Caracteristicile neonatale în malformaţiile cardiace congenitale – experienţa noastră
The neonatal characteristics of congenital heart defects – our experience
Abstract
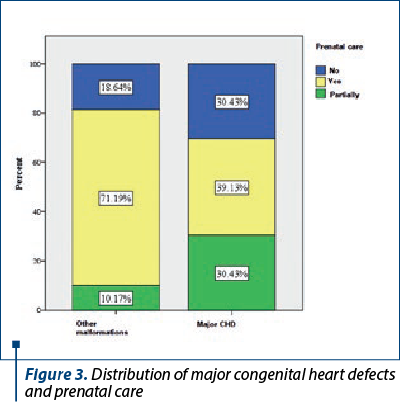
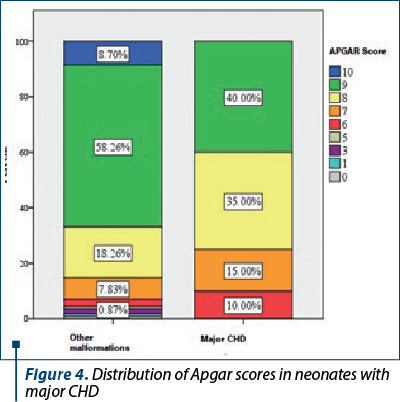
Introduction. Congenital heart defects (CHD) represent the most frequent birth defect, occurring in 1% to 5% of all live births. The purpose of our study was to reveal the neonatal characteristics of neonates with CHD from our department. Materials and method. We performed a prospective study between June 2016 and August 2021 that included newborns from the “Bucur” Maternity, Bucharest, who were diagnosed with cardiac defects. The study included 144 newborns with malformations and 70 neonates (48.6%) with CHD. The malformations were divided into minor malformations, mild cardiac malformations and major cardiac defects. Results. Minor cardiac malformations were found in 15.28% (22 cases) of the newborns with malformations, and the gender distribution was 12 boys and nine girls, respectively one child with ambiguous gender/hermaphrodite. We observed that 54.55% of them were born at term (12 children), 27.27% were late preterm (three cases), 4.55% were moderate preterm (one case) and 13.64% were extremely preterm (three cases). Within the group of newborns with malformations, the proportion of mild malformations was 17.36%, being represented by 25 newborns. Major cardiac defects were found in 15.97% (23 cases) of the newborns with malformations and the gender distribution was 11 boys (47.83%) and 12 girls (52.17%). Significantly lower Apgar scores (at 1 minute) were observed in neonates with major cardiac malformations compared with neonates with other types of malformations (U=815,000.5, Z=-2293, p=0.022). Conclusions. The variety of CHD in our clinic was from minor to severe. The environmental factors correlated with the type of CHD. The congenital heart defects were more frequent in adolescent mothers and in pregnancies with no prenatal care. The neonatal characteristics are related to the gestational age at birth and with the severity of congenital heart defects.Keywords
congenital heart defectspretermnewbornneonatesRezumat
Introducere. Malformaţiile cardiace congenitale (MCC) reprezintă cel mai frecvent defect congenital, apărând la 1% până la 5% din nou-născuţii vii. Scopul acestui studiu a fost de a dezvălui caracteristicile neonatale ale nou-născuţilor cu MCC din departamentul nostru. Materiale şi metodă. Am realizat un studiu prospectiv în perioada iunie 2016 – august 2021 care a inclus nou-născuţi de la Maternitatea „Bucur”, Bucureşti, diagnosticaţi cu defecte cardiace. Studiul a inclus 144 de nou-născuţi cu malformaţii şi 70 de nou-născuţi (48,6%) cu MCC. Malformaţiile au fost împărţite în malformaţii minore, malformaţii cardiace uşoare şi defecte cardiace majore. Rezultate. Malformaţiile cardiace minore au reprezentat 15,28% (22 de cazuri) dintre nou-născuţii cu malformaţii, iar distribuţia pe sexe a fost de 12 băieţi şi nouă fete, respectiv un copil cu sex ambiguu/hermafrodit. Am observat că 54,55% dintre ei s-au născut la termen (12 copii), 27,27% au fost prematuri tardivi (trei cazuri), 4,55% au fost prematuri moderaţi (un caz) şi 13,64% au fost prematuri extremi (trei cazuri). În cadrul lotului de nou-născuţi cu malformaţii, proporţia malformaţiilor moderate a fost de 17,36%, fiind reprezentată de 25 de nou-născuţi. Defectele cardiace majore au fost constatate la 15,97% (23 de cazuri) dintre nou-născuţii cu malformaţii, iar distribuţia pe sexe a fost de 11 băieţi (47,83%) şi 12 fete (52,17%). Scoruri Apgar semnificativ mai mici (la 1 minut) au fost observate la nou-născuţii cu malformaţii cardiace majore, în comparaţie cu nou-născuţii cu alte tipuri de malformaţii (U=815000,5, Z=-2293, p=0,022). Concluzii. Gradul de severitate al malformaţiilor cardiace în clinica noastră a fost de la minor la sever. Factorii de mediu s-au corelat cu tipul de MCC. Malformaţiile cardiace congenitale au fost mai frecvente la mame adolescente şi la sarcinile neinvestigate. Caracteristicile neonatale sunt legate de vârsta gestaţională la naştere şi de severitatea malformaţiilor cardiace congenitale.Cuvinte Cheie
malformaţii cardiace congenitaleprematurnou-născutperioadă neonatalăIntroduction
Congenital heart defects (CHD) represent the most frequent birth defect, occurring in 1% to 5% of all live births. Genetic, epigenetic and environmental factors are incriminated in a complex, multistep process of morphogenesis that is under genetic regulation. Although the genetic contribution is well recognized, the genetic causes of human are still identified infrequently(1).
The heart is unique in its dynamic development: growth is related to mechanical stimulation, and any pathogenic factor of the intrauterine environment may have a direct impact on fetal embryology(2). Advances in ultrasound, prenatal care, cardiovascular medicine and surgery have enabled most patients to reach adulthood. Unfortunately, these patients require frequent follow-ups by physicians with specific knowledge in the field of congenital heart disease(3). The purpose of our study was to reveal the neonatal characteristics of neonates with CHD from our department.
Materials and method
We performed a prospective study between June 2016 and August 2021 that included newborns from the “Bucur” Maternity, Bucharest, who were diagnosed with cardiac defects. The study included 144 newborns with malformations and 70 neonates (48.6%) with CHD. From the data obtained, we selected in the present report only the newborns who had cardiac defects.
The malformations were divided as follows: minor malformations (small atrial septal defect; ASD), minor muscular ventricular septal defect (VSD), minor pulmonary artery stenosis, isolated bicuspid aortic valve; mild cardiac malformations – congenital heart defects and malformations that do not represent a neonatal emergency were included (examples: VSD, ASD, persistent arterial ductus – with/or without existing hemodynamic impact), and major cardiac defects (complex cardiac malformation; CCM), life-threatening cardiac malformations, decompensated cardiac malformation, such as tetralogy of Fallot, severe hypoplasia of the right or left ventricles, moderate/severe aortic coarctation, severe pulmonary valve stenosis, transposition of great vessels, pulmonary artery atresia, abnormalities of pulmonary venous drainage with single collector in left atrium, double right ventricle outflow, pulmonary valve agenesis.
The data were collected using Excel program and were processed with SPSS 25 variant statistic program. A p value was considered statistically significant when p≤0.05.
Results
Minor cardiac malformations were found in 15.28% (22 cases) of the newborns with malformations, and the gender distribution was 12 boys and nine girls, respectively one child with ambiguous gender/hermaphrodite. Among them, 50% of the children with minor cardiac malformations were born by caesarean section (11 cases) and 50% vaginally (11 cases), and 90.9% of the newborns had cranial presentation (20 cases), while 9.1% had breech presentation (two cases). Neonates with minor cardiac defects ranged in weight from 1300 to 4110 grams, with a mean weight of 2712.05 grams (standard deviation: 750.369; CI: 2379.35-3044.74).
During pregnancy, the minor cardiac defect was suspected by ultrasound in two cases, representing 9% of the neonates diagnosed with minor malformations. The temporary distribution of the minor cardiac defects was as follows: 50% of the children were born in 2017 (11 cases), 18.2% were born in 2018 (four cases), 18.2% in 2019 (four cases), 4.5% in 2020 (one case), and 9.1% in 2021 (five cases) – Figure 1.
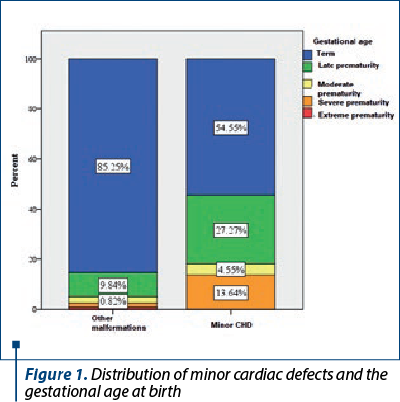
We analyzed the gestation age at birth for these neonates and we observed that 54.55% of them were born at term (12 children), 27.27% were late preterm (three cases), 4.55% were moderate preterm (one case) and 13.64% were extremely preterm (three cases).
Within the group of newborns with malformations, the proportion of mild malformations was 17.36%, being represented by 25 newborns. The gender distribution was balanced, with 12 boys and 13 girls. Most cases of mild heart malformations were found in children born at term (88% of cases; 22 children), and the other 12% of cases were found in children born with late prematurity (three cases).
Regarding the mode of delivery, 66.67% of the neonates with moderate heart malformations were born by caesarean section (16 cases), and 33.33% by vaginal way (eight cases). At birth, 87.5% of the newborns had cranial presentation (21 cases), and 12.5% had breech presentation (three cases). Neonates with mild heart malformations ranged in weight from 2000 to 3860 grams, with a mean weight of 3155.22 grams (standard deviation: 563.55; CI: 2911.53-3398.92). Among them, four cases (16%) of the 25 newborns with mild cardiac malformations had the ultrasound suspicion of malformations from pregnancy. The temporary distribution of the neonates with mild CHD was: 32% were born in 2017 (eight cases), 24% in 2018 (six cases), 36% in 2019 (nine cases), and 8% in 2021 (two cases).
Major cardiac defects
Major cardiac defects were found in 15.97% (23 cases) of the newborns with malformations and the gender distribution was 11 boys (47.83%) and 12 girls (52.17%). 52.38% of the mothers who gave birth to children with major CHD came from urban areas (12 cases), and 47.62% came from rural areas (10 cases).
Furthermore, 78.26% of the children with major cardiac malformations were born at term (18 children), 13.04% were late preterm (three cases), 4.35% were moderate preterm (one case), and 4.35% were extremely preterm (one case).
Also, 73.91% of the children with major cardiac malformations were born by caesarean section (17 cases), and 26.09% vaginally (six cases); 95.65% of the newborns had cranial presentation at birth (22 cases) and 4.35% had breech presentation (one case).
Neonates with major cardiac malformations ranged in weight from 1495 to 3850 grams, with a mean weight of 2843.41 grams (standard deviation: 672.55; CI: 2545.21-3141.6). Among them, 12 (52.17%) were identified with CHD from pregnancy. Also, 26.1% of the children with major cardiac malformations were born in 2017 (six cases), 39.1% in 2018 (nine cases), 13% in 2019 (three cases), and 21.7% in 2020 (five cases).
A number of five out of the 11 adolescent mothers (45.45%) included in the group with malformations gave birth to children with major cardiac malformations (Figure 2). Thus, among the children with major cardiac malformations, 25% were born by adolescent mothers (five cases out of 20), this situation being found in only 5.88% of the other newborns with other malformations (six of the 102 children with other malformations had an adolescent mother).

It was found that pregnancies resulting in children with major cardiac defects had no prenatal care more often than pregnancies resulting in children with other types of malformations. First, it is noted that approximately one-third of them were not followed-up at all (30.43%; seven cases), and another third were followed-up only partially (30.43%; seven cases) – Figure 3. Thus, less than 40% of these pregnancies were monitored (39.13%; nine cases). In comparison, the pregnancies of other women who gave birth to children with malformations (other than major cardiac) were followed-up in more than 70% of cases (71.19%; 84 cases) and only 18.64% were not followed-up at all (22 cases).
Significantly lower Apgar scores (at 1 minute) were observed in neonates with major cardiac malformations compared to neonates with other types of malformations (U=815,000.5, Z=-2293, p=0.022) – Figure 4.
Discussion
It was established that congenital heart disease represents abnormalities in heart structure that occur before birth. The causes for CHD were identified as the excessive alcohol consumption during pregnancy, medications, or maternal viral infection, such as Rubella virus or measles, in the first trimester of pregnancy. It was also observed that, for congenital heart disease, genes in chromosome 1 showed some defects in nucleotide sequence(4). Prematurity and low birth weight are important risk factors for increased morbidity and mortality in infants with congenital heart defects(5). The risk of adverse pregnancy outcome, including CHD, increases with the advancing maternal age. Women aged above 40 years old have an increased risk of adverse perinatal and maternal outcome, especially when pregnancy goes beyond 41 weeks and the fetus has diagnosed of undiagnosed malformations(6). Elective induction of labor at 41 weeks of gestation, and potentially earlier, also appears to be an adequate intervention with benefits for both mother and child(7).
Studies proved that, after detecting a fetal cardiac malformation, karyotyping is necessary for an accurate prenatal care. The possibility of detection of an aneuploidy is increased if some typical heart defects are associated with congenital heart defects(8). A method of detection is microarray with cytogenetic analysis to identify particularly the chromosomal abnormalities in fetuses with CHD and to conduct obstetrical outcomes(9).
The gold standard method to diagnose neonates with congenital heart defects is ultrasonography, even though there are studies that tried to prove the efficiency of other techniques, such as pulse oximetry. Pulse oximetry will detect more infants in settings with a lower prenatal diagnosis rate(10,11).
A recent report proved that prenatal diagnosis of CHD is associated with a lower birth weight, preterm delivery and with an increased risk of delivery by primary cesarean section(12). Our study revealed similar results.
Despite important advances in neonatal management, congenital heart disease remains the first cause of death in the first year of life from congenital malformations. The current methods used to approach improving outcomes in CHD are multiple and include methods such as advanced cardiac imaging in the neonate with congenital heart defects, and highlight the growing importance of quality improvement and safety programs in the cardiac intensive care unit(13). Even so, unrecognized critical CHD may result in death in the neonatal period and the diagnosis of congenital heart defects has to be made as early as possible(14). During pregnancy, abnormalities in cardiotocographic monitoring may be the result of fetal heart defect, but the ultrasonographic evaluation of the fetus and additional neonatal imagistic methods must establish the precise diagnosis(15).
Understanding the risks of early delivery of neonates with prenatally diagnosed CHD may help guide the perioperative management in neonates who are born preterm(16). When congenital heart defects are not diagnosed before birth, there should be a high degree of suspicion of critical cardiac malformations in infants presenting with shock or hypoxia(17). Clear definitions for the medical approach, including nutritional elements in the setting of medical complications and the close assessment of growth by pediatricians and specialized nutritionists, are crucial for the long-term outcome and for the quality of life of these infants(18).
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
-
Azhar M, Ware SM. Genetic and developmental basis of cardiovascular malformations. Clin Perinatol. 2016;43(1):39-53.
-
Linglart L, Bonnet D. Epigenetics and congenital heart diseases. J Cardiovasc Dev Dis. 2022;9(6):185.
-
Van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ. The changing epidemiology of congenital heart disease. Nat Rev Cardiol. 2011;8(1):50-60.
-
Sun R, Liu M, Lu L, Zheng Y, Zhang P. Congenital heart disease: causes, diagnosis, symptoms, and treatments. Cell Biochem Biophys. 2015;72(3):857-60.
-
Puia-Dumitrescu M, Sullivan LN, Tanaka D, Fisher K, Pittman R, Kumar KR, Malcolm WF, Gustafson KE, Lodge AJ, Goldberg RN, Hornik CP. Survival, morbidities, and developmental outcomes among low birth weight infants with congenital heart defects. Am J Perinatol. 2021;38(13):1366-72.
-
Kortekaas JC, Kazemier BM, Keulen JKJ, Bruinsma A, Mol BW, Vandenbussche F, Van Dillen J, De Miranda E. Risk of adverse pregnancy outcomes of late- and postterm pregnancies in advanced maternal age: A national cohort study. Acta Obstet Gynecol Scand. 2020;99(8):1022-30.
-
Caughey AB, Sundaram V, Kaimal AJ, Cheng YW, Gienger A, Little SE, Lee JF, Wong L, Shaffer BL, Tran SH, Padula A, McDonald KM, Long EF, Owens DK, Bravata DM. Maternal and neonatal outcomes of elective induction of labor. Evid Rep Technol Assess (Full Rep). 2009;(176):1-257.
-
Chaoui R, Körner H, Bommer C, Göldner B, Bierlich A, Bollmann R. Pränatale Diagnostik von Herzfehlern und assoziierte chromosomale Aberrationen [Prenatal diagnosis of heart defects and associated chromosomal aberrations]. Ultraschall Med. 1999;20(5):177-84. German.
-
Cai M, Huang H, Su L, Lin N, Wu X, Xie X, An G, Li Y, Lin Y, Xu L. Fetal congenital heart disease: Associated anomalies, identification of genetic anomalies by single-nucleotide polymorphism array analysis, and postnatal outcome. Medicine (Baltimore). 2018;97(50):e13617.
-
Johnson LC, Lieberman E, O’Leary E, Geggel RL. Prenatal and newborn screening for critical congenital heart disease: findings from a nursery. Pediatrics. 2014;134(5):916-22.
-
Majani N, Chillo P, Slieker MG, Sharau G, Mlawi V, Mongella S, Nkya D, Khuboja S, Kwesigabo G, Kamuhabwa A, Janabi M, Grobbee D. Newborn screening for critical congenital heart disease in a low-resource setting; research protocol and preliminary results of the Tanzania pulse oximetry study. Glob Heart. 2022;17(1):32.
-
Ge CJ, Mahle AC, Burd I, Jelin EB, Sekar P, Jelin AC. Fetal CHD and perinatal outcomes. Cardiol Young. 2020;30(5):686-91.
-
Martin GR, Cross RR, Hom LA, Klugman D. Updates in congenital heart disease: can outcomes improve? Am J Perinatol. 2019;36(S 02):S22-S28.
-
Krishna MR, Kumar RK. Diagnosis and management of critical congenital heart diseases in the newborn. Indian J Pediatr. 2020;87(5):365-71.
-
Feduniw S, Muzyka-Placzyńska K, Kajdy A, Wrona M, Sys D, Szymkiewicz-Dangel J. Intrapartum cardiotocography in pregnancies with and without fetal CHD. J Perinat Med. 2022;50(7):961-9.
-
Reddy RK, McVadon DH, Zyblewski SC, Rajab TK, Diego E, Southgate WM, Fogg KL, Costello JM. Prematurity and congenital heart disease: a contemporary review. Neoreviews. 2022;23(7):e472-e485.
-
Singh Y, Lakshminrusimha S. Perinatal cardiovascular physiology and recognition of critical congenital heart defects. Clin Perinatol. 2021;48(3):573-94.
-
Tsintoni A, Dimitriou G, Karatza AA. Nutrition of neonates with congenital heart disease: existing evidence, conflicts and concerns. J Matern Fetal Neonatal Med. 2020;33(14):2487-92.





