Introduction. As the multiresistant bacteria emerge, the use of antibiotic treatment requires a clear justification, so that the benefit-risk ratio is both in favor of the individual patient and society. Materials and method. This paper represents a retrospective study that evaluated the use of antibiotics in a group of 241 newborns in the “Bucur” Maternity, Bucharest, Romania, during 2018-2020. We analyzed, using the SPSS Statistics 20 program, variables such as gestational age, birth weight, mode of delivery, Apgar score, C-reactive protein, diagnoses, antibiotics used, duration of antibiotic treatment, as well as multiple correlations between them. Results. The rate of term newborns was 52% (n=107), while premature babies represented 48% (n=100). Mean C-reactive protein was 1.117 mg/dl (first day), 0.712 mg/dl (third day) and 1.2 mg/dl (fifth day). The most frequently used antibiotics were ampicillin (n=197; 39.1%) and gentamicin (n=168; 33.3%). The longest average duration of antibiotic treatment was recorded by gentamicin (5.21 days; SD: 9.159) and ampicillin (4.92 days; SD: 8.02). The infectious pathology was present in 62 cases and included: suspected maternal-fetal infection (n=20; 6.7%), maternal-fetal infection (n=19; 6.4%), perinatal infection (n=18; 6%) and neonatal sepsis (n=5; 1.7%). The use of ampicillin or gentamicin was more frequently associated with the absence of an infectious pathology, and this fact is statistically significant. Thus, 69.49% (164 cases) of those without infections and only 12.29% (29 cases) of those with infections received ampicillin (X2=11.21; p value 2-sided=0.001). Regarding gentamicin, 54.24% (128 cases) received the antibiotic although they did not have an infectious pathology, and 15.68% (37 cases) had infectious pathology and received treatment (X2=4; p value 2-sided=0.045). Conclusions. The justification of antibiotic treatment in newborns was not always present and it was observed a tendency to overmedication in this age category with possible risks, such as adverse reactions and the selection of resistant germs, that do not always outweigh the benefits. More regulations regarding the indications of antibiotic treatment in newborns are needed in order to avoid possible risks, both at the individual and the community level.
Antibiotherapy in a tertiary neonatal care unit – use or abuse?
Antibioterapia într-o unitate neonatală terţiară – utilizare justificată sau abuz?
First published: 26 mai 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.40.2.2023.8068
Abstract
Rezumat
Introducere. În condiţiile actuale, în care ne confruntăm cu bacterii multirezistente, este de înţeles că tratamentul antibiotic necesită o justificare clară, astfel încât raportul risc-beneficiu să fie în favoarea pacientului ca individ, dar şi a societăţii ca întreg. Materiale şi metodă. Această lucrare reprezintă un studiu retrospectiv ce a inclus un grup de 241 de nou-născuţi care au primit tratament antibiotic în cadrul Maternităţii „Bucur”, Bucureşti, România. Am analizat, cu ajutorul programului SPSS Statistics 20, variabile precum vârsta gestaţională, greutatea la naştere, modalitatea de naştere, indicele Apgar, proteina C reactivă, diagnosticele, antibioticele utilizate, durata antibioterapiei, dar şi multiple corelaţii între acestea. Rezultate. Nou-născuţii la termen au reprezentat 52% (n=107), iar prematurii, 48% (n=100). Proteina C reactivă medie a fost de 1,117 mg/dl (prima zi), 0,712 mg/dl (a treia zi) şi 1,2 mg/dl (a cincea zi). Cel mai frecvent utilizate antibiotice au fost ampicilina (n=197; 39,1%) şi gentamicina (n=168; 33,3%). Durata medie de antibioterapie cea mai mare a fost înregistrată la gentamicină (5,21 zile; DS: 9,159) şi ampicilină (4,92 zile; DS: 8,02). Patologia infecţioasă a fost prezentă în 62 de cazuri şi a inclus: suspiciune de infecţie materno-fetală (n=20; 6,7%), infecţie materno-fetală (n=19; 6,4%), infecţie perinatală (n=18; 6%) şi sepsis neonatal (n=5; 1,7%). Mai frecvent, utilizarea ampicilinei sau gentamicinei a fost semnificativ statistic asociată cu absenţa unei patologii infecţioase. Astfel, 69,49% (164 de cazuri) dintre nou-născuţii fără patologie infecţioasă şi doar 12,29% (29 de cazuri) dintre
cei cu patologie infecţioasă au primit ampicilină (X2=11,21;
p value 2-sided=0,001). În ceea ce priveşte gentamicina, 54,24% (128 de cazuri) au primit antibioticul deşi nu aveau o patologie infecţioasă, iar 15,68% (37 de cazuri) aveau patologie infecţioasă şi au primit tratament (X2=4; p value 2-sided=0,045). Concluzii. Justificarea tratamentului antibiotic la nou-născuţi nu este mereu prezentă, fiind observată o tendinţă de supramedicaţie la această categorie de vârstă, cu posibile riscuri, precum reacţiile adverse şi selecţia de germeni rezistenţi, care nu depăseşc întotdeauna beneficiile. Sunt necesare mai multe reglementări cu privire la indicaţiile tratamentului antibiotic la nou-născuţi, pentru a evita posibilele riscuri, atât la nivel individual, cât şi comunitar.
Introduction
Neonatal sepsis is a major global health problem. The incidence is 2202 cases per 100,000 live newborns, with a mortality between 11% and 19%(1). In a 13-year study in 65 countries that analyzed the leading causes of death in the first month of life, sepsis and other severe infections accounted for almost half of the events in the late neonatal period (days 7-27) in 2013(2). Risk factors for high mortality in neonatal sepsis are: prematurity(3), Escherichia coli infection and positive blood cultures(4).
Materials and method
We performed a retrospective study, based on the analysis of 241 newborns files hospitalized in the “Bucur” Maternity, Bucharest, Romania, between 2018 and 2020, who received at least one antibiotic. The cases were extracted from the electronic medical records, stating that there were situations where a number of information was missing due to the fact that the patients came by transfer from other units. For data collection and statistical analysis, we used the IBM SPSS Statistics 20 program.
Variables analyzed for each newborn included: gestational age, birth weight, Apgar score, mode of delivery, C-reactive protein, antibiotics used and duration of administration, newborn diagnoses, and any recorded maternal infections. For C-reactive protein (CRP), three values were recorded, in ascending chronological order, marked time 1, time 2 and time 3, evaluated on day 1, day 3 and day 5 after antibiotic administration.
For correlations, we used the Pearson coefficient, respectively the chi-square test.
The Pearson coefficient is used to evaluate the existence of a certain correlation between two continuous variables, with the condition that they have a normal histogram distribution. The following variables and their relationship were analyzed: gestational age, birth weight, Apgar score, CRP time 1, duration in days of antibiotic treatment (all except ceftriaxone and colistin, as they do not have a normal distribution on the histogram).
The chi-square test is used to determine whether two nominal variables are dependent on each other. The following variables were analyzed: mode of delivery, antibiotics used and diagnoses.
Results
The main characteristics of the study group
The analyzed variables are: gestational age (GA), birth weight (BW), mode of delivery, APGAR score (AS), C-reactive protein, antibiotics used, duration of treatment and diagnoses. The mean GA was 36 weeks, with a standard deviation (SD) of approximately three weeks, with a minimum of 25 weeks and a maximum of 41 weeks. As categories of newborns, 51.7% (n=107) were term and 48.3% (n=100) were premature. Of these, 5.8% (n=12) were late term, 15.9% (n=33) were true term, 30% (n=62) were early term, 33.3% (n=69) were premature, 7.7% (n=16) were moderate premature, 5.3% (n=11) were severe preterm and 1.9% (n=4) were extreme preterm. The mean BW was 2688 grams, with a standard deviation of about 726 grams, with a minimum of 800 grams and a maximum of 4919 grams. Caesarean section was the mode of delivery in 53.6% of cases (n=127) and spontaneous delivery was performed in 45.6% of cases (n=110). The mean value of AS was 8.1, with a standard deviation of approximately 1.2.
Of the total of 241 neonates included in the study, dynamically measured CRP (mg/dl) could be recorded in 185 patients at time 1, in 87 patients at time 2, and in 12 patients at time 3. The mean time 1 CRP was 1.12, with a standard deviation of 1.77, with a minimum of 0.01 and a maximum of 13.65. The mean time 2 PCR was 0.71, with a standard deviation of 1.24, a minimum of 0.01 and a maximum of 7. The mean time 3 PCR was 1.2, with a standard deviation of 2.11, a minimum of 0.03 and a maximum of 7.6.
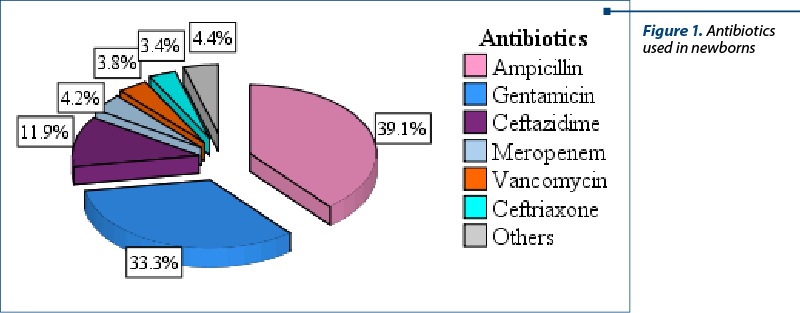
The following antibiotics were used in the study group: amikacin, ampicillin, ceftazidime, ceftriaxone, cilastatin, colistin, gentamicin, imipenem plus cilastatin, meropenem, penicillin and vancomycin. The most frequently administered were ampicillin (39.1%; n=197), gentamicin (33.3%; n=168), ceftazidime (11.9%; n=60), meropenem (4.2%; n=21), vancomycin (3.8%; n=19) and ceftriaxone (3.4%; n=17).
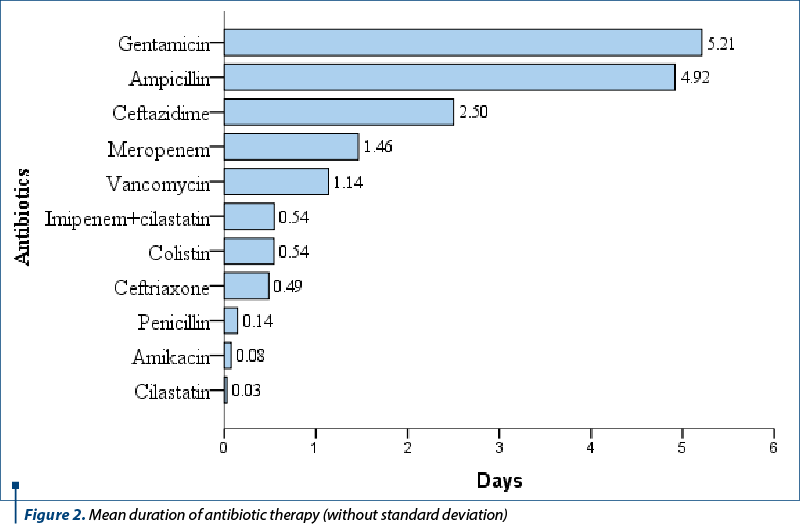
The average duration of antibiotic treatment administration is shown in Figure 2. The antibiotics with the longest treatment duration were gentamicin (5.21 days; SD: 9.159), ampicillin (4.92 days; SD: 8.02), ceftazidime (2.5 days; SD: 8.213), meropenem (1.46 days; SD: 7.795) and vancomycin (1.14 days; SD: 6.612).
The main categories of diagnoses that have been determined included: respiratory, infectious, hematological, neurological pathologies, jaundice, congenital heart defects (CHD), birth asphyxia, nuchal cord, perinatal hypoxic syndrome, congenital and chromosomal anomalies, erythema toxicum etc. The most frequent categories encountered were: hyperbilirubinemia (30%; n=82), respiratory pathology (30%; n=82), infectious pathology (16.5%; n=45), hematological pathology (7.7%; n=21) and perinatal hypoxic syndrome (5.5%; n=15).
Of the total of 241 cases, the diagnostic data could be obtained for 197 patients, and 44 had insufficient data. The most frequent diagnoses were represented by: jaundice (27.5%; n=82), newborn respiratory distress syndrome (NRDS; 19.8%; n=59), suspicion of maternal-fetal infection (6.7%; n=20), maternal-fetal infection (6.4%; n=19), perinatal infection (6%; n=18), transient tachypnea of the newborn (TTN; 6%; n=18), perinatal hypoxic syndrome (5%; n=15), anemia (3.7%; n=11) and hemorrhagic syndrome (3.4%; n=10).
Of the 83 patients with respiratory pathology, 68.6% presented newborn respiratory distress syndrome (n=59), 20.93% presented transient neonatal tachypnea (n=18), 8.14% had tachypnea (n=7) and 1.16% presented each laryngeal stridor, respectively newborn desaturation (n=1 each).
Seven patients presented with congenital heart defects, of which two cases were with atrial septal defect (ASD) and one with ventricular septal defect (VSD), patent ductus arteriosus (PDA), tricuspid atresia, complex congenital heart defects (ASD, VSD, dextrocardia, pulmonary artery stenosis and right ventricular double ejection) and unspecified CHM.
Of the total of 241 patients, 6.7% had suspected maternal-fetal infection (n=20), 6.4% had maternal-fetal infection (n=19), 6% had perinatal infection (n=18), and 1.7% had neonatal sepsis (n=5), totaling 62 cases of infectious pathology.
The five reported cases of early neonatal sepsis had as etiology E. coli in two cases and unknown in the other three. The etiology of the 18 cases of perinatal infection was represented by Staphylococcus aureus (n=2), E. coli and group B Streptococcus (n=1 each) and unknown in the remaining 14 cases. Maternal-fetal infections were reported in 18 cases and the etiology was E. coli in one patient and the remaining 17 cases had an unspecified etiology.
Other infections reported were conjunctivitis, Enterobacter digestive colonization, congenital syphilis, and hepatitis C virus infection (one case each).
Twelve diagnoses of maternal infections were also recorded, of which four cases with group B Streptococcus (GBS), three cases with E. coli, two cases with hepatitis C virus (HCV) and one case with hepatitis B virus (HBV), syphilis and Listeria, respectively.
Among the patients with hematological diagnoses, anemia occurred in 11 newborns (of which one congenital, one prematurity, and in the rest the type was not specified), 10 had hemorrhagic syndrome and five had incompatibilities in the Rh system (four cases) or ABO (one case).
Of the 82 cases of hyperbilirubinemia, 34 cases were reported as neonatal jaundice, three cases as jaundice of prematurity, one case each for physiological jaundice, moderate hyperbilirubinemia, respectively bilirubin 10 mg/dl, and in the remaining 42 cases it was not specified.
A perinatal pathology was registered in 22 newborns, of which 15 cases had perinatal hypoxic syndrome, four cases had asphyxia at birth and three cases had nuchal cord.
The reported neurological diagnoses included: tonic-clonic seizures (n=2), intracranial hemorrhage (n=1), and post-intracranial hemorrhage hydrocephalus (n=1).
Congenital or chromosomal abnormalities reported were: cheilopalatoschisis, preauricular papilloma, Down syndrome, upper limb malformations and glandular hypospadias (n=1 each).
Other diagnoses were: transfusion-transfused syndrome (n=2), small-for-gestational-age newborn, retinopathy of prematurity, difficult digestive adaptation syndrome, neonatal hypoglycemia, anaphylactic shock, spontaneously healed right pneumothorax, exposure to treponemes, newborn affected by maternal drug addiction (n=1 each). Also, six cases of erythema toxicum were reported.
Out of a total of 241 cases, prophylactic antibiotic therapy was administered to 22% of the newborns (n=53).
Correlations
The correlations were analyzed using the Pearson coefficient (r) and the chi-square test.
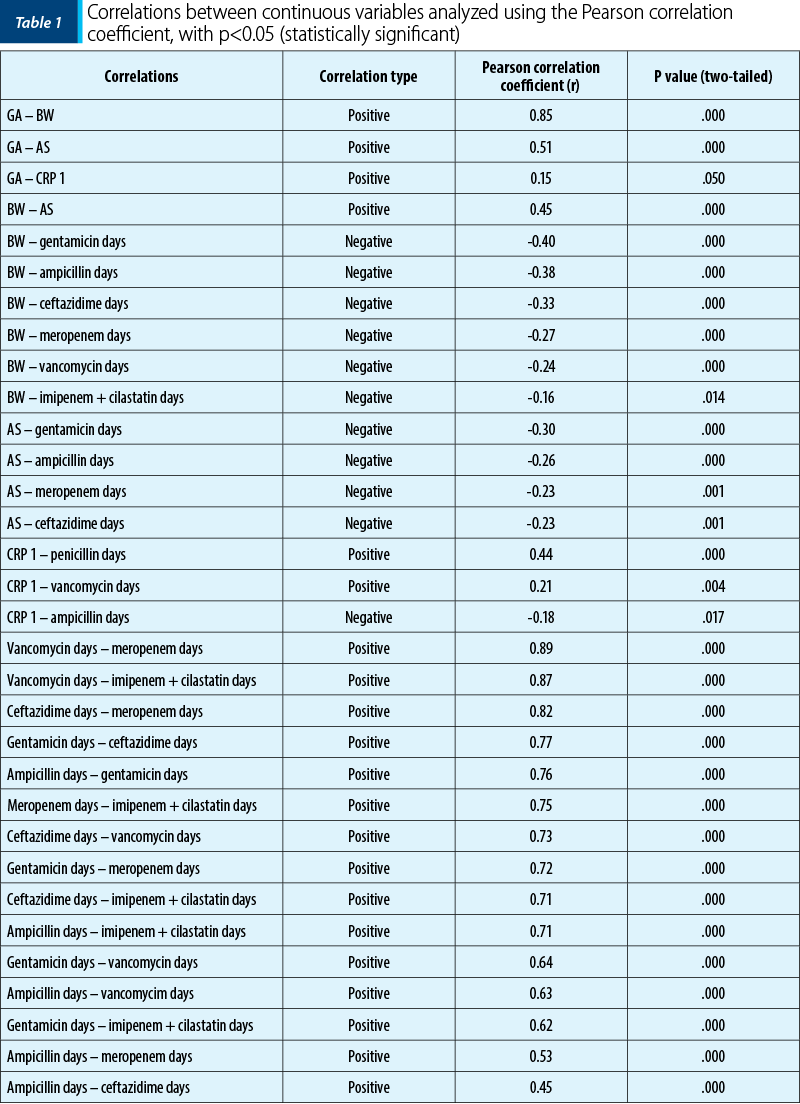
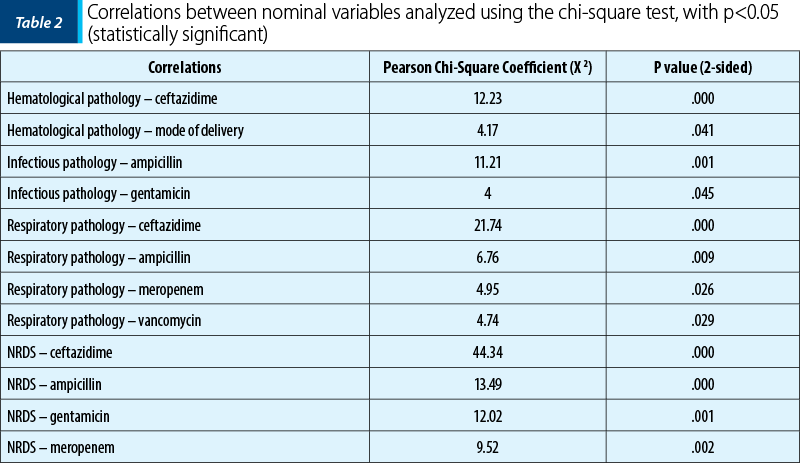
The correlations between the continuous variables, in descending order according to the Pearson coefficient, which are statistically significant (p<0.05), are presented in Table 1. For the statistically significant correlations, scatter plot graphs were made.
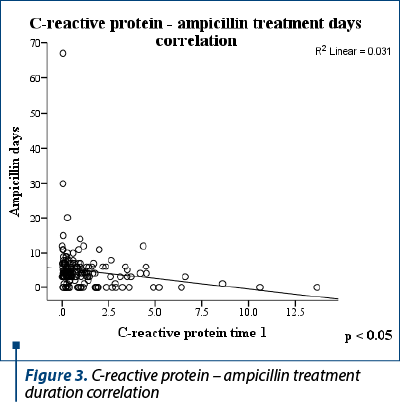
C-reactive protein at time 1 correlated positively with the duration of treatment with penicillin (r=0.44; two-tailed p value = 0.000) and vancomycin (r=0.21; two-tailed p value = 0.004), respectively negatively with ampicillin (r = -0.18; two-tailed p value = 0.017) – Figure 3.
The following correlations were analyzed using the chi-square test. The grouped column graph was used to represent the correlations. Table 2 shows the statistically significant correlations (p<0.05).
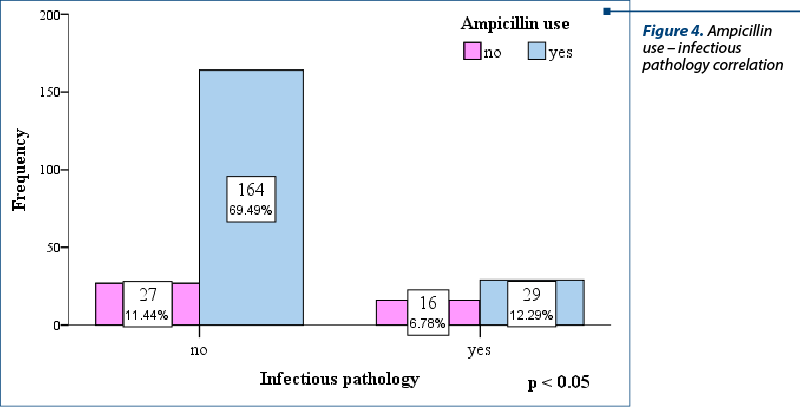
In the studied group, the use of ampicillin or gentamicin was more frequently associated with the absence of an infectious pathology, and this fact is statistically significant. Thus, 69.49% (164 cases) of those without infections and only 12.29% (29 cases) of those with infections received ampicillin (X2=11.21; p value 2-sided = 0.001) – Figure 4. Regarding gentamicin, 54.24% (128 cases) received the antibiotic although they did not have an infectious pathology, and 15.68% (37 cases) had an infectious pathology and received treatment (X2=4;
p value 2-sided = 0.045).
Discussion
In our study, the rate of term newborns was 52% (n=107), and premature babies represented 48% (n=100). The mean gestational age was 36 weeks, the mean birth weight was 2688 grams, and the mean Apgar score was 8.1. The mode of delivery was by caesarean section in 54% of cases and spontaneous birth in 48% of cases. Mean C-reactive protein was 1.117 mg/dl (first day), 0.712 mg/dl (third day) and 1.2 mg/dl (fifth day). The most frequently used antibiotics were ampicillin (n=197; 39.1%) and gentamicin (n=168; 33.3%). The longest average duration of antibiotic treatment was recorded by gentamicin (5.21 days; SD: 9.159) and ampicillin (4.92 days; SD: 8.02). The most frequent diagnoses were jaundice (n=82.27.5%) and NRDS (n=59; 19.8%). The infectious pathology included suspected maternal-fetal infection (n=20; 6.7%), maternal-fetal infection (n=19; 6.4%), perinatal infection (n=18.6%) and neonatal sepsis (n=5; 1.7%). The etiology of the perinatal infection was nonspecific in 14 cases, Staphylococcus aureus in two cases, E. coli and group B Streptococcus in one case.
In practice, the most frequently used antibiotics for the empiric treatment of neonatal sepsis are ampicillin and gentamicin. The most used cephalosporin in the USA for newborns is cefotaxime, and as alternatives, ceftazidime or cefepime. Ceftriaxone is rarely used due to the risk of hyperbilirubinemia in the newborn. Meropenem is a broad-spectrum carbapenem, without neurological adverse reactions such as seizures. Vancomycin requires monitoring of the therapeutic level, because it can cause nephrotoxicity, ototoxicity and red man syndrome, but their incidence in newborns remains unclear(5).
In a multinational randomized clinical trial that took place between 2009 and 2015, which followed-up newborns in a control group and in a test group in which the procalcitonin level was monitored, it was observed that the average duration of antibiotic treatment was shorter in the test group (55 hours – 2.29 days) versus the control group (65 hours – 2.7 days). We can observe a shorter duration of antibiotic therapy even in the control group compared to the group studied in Romania(6).
The higher the gestational age, the higher the birth weight, Apgar score and C-reactive protein at time 1 are (positive correlation). In a 2004 report, it was objectified that a CRP value above 6 mg/dL (pathological significance) was more common in neonates with higher GA(7).
Birth weight was negatively correlated with the duration of multiple antibiotics usage. A retrospective cohort study from 2019 that included neonates with a BW less than 1250 g admitted to the neonatal intensive care unit with negative blood cultures and lumbar puncture in the first two days of life demonstrated that a duration of more than five days of antibiotic therapy has been associated with increased morbidity and with the development of bronchopulmonary dysplasia(8). On the other hand, a study that included patients with GA under 30 weeks showed an inverse association of early initiation of antimicrobial treatment in the first 24 hours of life with necrotizing ulcerative enterocolitis(9). A 2021 study demonstrated an increased risk of fungal colonization of peripherally inserted central catheters (PICCs) after 15 days of antibiotic treatment(10). Also, the risk of hematogenous infection from PICC is higher as GA decreases(11).
A 2020 Swedish study of 12,623 term newborns, of which 120 developed early sepsis, demonstrated the cost-effectiveness of the decision to change the duration of antibiotic treatment based on the value of C-reactive protein and clinical symptoms, without the risk of relapse(12). Another study published in 2021 demonstrates the utility of C-reactive protein (cut off 1.6 mg/dL) and procalcitonin in the first 36 hours after starting empiric antibiotic treatment as highly accurate exclusion criteria of early neonatal sepsis(13).
In the studied group, the use of ampicillin or gentamicin was more frequently associated with the absence of an infectious pathology, and this fact is statistically significant. These aspects could be due to the fact that ampicillin and gentamicin were the most frequently used antibiotics, even though they did not always have a clear indication for administration, like positive cultures, being probably administered for prophylaxis in the maternal context.
Conclusions
Antibiotic prophylaxis was administered to 22% of newborns. Baseline C-reactive protein is correlated with the duration of penicillin and vancomycin therapy.
The following combinations of two antibiotics were frequently administered in association: ampicillin, ceftazidime, gentamicin, imipenem plus cilastatin, meropenem, vancomycin. Neonatal respiratory distress syndrome correlated positively with the administration of ceftazidime and meropenem, and correlated negatively with ampicillin and gentamicin; all the aforementioned correlations are statistically significant.
The justification of antibiotic treatment in newborns is not always present. It was observed a tendency to overmedication in this age category, with possible risks such as adverse reactions and the selection of resistant germs that do not always outweigh the benefits. More regulations regarding the indications of antibiotic treatment in newborns are needed, in order to avoid possible risks, both at the individual and community level.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, Schlapbach LJ, Reinhart K, Kissoon N. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med. 2018;6(3):223-30.
-
Oza S, Lawn JE, Hogan DR, Mathers C, Cousens SN. Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000-2013. Bull World Health Organ. 2015;93(1):9-28.
-
Cohen-Wolkowiez M, Moran C, Benjamin DK, Cotten CM, Clark RH, Benjamin DK Jr, Smith PB. Early and late onset sepsis in late preterm infants. Pediatr Infect Dis J. 2009;28(12):1052-6.
-
Stoll BJ, Hansen NI, Sánchez PJ, Faix RG, Poindexter BB, Van Meurs KP, Bizzarro MJ, Goldberg RN, Frantz ID 3rd, Hale EC, Shankaran S, Kennedy K, Carlo WA, Watterberg KL, Bell EF, Walsh MC, Schibler K, Laptook AR, Shane AL, Schrag SJ, Das A, Higgins RD. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics. 2011;127(5):817-26.
-
Mukhopadhyay S, Wade K, Puopolo K. Drugs for the Prevention and Treatment of Sepsis in the Newborn. Clin Perinatol. 2019;46(2):327-47.
-
Stocker M, van Herk W, El Helou S, Dutta S, Fontana MS, Schuerman F, et al. Procalcitonin-guided decision making for duration of antibiotic therapy in neonates with suspected early-onset sepsis: a multicentre, randomised controlled trial (NeoPIns). Lancet. 2017;390(10097):871–81.
-
Turner MA, Power S, Emmerson AJ. Gestational age and the C reactive protein response. Arch Dis Child Fetal Neonatal Ed. 2004;89(3):F272-F273.
-
Fajardo C, Alshaikh B, Harabor A. Prolonged use of antibiotics after birth is associated with increased morbidity in preterm infants with negative cultures. J Matern Fetal Neonatal Med. 2019;32(24):4060-6.
-
Berkhout D, Klaassen P, Niemarkt HJ, de Boode WP, Cossey V, van Goudoever JB, et al. Risk factors for necrotizing enterocolitis: A prospective multicenter case-control study. Neonatology. 2018;114(3):277-84.
-
Zhang L, Yang L, Dong W, Liu X, Lei X, Zhang L. Risk factors and clinical analysis of peripherally inserted central catheter-related fungal colonization in premature infants. Sci Rep. 2021;11(1): 20897.
-
Xu YP, Shang ZR, Dorazio RM, Shi LP. Risk factors for peripherally inserted central catheterization-associated bloodstream infection in neonates. Zhongguo Dang Dai Er Ke Za Zhi. 2022;24(2):141-46.
-
Gyllensvärd J, Ingemansson F, Hentz E, Studahl M, Elfvin A. C-reactive protein- and clinical symptoms-guided strategy in term neonates with early-onset sepsis reduced antibiotic use and hospital stay: a quality improvement initiative. BMC Pediatr. 2020;20(1):531.
-
Stocker M, van Herk W, El Helou S, et al. C-Reactive Protein, Procalcitonin, and white blood count to rule out neonatal early-onset sepsis within 36 hours: a secondary analysis of the Neonatal Procalcitonin Intervention Study. Clin Infect Dis. 2021;73(2):e383-e390.