A rare case of operated OHVIRA syndrome with a pseudocyst
Un caz rar operat de sindrom OHVIRA cu un pseudochist
Abstract
Obstructed hemivagina with ipsilateral renal agenesis (OHVIRA) syndrome – also known as Herlyn-Werner-Wunderlich syndrome – is a rare Müllerian anomaly. It was described first in 1992 by Wilson. Uterine anomalies can range from mild segmental abnormalities to unicornuate, bicornuate, didelphic uterus and even the absence of uterus and vagina. Among the most common renal anomalies, there are renal agenesis, renal ectopy, multicystic dysplastic kidney and renal duplication. We present the case of a 26-year-old nulligravida with OHVIRA syndrome, previously operated for rudimentary horn excision, diagnosed with vaginal pseudocyst.Keywords
OHVIRA syndromepseudocystrare uterine anomalyRezumat
Sindromul de hemivagin obstructiv cu ageneză renală ipsilaterală (OHVIRA) – cunoscut şi sub denumirea de sindrom Herlyn-Werner-Wunderlich – este o anomalie mülleriană rară. Sindromul a fost descris prima dată în anul 1992 de Wilson. Anomaliile uterine pot varia de la uşoare anomalii segmentare până la uter unicorn, bicorn, didelf şi chiar absenţa uterului şi a vaginului. Printre anomaliile renale, cele mai frecvente sunt agenezia renală, ectopia renală, rinichiul displazic multichistic şi duplicarea renală. Prezentăm un caz de nulipară de 26 de ani cu sindrom OHVIRA, operată anterior pentru excizia rudimentară a cornului, diagnosticată cu pseudochist vaginal.Cuvinte Cheie
sindrom OHVIRApseudochistanomalie uterină rarăCase report
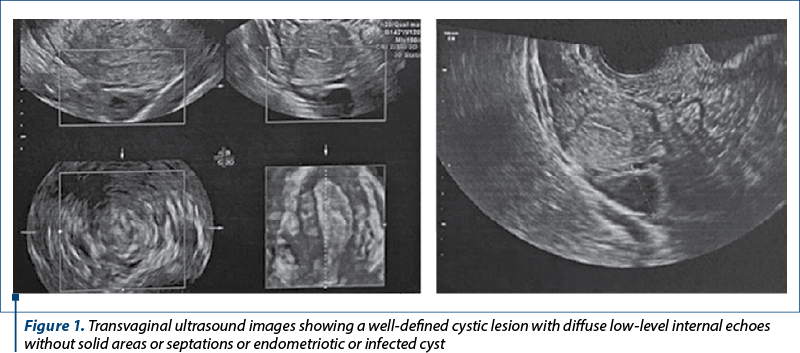
We present the case of a 26-year-old patient, nulligravida, married for a year, a known case of OHVIRA (obstructed hemivagina with ipsilateral renal agenesis) syndrome previously operated, who presented with complaints of lower abdominal pain and dysmenorrhea for the past three months, progressively increasing. Menstrual history: regular, with 5-6 days of flow every 28-30 days. She had no history of passage of clots. She was operated 12 years before, at 14 years old, as she had cyclical lower abdominal pain since menarche. She was evaluated in detail and it was found to have a non-communicating functional right uterine horn with hematocolpos, hematometra and hematosalpinx on the same side. Laparotomy and resection of the right rudimentary horn were performed. Ovaries and tubes on both sides were preserved. Post-surgery, she had regular menstrual cycles with no menstrual complaints, until 3 months before, when she started complaining of dysmenorrhea and lower abdominal pain. On examination, the patient was thin, with normal secondary sexual characteristics. Regarding breast, she was in Tanners’ stage 4, and pubic hair was normal for her age. The abdomen was soft, non-tender, and no masses were felt. On speculum examination, the cervix was not visualized, a large bulge was seen in the right fornix, and white discharge was seen per vagina. On bimanual pelvic examination, cervix felt pushed up and deviated towards the left side and felt small. At rectal examination, the fundus of the uterus was felt towards left side. The transvaginal ultrasound revealed 5-6 antral follicles in right ovary and 10-12 antral follicles in the left ovary (Figure 1). Endometrial thickness was 9.5 mm. A 6.4x4.8 cm cystic collection was seen on the right side, with homogenous appearance.
Multi-slice computed tomography (MSCT) of abdomen and pelvis (Figure 2) showed a 64x59 mm thick-walled cystic lesion/remnant of the right uterine horn filled with hemorrhagic debris, contiguous with the right side of vagina, with no definite communication. Left uterine horn measured 74x26x69 mm, without any endometrial collection. Endometrium (ET): 5.2 mm. Left side chest X ray (CX) was unremarkable. Otherwise, vagina appeared normal. Bilateral ovaries were normal. The right kidney was not seen. Left kidney: 12.2x5.1 cm. Also, spondylosis of the L5 vertebra was noticed.

A routine preoperative investigation, including 2D echography, was done, which was normal. Karyotyping revealed 46XX. CA-125 was 13.2 U/ml. The differential diagnoses considered were:
1. Remnant of the rudimentary horn that was excised previously, which formed a hematometra.
2. Müllerian cyst.
3. Gartner’s cyst.
4. Pseudocyst.
A diagnostic hysterolaparoscopy, followed by the drainage and laparoscopic excision of the cyst, was done. On hysteroscopy, the cervix was deviated to the left with large fullness on the right side of vagina.
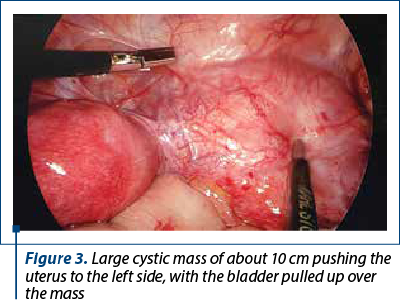
On laparoscopy, a large cystic mass about 10 cm in size was seen, pushing the uterus to the left side, with the bladder pulled up over the mass (Figure 3). Right kidney and ureter were absent. Endometriotic spots were seen on uterosacral ligaments. Bladder dissection was performed and the cyst was drained, which turned out to be a mucous filled cyst (Figure 4). Cyst wall was sent for histopathological examination (HPE).
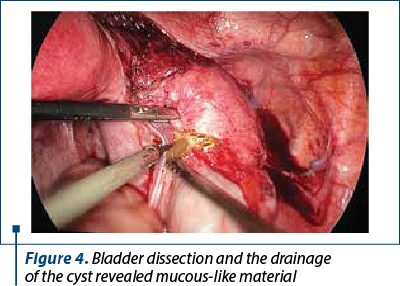
Cystoscopy revealed single left ureter. Postoperatively, the patient was stable and she was discharged the next day. She was started on leuprolide injections, 3.75 mg, once a month, for three cycles, for her endometriotic lesions, and as she was symptomatic and did not desire immediate fertility. The histopathology report revealed fibrous tissue with the possibility of a pseudocyst. The patient and her husband were advised to perform an evaluation of both partners once they seek fertility. The patient was also explained about the future risks of second-trimester abortions and the need for cerclage in pregnancy.
Discussion
The clinical presentation of Müllerian duct anomaly varies widely regarding presentations. Due to the wide variations in the spectrum of anomalies in obstructed hemivagina with ipsilateral renal agenesis (OHVIRA) syndrome, some authors even suggest renaming the term “agenesis” to “anomaly”. The most common associated disorders are renal anomalies such as renal agenesis, renal ectopy, multicystic dysplastic kidney and renal duplication(2). Rarely, an ectopic vaginal ureter may also be associated with a dysplastic kidney(3). A case was also reported with clear cell carcinoma of the cervix in OHVIRA syndrome(4). Obstetric complications seen in patients with OHVIRA syndrome are miscarriage, malpresentations, prematurity, fetal growth restriction and rupture uterus, therefore these cases require good antenatal care(5). There is also an increased risk of hypertensive disease in pregnancy, long-term implications for chronic renal and cardiovascular disease in pregnancy(6). Due to its rarity and the various presentations, the diagnosis is usually missed out, leading to management problems. It is important to have awareness regarding the risk of cancer and the anatomical variants associated with OHVIRA syndrome. A precise preoperative diagnosis helps to adopt a minimally invasive approach in the management of these cases. The excision of the obstructed hemivaginal septum and hematometra drainage are the treatment of choice in most cases of OHVIRA syndrome(7). Pregnancy has been reported in both horns with equal incidence, therefore it is advised to preserve the obstructed uterus. The patients with Müllerian anomalies only develop endometriosis if a uterus/endometrium is present(8).
Conclusions
A differential diagnosis of OHVIRA syndrome should be considered in young female patients presenting with a pelvic mass and renal anomalies. The ultrasound is operator-dependent. Magnetic resonance imaging (MRI) is the imaging modality of choice, with good diagnostic accuracy in 96% to 100% of cases. Laparoscopy is the gold standard, but it is only used when MRI fails to establish a diagnosis(9). It helps the minimally invasive management and also improves the sexual and reproductive outcomes for such patients. We should suspect other possibilities, such as pseudocysts, Müllerian cyst or Gartner’s cysts, when the patients with Müllerian anomalies present with pelvic masses.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
Haddad B, Barranger E, Paniel BJ. Blind hemivagina: long-term follow-up and reproductive performance in 42 cases. Hum Reprod Oxf Engl. 1999;14(8):1962–4.
-
Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril. 2007;87(4):918-922.
-
Sameshima H, Nagai K, Ikenoue T. Single vaginal ectopic ureter of fetal metanephric duct origin, ipsilateral kidney agenesis, and ipsilateral rudimentary uterine horn of the bicornuate uterus. Gynecol Oncol. 2005;97(1):276-8.
-
Eanase Y, Yoshida H, Naka T, Kitamura S, Natsume T, Kobayashi Kato M, Uno M, Ishikawa M, Ali Mahmoud Ali A, Kato T. Clear cell carcinoma of the cervix with OHVIRA Syndrome: a rare case report. World J Oncol. 2021;12(1):34-8.
-
Heinonen PK. Clinical implications of the didelphic uterus: long-term follow-up of 49 cases. Eur J Obstet Gynecol Reprod Biol. 2000;91(2):183–90.
-
Heinonen PK. Gestational hypertension and preeclampsia associated with unilateral renal agenesis in women with uterine malformations. Eur J Obstet Gynecol Reprod Biol. 2004;114(1):39–43.
-
Kriplani A, Dalal V, Kachhawa G, Mahey R, Yadav V, Kriplani I. Minimally invasive endoscopic approach for management of OHVIRA Syndrome. J Obstet Gynaecol India. 2019;69(4):350-5.
-
Konrad L, Dietze R, Kudipudi PK, Horné F, Meinhold-Heerlein I. Endometriosis in MRKH cases as a proof for the coelomic metaplasia hypothesis? Reproduction. 2019;158(2):R41-R47.
-
Zurawin RK, Dietrich JE, Heard MJ, Edwards CL. Didelphic uterus and obstructed hemivagina with renal agenesis: Case report and review of the literature. J Pediatr Adolesc Gynecol. 2004;17(2):137-41.



