Localizare atipică a unui lipom
Unusual location of a lipoma
Abstract
Introduction
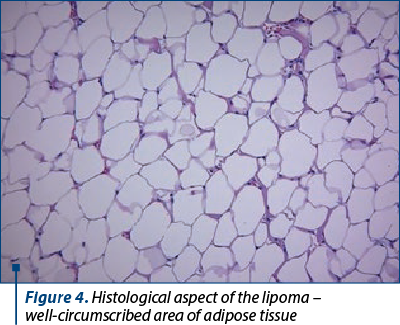
Lipoma is defined as a benign tumor of soft tissue, and the diagnosis is confirmed by the histopathological exam which describes a well-circumscribed collection of mature adipose tissue(1,2). Lipoma is the most common mesenchymal tumor and usually has a thin fibrous capsule(3). Generally, it is localized on the upper back, neck or extremities(4).
Vulvar lipomas are extremely rare; therefore, a small number of cases is reported in world literature(3,5,6). Even though the pathology can be diagnosed at any age, it is more commonly seen at 40-60 years old(3,7). Its etiology is still unclear, but trauma and gene rearrangement may play a role in its development(1,4,8).
Clinically, most lipomas measure few centimeters, but vulvar ones may reach very large sizes(3). At the examination, vulvar lipoma is detected like an oval-shaped mass, non-painful. It requires a differential diagnosis with Bartholin gland cyst, mucus cyst, epidermal cyst, inguinal hernia, fibroma or hemangioma, as well as several other benign and malignant neoplastic conditions(1,5,9). It is unusual for a lipoma to turn into malignancy(3).
Regarding the imagine exam, vulvar lipomas are described by ultrasonography as whorl-shaped, lobular structures with no vascularization on color and power Doppler imaging(10,11). A case report of vulvar lipoma showed that an encapsulated homogenous echogenic mass on ultrasound examination represents a diagnostic criterion(1,11). For an accurate diagnosis, a CT scan or an MRI is useful in evaluating the anatomical extensions of lipomas(7,12-14).
The management of lipomas can be conservative, including injection of pharmaceutical agents or laser which has good results in small and asymptomatic ones(1,15). In case of large lipomas, which may cause discomfort, psychological and social problems, the surgical excision is the preferred option(1,15). Although there are multiple methods for the management of lipomas, the surgical one is the treatment of choice, and it includes the complete removal of the capsule to prevent recurrence(1).
Case presentation
A 25-year-old female presented first in July 2021 in our clinic with vulvar discomfort that had started at the beginning of the year.
From the anamnesis, we found out that the symptoms had started insidiously, about two months before.
The examination revealed a singular growth of approximately 8/4 cm (Figure 1), with clinical characteristics of a benign tumor. The patient was presented with the option of admission in order to perform additional imaging investigations but, due to the current pandemic situation, this course of action was delayed by one year, during which the lesion grew to approximately 13/4 cm (Figure 2).
The only change in the patient’s lifestyle during this period was undergoing sessions of intense pulsed light for hair removal.
Eventually, the patient was admitted to the Department of Obstetrics-Gynecology of the University Emergency Hospital Bucharest. We noted a stable hemodynamically and respiratory patient, afebrile, 120/70 mmHg, pulse rate 74 bpm, rhythmic, temporally-spatially oriented, cooperating, the intestinal transit being present, with spontaneous urination, weight about 52 kg, without any other physical pathological characteristics noted, other than the growth described above.
No abnormal lab results were identified, not even elevated serum levels of triglycerides or hypercholesterolemia.
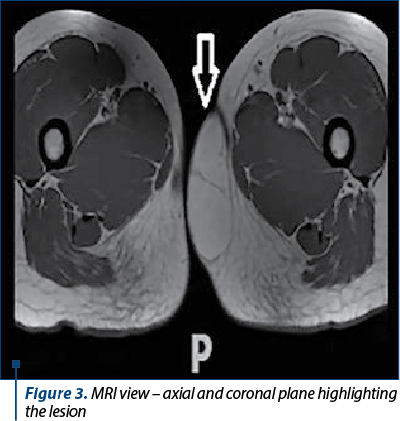
An MRI examination was performed which revealed a lobed-tumor at the level of the left labia, well delimited, with local deformation and minimal mass effect on the surrounding tissues, without pelvic or inguinal modified lymph nodes (Figure 3).
Furthermore, a tumorectomy was performed which confirmed the lipoma (Figure 4). The postoperative evolution was good, with no surgical complications.
Discussion
This case presents a rare location of a singular lipoma. The most well-known locations of the lipomas include areas such as the neck, upper back or proximal extremities(4). Vulva represents a rare site for lipoma development(1).
The etiology and pathogenesis of lipomas are still undetermined, but trauma, obesity and gene rearrangement have been cited as risk factors(1,4,8). In our case, we could not link the etiology of the vulvar lipoma to none of the known risk factors. Our patient has not had any trauma recently and she was not obese. The only change in our patient’s lifestyle was that she underwent sessions of intense pulsed light for hair removal in the last year, under which the lipoma increased. We cannot claim this procedure was the reason for the increasing lipoma, but we can neither exclude it.
Regarding the age frequency of the vulvar lipomas, it has been reported to be more common between the fourth and sixth decades of life(3,7), but our patient was only 25 years old, and this means another rare characteristic for the case.
The diagnosis of lipoma can be established through clinical examination, and it is described as a soft, mobile mass which is not adherent to the overlying skin(1). It is also painless, but it creates discomfort(1). In the current case, the tumor had all the specific features for a lipoma. Additional exams can be performed for an accurate diagnosis, such as an MRI examination which is the gold standard exam for soft tissue examination. In case of lipomas, MRI usually shows high signal in weighted images(1,15). For our patient, the presumptive diagnosis was established by clinical examination and MRI, and the certain one was confirmed by the histopathologic result. The imagining exams are useful in differentiating lipomas from liposarcomas(7,12-14).
Even though there are multiple options for the management of lipomas, the surgical excision represents the recommended one because it prevents the recurrence(1,15). In our case, we chose the surgical intervention with the complete removal of the capsule and the histopathological examination.
Conclusions
Vulvar lipoma represents a rare location for this type of tumors. Even though they are benign, they need histopathological examination and additional image exams, such as ultrasonography or MRI, to exclude a liposarcoma. The treatment of choice is the surgery excision to prevent recurrences.
Conflicts of interests: The authors declare no conflict of interests.
Keywords
germinalvulvartumorlipomaRezumat
Vulva reprezintă o localizare atipică pentru dezvoltarea unui lipom. Etiologia lipomului rămâne necunoscută, însă factori multipli au fost încriminaţi, precum obezitatea sau trauma. De asemenea, lipomul apare cel mai frecvent între 40 şi 60 de ani. În această lucrare, este prezentat cazul unei paciente de 25 de ani, fără factori de risc cunoscuţi, care a dezvoltat un lipom vulvar. S-a practicat excizia chirurgicală a tumorii, acesta fiind tratamentul preferat pentru evitarea recurenţei. Examenul histopatologic a confirmat diagnosticul de lipom vulvar.Cuvinte Cheie
germinalvulvartumorălipomIntroduction
Lipoma is defined as a benign tumor of soft tissue, and the diagnosis is confirmed by the histopathological exam which describes a well-circumscribed collection of mature adipose tissue(1,2). Lipoma is the most common mesenchymal tumor and usually has a thin fibrous capsule(3). Generally, it is localized on the upper back, neck or extremities(4).
Vulvar lipomas are extremely rare; therefore, a small number of cases is reported in world literature(3,5,6). Even though the pathology can be diagnosed at any age, it is more commonly seen at 40-60 years old(3,7). Its etiology is still unclear, but trauma and gene rearrangement may play a role in its development(1,4,8).
Clinically, most lipomas measure few centimeters, but vulvar ones may reach very large sizes(3). At the examination, vulvar lipoma is detected like an oval-shaped mass, non-painful. It requires a differential diagnosis with Bartholin gland cyst, mucus cyst, epidermal cyst, inguinal hernia, fibroma or hemangioma, as well as several other benign and malignant neoplastic conditions(1,5,9). It is unusual for a lipoma to turn into malignancy(3).
Regarding the imagine exam, vulvar lipomas are described by ultrasonography as whorl-shaped, lobular structures with no vascularization on color and power Doppler imaging(10,11). A case report of vulvar lipoma showed that an encapsulated homogenous echogenic mass on ultrasound examination represents a diagnostic criterion(1,11). For an accurate diagnosis, a CT scan or an MRI is useful in evaluating the anatomical extensions of lipomas(7,12-14).
The management of lipomas can be conservative, including injection of pharmaceutical agents or laser which has good results in small and asymptomatic ones(1,15). In case of large lipomas, which may cause discomfort, psychological and social problems, the surgical excision is the preferred option(1,15). Although there are multiple methods for the management of lipomas, the surgical one is the treatment of choice, and it includes the complete removal of the capsule to prevent recurrence(1).
Case presentation
A 25-year-old female presented first in July 2021 in our clinic with vulvar discomfort that had started at the beginning of the year.
From the anamnesis, we found out that the symptoms had started insidiously, about two months before.
The examination revealed a singular growth of approximately 8/4 cm (Figure 1), with clinical characteristics of a benign tumor. The patient was presented with the option of admission in order to perform additional imaging investigations but, due to the current pandemic situation, this course of action was delayed by one year, during which the lesion grew to approximately 13/4 cm (Figure 2).


The only change in the patient’s lifestyle during this period was undergoing sessions of intense pulsed light for hair removal.
Eventually, the patient was admitted to the Department of Obstetrics-Gynecology of the University Emergency Hospital Bucharest. We noted a stable hemodynamically and respiratory patient, afebrile, 120/70 mmHg, pulse rate 74 bpm, rhythmic, temporally-spatially oriented, cooperating, the intestinal transit being present, with spontaneous urination, weight about 52 kg, without any other physical pathological characteristics noted, other than the growth described above.
No abnormal lab results were identified, not even elevated serum levels of triglycerides or hypercholesterolemia.
An MRI examination was performed which revealed a lobed-tumor at the level of the left labia, well delimited, with local deformation and minimal mass effect on the surrounding tissues, without pelvic or inguinal modified lymph nodes (Figure 3).
Furthermore, a tumorectomy was performed which confirmed the lipoma (Figure 4). The postoperative evolution was good, with no surgical complications.
Discussion
This case presents a rare location of a singular lipoma. The most well-known locations of the lipomas include areas such as the neck, upper back or proximal extremities(4). Vulva represents a rare site for lipoma development(1).
The etiology and pathogenesis of lipomas are still undetermined, but trauma, obesity and gene rearrangement have been cited as risk factors(1,4,8). In our case, we could not link the etiology of the vulvar lipoma to none of the known risk factors. Our patient has not had any trauma recently and she was not obese. The only change in our patient’s lifestyle was that she underwent sessions of intense pulsed light for hair removal in the last year, under which the lipoma increased. We cannot claim this procedure was the reason for the increasing lipoma, but we can neither exclude it.
Regarding the age frequency of the vulvar lipomas, it has been reported to be more common between the fourth and sixth decades of life(3,7), but our patient was only 25 years old, and this means another rare characteristic for the case.
The diagnosis of lipoma can be established through clinical examination, and it is described as a soft, mobile mass which is not adherent to the overlying skin(1). It is also painless, but it creates discomfort(1). In the current case, the tumor had all the specific features for a lipoma. Additional exams can be performed for an accurate diagnosis, such as an MRI examination which is the gold standard exam for soft tissue examination. In case of lipomas, MRI usually shows high signal in weighted images(1,15). For our patient, the presumptive diagnosis was established by clinical examination and MRI, and the certain one was confirmed by the histopathologic result. The imagining exams are useful in differentiating lipomas from liposarcomas(7,12-14).
Even though there are multiple options for the management of lipomas, the surgical excision represents the recommended one because it prevents the recurrence(1,15). In our case, we chose the surgical intervention with the complete removal of the capsule and the histopathological examination.
Conclusions
Vulvar lipoma represents a rare location for this type of tumors. Even though they are benign, they need histopathological examination and additional image exams, such as ultrasonography or MRI, to exclude a liposarcoma. The treatment of choice is the surgery excision to prevent recurrences.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
-
Reda A, Gomaa I. Vulvar lipoma: a case report. Reva Bras Ginecol Obstet. 2018;40(10):647-9.
-
Morgan MB. Benign mesenchymal tumors. In: Morgan MB, Hamill JR Jr, Spencer JM. (eds.). Atlas of Mohs and Frozen Section Cutaneous Pathology. New York, NY: Springer; 2010:153-61.
-
Sukgen G. A case report: the third-largest case in the literature of a vulvar lipoma. Gynecol Minim Invasive Ther. 2020;9(4):234-6.
-
Bianchini L, Birtwisle L, Saâda E, et al. Identification of PPAP2B as a novel recurrent translocation partner gene of HMGA2 in lipomas. Genes Chromosomes Cancer. 2013;52(06):580-90.
-
Dekonda N, Korumilli RK, Wattamwar AA, Vasant D, Chandran PU. Vulvar lipoma – a case series. IOSR-JDMS. 2019;18(9):14-6.
-
Khreisat B, Uraiqat A. Vulvar lipoma:a case report. J Royal Med Serv. 2012;19(2):79-81.
-
Lee JH, Chung SM. Large vulvar lipoma in an adolescent: a case report. J Korean Med Sci. 2008;23(4):744-6.
-
Coban YK, Uzel M, Gumus N. Lipoma due to chronic intermittent compression as an occupational disease. Ann Plast Surg. 2006;57(3):275-8.
-
Heller DS. Benign tumors and tumor-like lesions of the vulva. Clin Obstet Gynecol. 2015;58(03):526-535.
-
Cheung VY. Ultrasonography of benign vulvar lesions. Ultrasonography. 2018;37(4):355-60.
-
Sherer DM, Gorelick C, Wagreich A, Lee YC, Serur E, Zigalo A, Abulafia O. Sonographic findings of a large vulvar lipoma. Ultrasound Obstet Gynecol. 2007;30(5):786-7.
-
Odoi AT, Owusu-Bempah A, Dassah ET, Darkey DE, Quayson SE. Case reports vulvar lipoma: is it so rare?. Ghana Med J. 2011;45(3):125-7.
-
Kehagias DT, Smyrniotis VE, Karvounis EE, Gouliamos AD, Creatsas G. Large lipoma of the vulva. Eur J Obstet Gynecol Reprod Biol. 1999;84(1):5-6.
-
Oh JT, Choi SH, Ahn SG, Kim MJ, Yang WI, Han SJ. Vulvar lipomas in children: an analysis of 7 cases. J Pediatr Surg. 2009;44(10):1920-3.
-
Boyer M, Monette S, Nguyen A, Zipp T, Aughenbaugh WD, Nimunkar AJ. A review of techniques and procedures for lipoma treatment. Clin Dermatol. 2015;3:105-12.




