The current paper performs an overview of definitions given to specific concepts linked with exposure to adversity, such as: traumatic event, trauma, post-traumatic stress. Furthermore, we outline trauma as a process, as encounter of person, context and traumatic event, and what the experience of trauma represents for the person and community, on a subjective, cognitive, intra- and interpersonal systems level. Also, we address the pathways of development and evolution of the trauma for the bearing person.
Trauma – experienţa individuală, contextul şi trasee de dezvoltare
Trauma – individual experience, context and pathways of evolution
First published: 30 noiembrie 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.71.4.2022.7327
Abstract
Rezumat
Acest articol trece în revistă definiţiile furnizate de-a lungul timpului pentru unele concepte specifice asociate cu expunerea la adversităţi, precum: eveniment traumatizant, traumă, stres posttraumatic. De asemenea, articolul conceptualizează trauma ca proces, ca întâlnire dintre persoană, context şi evenimentul traumatizant, precum şi ceea ce reprezintă trauma pentru persoană şi comunitate la nivel subiectiv, cognitiv, intra- şi interpersonal şi al sistemelor sociale. De asemenea, articolul abordează potenţialele trasee de dezvoltare şi evoluţie ale persoanei purtătoare a traumei.
Introduction
Persons, communities and humanity as a whole share the experience of exposure to adversities. While this experience is not pathological per se(1), the person – development – event – context – timing interplay generates unique trajectories of adaptation to adversities, which in turn permeate to various extents the existence of persons and communities, from the level of daily functioning to the sense of self(2).
Since the coining of pathological consequences of exposure to adversity as post-traumatic stress disorder in 1980(3), changes in society have led to shifts in the understanding of both adverse events with traumatic potential, and detrimental effects of exposure to adversity(4). The plethora of psychological trauma studies validate their usefulness when translated into more effective and better tailored strategies of trauma management – i.e., trauma-informed practice(5).
Definitions
After a brief separation, current American(6) and international(7) classifications of mental disorders operate with similar understanding and definitions of concepts related to psychological experiences of exposure to adversity. They define traumatic events as external adversities that pose a clear, pervasive threat to the person’s life, physical and psychological integrity and functioning. The newly defined complex traumatic events additionally involve repetitive, prolonged, serial exposure to extremely horrific, complex events (such as repeated child abuse, torture, slavery, genocide, organized violence), and impossibility to escape(6,7).
The exposure to traumatic events is not pathological per se(8). It occurs directly or vicariously – i.e., by witnessing others who are exposed or by exposure via media, and may affect persons and communities; the person encounters the event during a specific time in their development trajectory. Moreover, the relationship between exposure to traumatic events and subsequent mental health issues is nonlinear, not limited to psychiatric disorders directly related to specific events, and it is shaped by a multitude of factors(6-8). The term trauma encompasses a process of both objective and subjective experiences resulting from the person – development – traumatic event – context interplay(8). Post-traumatic stress disorder (PTSD) represents the patterns of psycho-physiological reactions generated by the interaction with the traumatic event with the purpose of adjustment, which become repetitive, intrusive and pervasive and affect the functioning. Complex post-traumatic stress includes the aforementioned features, and patterns of persistent, pervasive, significant impairment in self-concept and affect regulation, shame and guilt, disrupted connectedness and social relationships(6,7).
The experience of trauma
For persons and communities, the traumatic event represents a reference for new experiences, comparison for current experiences, comparison for how to think and feel about other events. The event is seen as splitting life into two – before and after, connecting and bringing together all threads of the person’s life story, irreversibly shaping existence and leaving permanent marks in the person’s life course. Moreover, everything in the person’s life may be seen as entangled with the event(9).
Exposure to the traumatic event also shapes the flow of thinking of the person, by changing the way of thinking about life in general, about the person’s future. The way the person understands and interprets present, future and even past events is changed by the traumatic event; additionally, whenever the person thinks about his/her future, the traumatic event is automatically recalled from memory and the person thinks about it and about its influence on their future(10).
The impact of traumatic events on identity and destiny
The exposure to traumatic events and the subsequent trauma become representative of who the person is, how they understand themselves and others, and how they relate to others. It becomes a symbol of what is relevant, particular and specific in the person and their life, compared with others and other lives(11). Moreover, it influences self/identity expression and the relationship with the self, others and the world, and irreversibly switches the course of life. The persons thinks of themselves as different because of the traumatic event happening (“If it hadn’t happened, I would have been a different person”)(12,13).
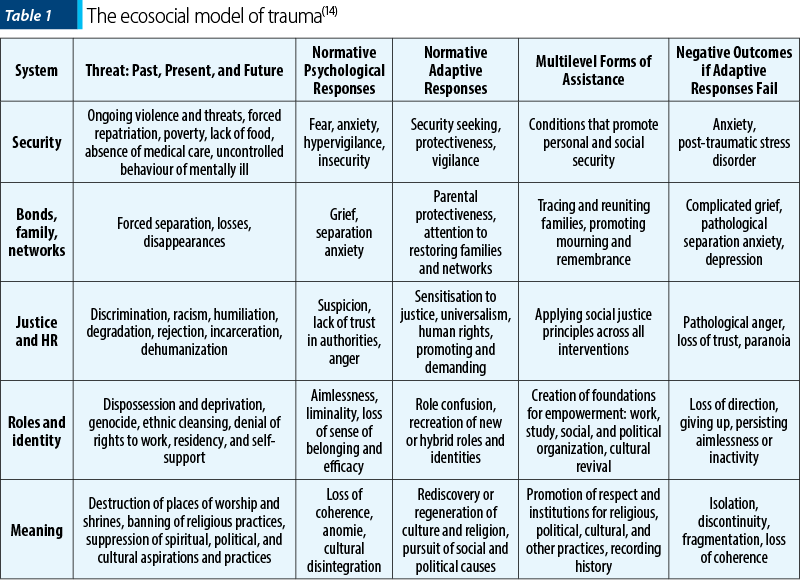
Trauma disrupts not only the person, but also the social systems and global community as a whole, due to its collective and vicarious nature. The ecosocial model of trauma acknowledges the levels of system disruption, reflected in unsafe physical environment for persons and groups, disrupted community relationships, social injustice and inequity, disrupted social roles and disrupted sense of meaning. While identifying how entire communities struggle with the multi-layered impact of pervasive trauma, the ecosocial model also proposes multi-layered interventions to restore the sense of safety, connectedness, social justice and equity, empowerment, coherence and meaning in persons and communities – Table 1(14).
Pathways of trauma, from pathology
to adaptation and growth
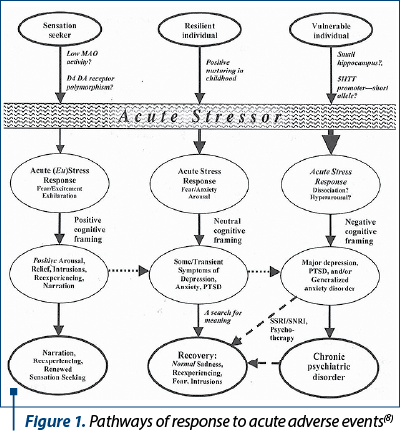
Dwelling on the paradigm of adaptation to stress, some authors proposed a model that incorporates the response to trauma exposure in a continuum, from negative framing combined with individual vulnerabilities, which likely leads to mental health issues, to positive framing combined with individual characteristics, which would lead to post-traumatic adaptation and even growth (Figure 1). The model acknowledges that the pathway to recovery and/or growth may include both transient psychological symptoms and persistent reexperiencing (cognitive processing) of the event. However, it underscores an overall dichotomous outcome of exposure to trauma (disruption versus adaptation)(8).
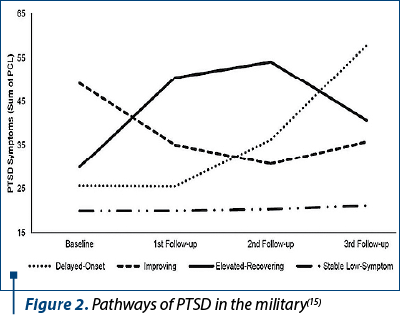
Insight from military populations ascertains four distinct pathways of evolution of post-traumatic stress symptoms: delayed onset, intense early onset with gradual recovery, gradual onset and gradual recovery, and stable low-level symptoms (Figure 2)(15).
Trauma and the post-pandemic society
The most recent model of post-traumatic stress (PTS) and post-traumatic growth (PTG), developed in the post-pandemic era, ascertains a direct pathway to PTG and validates that negative (PTS) and positive (PTG) outcomes share the common predictors of event centrality and unhelpful versus helpful disclosure. Most notably, core-belief disruption and deliberate rumination are significant predictors for post-traumatic growth(16).
In the current, post-pandemic world, exposure to traumatic events is pervasive and ubiquitous; increased stress levels emerge as a public health issue, and global socioeconomic determinants of health influence risk and resilience factors. This means that the level of mental and physical health is influenced by the social systems: health inequities both increase the exposure to traumatic events, and act as barriers to effective, comprehensive care for those who need it most. Resilience in the face of adversity includes social support and development of evidence-based strategies, tailored to, and delivered in the community(17).
Bibliografie
-
Benjet C, Bromet E, Karam EG, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. 2016 Jan;46(2):327-43.
-
Konner M. Trauma, adaptation and resilience: a cross-cultural and evolutionary perspective. In: Kirmayer LJ, Lemelson R, Barad M, editors. Understanding trauma. Integrating biological, clinical and cultural perspectives. New York (NY): Cambridge University Press, 2007, p. 300-338.
-
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (3rd ed.). American Psychiatric Association: Washington (DC), 1980.
-
Benedek DM, Ursano RJ. Posttraumatic stress disorder: from phenomenology to clinical practice. Focus. 2009;7(2):160-175.
-
Shalev AY. PTSD: A Disorder of Recovery? In: Kirmayer LJ, Lemelson R, Barad M, editors. Understanding trauma. Integrating biological, clinical and cultural perspectives. New York (NY): Cambridge University Press, 2007, p. 207-223.
-
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association: Washington (DC), 2013.
-
World Health Organization. ICD-11: International classification of diseases (11th revision). World Health Organization, 2019. Retrieved from https://icd.who.int/
-
Konner M. Trauma, adaptation and resilience: a cross-cultural and evolutionary perspective. In: Kirmayer LJ, Lemelson R, Barad M, editors. Understanding trauma. Integrating biological, clinical and cultural perspectives. New York (NY): Cambridge University Press, 2007, p. 300-338.
-
Gehrt TB, Berntsen D, Hoyle RH, Rubin DC. Psychological and clinical correlates of the Centrality of Event Scale: A systematic review. Clin Psychol Rev. 2018 Nov;65:57-80.
-
Berntsen D, Nielsen NP. The reconstructive nature of involuntary autobiographical memories. Memory. 2022 Jan;30(1):31-36.
-
Kongshøj ILL, Bohn A, Berntsen D. To mention or not to mention? The inclusion of self-reported most traumatic and most positive memories in the life story. Memory. 2022 Feb;30(2):133-146.
-
Marin KA, Shkreli A. An examination of trauma narratives: Narrative rumination, self-reflection, and identity in young adulthood. J Adolesc. 2019 Oct;76:139-151.
-
Berman SL, Montgomery MJ, Ratner K. Trauma and identity: A reciprocal relationship? J Adolesc. 2020 Feb;79:275-278.
-
Silove D. Adaptation, Ecosocial Safety Signals, and the Trajectory of PTSD. In: Kirmayer LJ, Lemelson R, Barad M, editors. Understanding trauma. Integrating biological, clinical and cultural perspectives. New York (NY): Cambridge University Press, 2007, p. 207-223.
-
Porter B, Bonanno GA, Frasco MA, Dursa EK, Boyko EJ. Prospective post-traumatic stress disorder symptom trajectories in active duty and separated military personnel. J Psychiatr Res. 2017 Jun;89:55-64.
-
David G, Shakespeare-Finch J, Krosch D. Testing theoretical predictors of posttraumatic growth and posttraumatic stress symptoms. Psychol Trauma. 2022 Mar;14(3):399-409.
-
Johnson S. In: Times of Adversity: A Neuroscience Perspective on Stress, Health, and Implications for Society Post-pandemic. Yale J Biol Med. 2022 Mar 31;95(1):165-170.
Articole din ediţiile anterioare
Canabidiolul – zeci de ani de cercetare şi utilizările clinice actuale
Deşi majoritatea cercetărilor referitoare la canabis s-au concentrat asupra delta-9-trans-tetrahidrocanabinolului (THC), recent alte componente ale...
Trauma psihică a expunerii la infecţia cu SARS-CoV-2
După mai mult de un an de expunere globală la COVID-19, la consecinţele acesteia asupra stării de sănătate şi la măsuri variabile de limitare a răs...
Tulburări psihice asociate traumatismului craniocerebral
Traumatismul craniocerebral necesită o abordare pluridisciplinară, în urma afectării din sfera neurologică şi psihiatrică, fiind o problemă majoră ...
Stuporul disociativ la adultul tânăr. Provocări ale diagnosticului diferenţial şi managementului terapeutic
Stuporul disociativ este o afecţiune psihiatrică rară, inclusă în cea de-a cincea ediţie a Manualului de Diagnostic şi Statistică a Tulburărilor Mi...