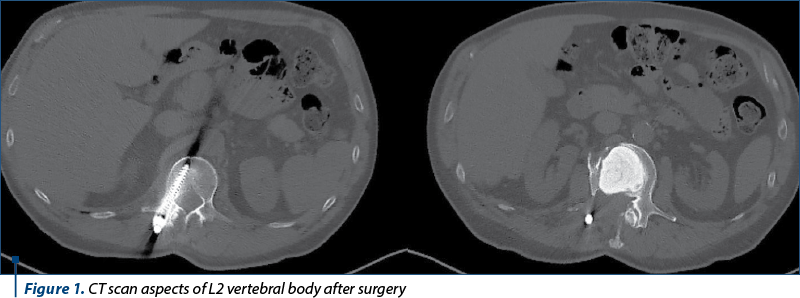
We present the clinical case of a 69-year-old patient, former smoker (40 pack-year), known with an osteosarcoma (malignant fibrous histiocytoma-like) of the spine (L2 vertebral body), surgically removed 10 years ago (with vertebral reconstruction) – Figure 1. The microscopic and immunohistochemical findings of the initial tumor (osteonectin positive, S-100 positive, CD64 positive, CD34 positive) sustain the high-grade osteosarcoma diagnosis, subtype malignant fibrous histiocytoma-like. The patient was referred to the oncologist and treated with adjuvant chemotherapy (epirubicin and cisplatin).
Since there was no sign of local or metastatic recurrence at two years after that treatment, the patient stopped visiting the hospital. The patient was referred to our hospital 10 years after that with a three-month history of right posterior thoracic pain, hemoptysis, cough, respiratory distress, involuntarily wight loss and lack of appetite.
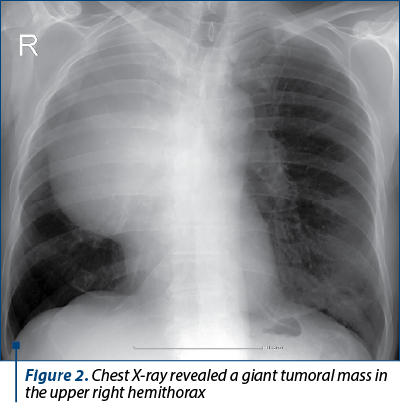
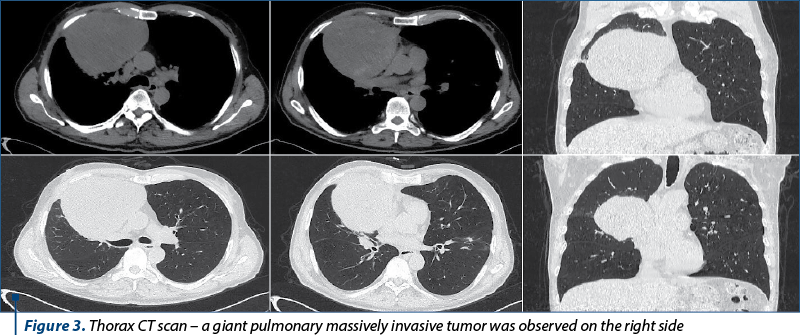
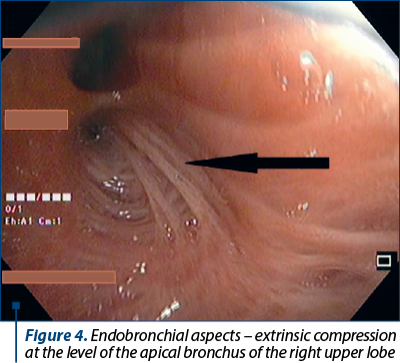
At the time of admission in our department, the hematology and biochemistry tests were almost normal. Chest X-ray revealed a giant tumoral mass in the upper right hemithorax and paradox tracheal retraction (right minor mediastinal displacement) explained secondary to scoliosis (Figure 2). Primary lung cancer was suspected. Thorax CT scan was performed and a giant pulmonary massively invasive tumor was observed on the right side, involving the almost entire right upper lobe and part of the middle lobe with almost 21 cm in its greatest dimensions (Figure 3). The patient underwent a bronchoscopy that found a free bronchial tree with no endobronchial tumors; extrinsic compression (narrowing) was noted at the level of the apical bronchus of the right upper lobe, as well as of the medial segmental bronchus of the middle lobe (Figure 4).
To obtain a definitive diagnosis, a transthoracic biopsy was performed. The histopathological examination described fragments of fibroconjunctival tissue and alveolar pulmonary parenchyma with fibrosis, chronic nonspecific inflammatory infiltrate, atypical adenomatous alveolar hyperplasia; reactive mesothelial hyperplasia; adjacent reactive-looking lymphoid structures. Immunohistochemical tests concluded a result without tumor cells.
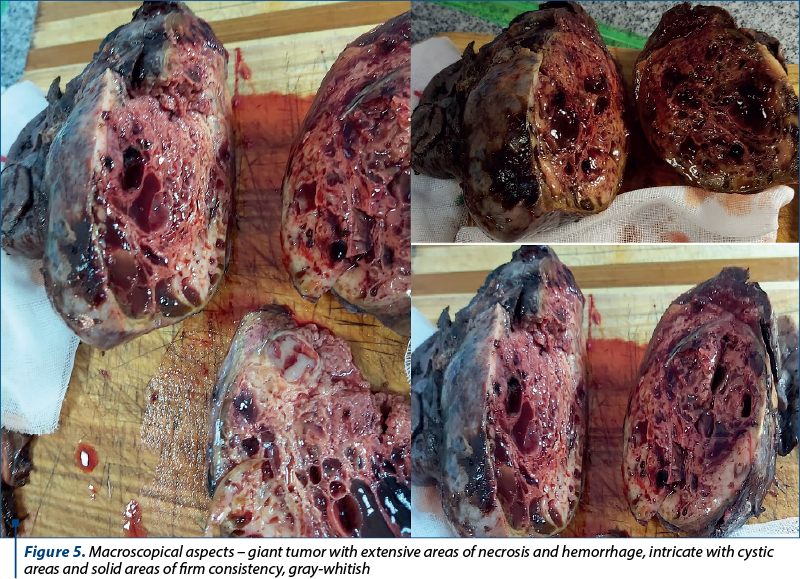
The case was discussed in the tumor board session and the recommendation was for surgical approach with a dual role: diagnostic and therapeutic. Thus, through a thoracotomy through the 5th intercostal space, we accessed the pleural cavity where we detected a large tumor mass that completely occupied the upper and invades part of the middle lobe. We decided to perform a superior bilobectomy with a complete right mediastinal lymph node dissection. The surgical resection specimen revealed a large tumoral mass of 14.5/14/9 cm extending in the right upper and middle lobes, well-demarcated and outlined by a thick fibrous capsule from the surrounding pulmonary tissue. The cut surface of the tumor was fleshy with extensive areas of necrosis and hemorrhage with blood-filled cystic spaces separated by fibrous septa (Figure 5).
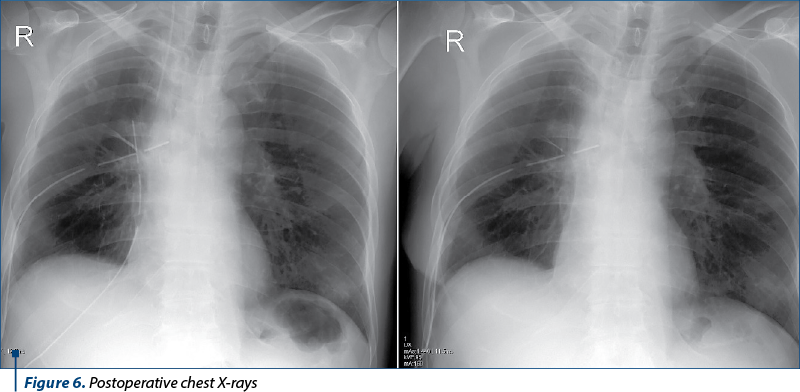
The patient had a favorable clinically and imaging evolution, being discharged on the sixth day postoperatively (Figure 6).
The histopathological examination showed a proliferation of pleomorphic and bizarre tumor cells with severe cytological atypical producing lace-like tumoral osteoid tissue. Extensive areas of necrosis and hemorrhage were present. Increased mitotic activity with frequent typical and atypical mitotic figures (Figure 7) were noted; no metastasis in mediastinal lymph nodes was observed.
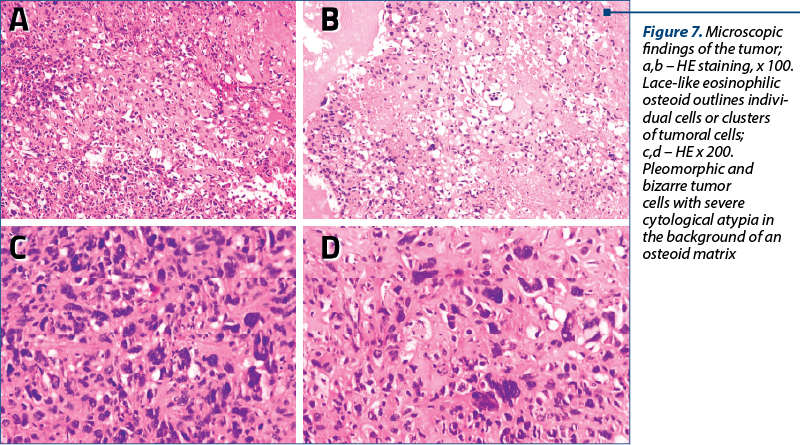
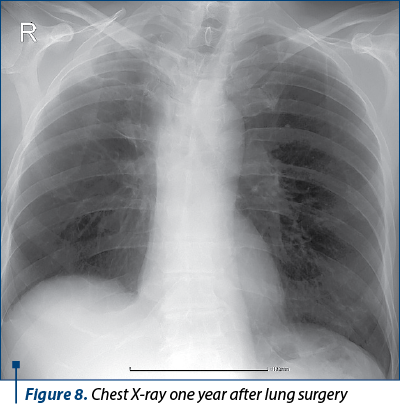
Immunohistochemical staining for osteonectin was diffusely positive, whereas those for SATB2, Calretinin, ERG, TTF1, CK7, ACT and S-100 protein were negative. The final diagnosis was a very late lung metastatic recurrence of high-grade osteosarcoma. Adjuvant chemotherapy was planned and the patient received six courses of gemcitabine and docetaxel. The patient has been free of the disease for more than eight months (Figure 8).
Discussion
Osteosarcoma is the third most common cancer in adolescence, after lymphomas and brain tumors. One-third of patients who present with osteosarcoma will have recurrent disease. Within the recurrent disease group, 95% of relapses occur within the first five years, with the lung as the most common site of metastases(1,2,3,4,8,9). Osteosarcoma (OS) has a well-recognized double peak of incidence. The majority arise in adolescence, but there is a significant second peak in the seventh and eighth decades of life(6).
The incidence of OS is common in the metaphysis of long tubular bones, but rare in the spine, pelvis and sacrum areas(10).
There is a wide variety of osteosarcoma subtypes, but in adults over the age of 40 the most common subtypes are conventional osteosarcoma and MFH-like.
Histologically, the MFH-like osteosarcoma was characterized by the presence of tumor osteoid and/or bone, which varied in quantity from case to case, varied in appearance from small foci to large masses, and coexisted with storiform-pleomorphic type MFH-like areas(8).
Late relapse of osteosarcoma is defined as local or metastatic recurrence at ≥5 years after the initial treatment. In low-grade central osteosarcoma cases, the incidence rate of late relapse was relatively high, and it occurred in 5.5% to 30% of the cases. In contrast, late relapse of high-grade osteosarcoma is rare, with an incidence of 0.6% to 2.9%. Very late relapse, defined as local or metastatic recurrence at ≥10 years after the initial treatment, rarely occurs (0-0.4%) in high-grade osteosarcoma cases(9-11).
Very late relapse is thus extremely rare. To the best of our knowledge, only 18 cases of high-grade osteosarcoma, including the present case, have been published as a case report or part of a case series or large cohort study(9-12). In literature, we found a paper that presents an osteosarcoma case with a pulmonary metastatic relapse after 38 years(8). The overall survival and the disease-free survival in osteosarcoma patients have been prolonged by recent progress in multimodality therapy, and thus clinicians as well as osteosarcoma patients should always keep in mind the possibility of very late relapse(9). The osteosarcoma subtype has its importance in good or poor disease prognosis; MFH-like subtype has better prognosis compared to conventional osteosarcoma(8).
The peculiarity of the case we presented is given by the following: the rare localization at the level of the spine of the primary osteosarcoma, the very late recurrence (at more than 10 years) by a giant, solitary lung metastasis, the possibility to perform R0 resections in both surgical procedures and the favorable clinical and oncological evolution.
Conclusions
This case highlights the importance of long follow-up periods and continued surveillance of osteosarcoma patients after the initial curative treatment.
Osteosarcoma remains a challenging disease to treat. Surgical excision in association with chemotherapy is essential for cure.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Horvat T (coord.). Metastazele pulmonare. În: Tratat de chirurgie. Vol IV – Chirurgie Toracică. Sub redacţia: Irinel Popescu, Editura Academiei Române, Bucureşti, 2008, p. 619-627.
-
Baumhoer D, Böhling TO, Cates JMM, et al. Osteosarcoma. In: WHO Classification of Tumours Soft Tissue and Bone Tumours, 5th ed, The WHO Classification of Tumours Editorial Board (Ed), IARC Press, 2020. p.403.
-
Mirabello L, Troisi RJ, Savage SA. International osteosarcoma incidence patterns in children and adolescents, Middle Ages and elderly persons. Int J Cancer. 2009;125(1):229-234. doi:10.1002/ijc.24320
-
Data from the American Cancer Society. Available at: https://www.cancer.org/cancer/osteosarcoma/about/key-statistics.html (Accessed on April 17, 2021).
-
Howlader N, Noone AM, Krapcho M, et al (eds). SEER Cancer Statistics Review, 1975-2018, National Cancer Institute. Bethesda, MD, based on November 2020 SEER data submission, posted to the SEER web site, April 2021. https://seer.cancer.gov/csr/1975_2018/ (Accessed on April 17, 2021).
-
Grimer RJ, Cannon SR, Taminiau AM, Bielack S, Kempf-Bielack B, Windhager R, Dominkus M, Saeter G, Bauer H, Meller I, Szendroi M, Folleras G, San-Julian M, van der Eijken J. Osteosarcoma over the age of forty. Eur J Cancer. 2003 Jan;39(2):157-63. doi: 10.1016/s0959-8049(02)00478-1. PMID: 12509946.
-
Naka T, Fukuda T, Shinohara N, Iwamoto Y, Sugioka Y, Tsuneyoshi M. Osteosarcoma versus malignant fibrous histiocytoma of bone in patients older than 40 years. A clinicopathologic and immunohistochemical analysis with special reference to malignant fibrous histiocytoma-like osteosarcoma. Cancer. 1995 Sep 15;76(6):972-84. doi: 10.1002/1097-0142(19950915)76:6<972::aid-cncr2820760610>3.0.co;2-t. PMID: 8625223.
-
Kaneuchi Y, Hakozaki M, Yamada H, Hasegawa O, Yamada S, Oka Y, Watanabe K, Konno S. Very late relapse of high-grade osteosarcoma: A case report and review of the literature. Medicine (Baltimore). 2020 Jul 17;99(29):e21206. doi: 10.1097/MD.0000000000021206. PMID: 32702886; PMCID: PMC7373632.
-
Halldorsson A, Brooks S, Montgomery S, Graham S. Lung metastasis 21 years after initial diagnosis of osteosarcoma: a case report. J Med Case Rep. 2009 Nov 24;3:9298. doi: 10.1186/1752-1947-3-9298. PMID: 20062787; PMCID: PMC2803821.
-
Zhao X, Wu Q, Gong X, Liu J, Ma Y. Osteosarcoma: a review of current and future therapeutic approaches. Biomed Eng Online. 2021 Mar 2;20(1):24. doi: 10.1186/s12938-021-00860-0. PMID: 33653371; PMCID: PMC7923306.
-
Ferrari S, Briccoli A, Mercuri M, Bertoni F, Cesari M, Longhi A, Bacci G. Late relapse in osteosarcoma. J Pediatr Hematol Oncol. 2006 Jul;28(7):418-22. doi: 10.1097/01.mph.0000212944.82361.1d. PMID: 16825986.
-
Le BH, Buchanan MR, Steer C, de Boer R. Late recurrence of osteosarcoma. Intern Med J. 2007 Jun;37(6):420-2. doi: 10.1111/j.1445-5994.2007.01346.x. PMID: 17535392.
Articole din ediţiile anterioare
Tumoare germinală testiculară nonseminomatoasă cu prognostic rezervat
Prezentăm cazul unui pacient în vârstă de 37 de ani, fără antecedente patologice semnificative, care s-a prezentat la camera de gardă cu dispnee ...