Complicaţii materne şi neonatale în sarcina gemelară obţinută spontan versus sarcina gemelară obţinută prin FIV
Maternal and neonatal complications in spontaneous twin pregnancy versus IVF twin pregnancy
Abstract
Introduction. The aim of this study was to identify the maternal and neonatal complications in the twin pregnancy obtained spontaneously versus the twin pregnancy obtained through the assisted reproduction techniques (IVF). The study included 40 patients with twin pregnancy, respectively 80 newborns, who were diagnosed and treated at the “Elias” University Emergency Hospital, Bucharest. Results. The incidence of the twin pregnancy obtained through IVF was identified at the 36-40 years old group. 47.5% of the patients who obtained the pregnancy through IVF presented complications, compared to 22.5% of the patients with pregnancy obtained spontaneously who developed complications. The results showed that the highest incidence of complications was in the group of patients who obtained the pregnancy through IVF. As far as the newborns are concerned, 8.75% of the IVF ones developed breathing complications and 3.75% developed other complications which required admission in the Neonatal Intensive Care Unit (NICU), without significant differences between twin I and twin II. Conclusions. The neonatal and twin pregnant woman management should include the awareness of the problems that may appear more frequently in this pregnancy category, respectively the newborns.Keywords
twin pregnancymaternal complicationsIVFneonatal complicationsRezumat
Introducere. Acest studiu a avut ca obiectiv identificarea complicaţiilor materne şi neonatale din sarcina gemelară obţinută spontan, comparativ cu sarcina gemelară obţinută prin tehnici de reproducere asistată (FIV). Am analizat 40 de paciente cu sarcină gemelară, respectiv 80 de nou-născuţi, care au fost diagnosticaţi şi trataţi la Spitalul Universitar de Urgenţă „Elias”, Bucureşti. Rezultate. O incidentă crescută a sarcinii gemelare obţinută prin FIV a fost identificată la pacientele din grupa de vârstă 36-40 de ani. 47,5% dintre pacientele care au obţinut sarcina prin FIV au prezentat complicaţii, faţă de 22,5% dintre pacientele care au obţinut sarcina spontan şi au dezvoltat, la rândul lor, complicaţii. Rezultatele au arătat că incidenţa mai mare a complicaţiilor a fost la grupa de paciente care au obţinut sarcina prin FIV. În ceea ce priveşte nou-născuţii, 8,75% dintre cei obţinuţi prin FIV au dezvoltat complicaţii respiratorii şi 3,75% au dezvoltat alte complicaţii, necesitând internare în secţia de terapie intensivă neonatală, neexistând diferenţe semnificative între geamănul I şi geamănul II. Concluzii. Managementul neonatal şi al gravidei cu sarcină gemelară ar trebui să includă conştientizarea problemelor care pot să apară mai frecvent la această categorie de sarcină, respectiv la nou-născuţi.Cuvinte Cheie
complicaţii maternecomplicaţii neonatalesarcină gemelarăFIVIntroduction
This study was carried out in order to determine the maternal and neonatal complications related to twin pregnancy.
Twin pregnancy is a high-risk pregnancy, as it is associated with a significant increase in the perinatal and maternal mortality and morbidity. Although twin pregnancies are usually welcome, the excitement of a twin pregnancy can often be overshadowed by unforeseen complications.
The obstetric complications include preterm labor, anemia, pregnancy-induced hypertension, postpartum hemorrhage, prematurity, and low birth weight(1). The risk of stillbirth is higher in twin pregnancies than in singleton pregnancies(2).
Twin pregnancy is known to have more obstetrical and neonatal complications, compared to singleton pregnancy(1).
In vitro fertilization (IVF) refers to a procedure designed to overcome infertility and produce a pregnancy as a direct result of the intervention. The first pregnancy after the fertilization of a human egg in vitro and the first birth from an in vitro fertilized embryo were reported in 1976 and 1978(3).
A consequence of assisted reproductive technology has been the progressive rise in the incidence of twin pregnancies. The study of twin or multiple births is important due to the increased health risks for both mothers and babies, and accompanying a higher healthcare cost(4).
Prematurity, low birth weight (LBW), birth asphyxia, birth trauma, intrauterine fetal death and congenital malformations are important factors to explain the reasons of high perinatal mortality.
Materials and method
This is a prospective observational study carried out between January 2019 and December 2020 at the “Elias” University Emergency Hospital, Bucharest. The study included 40 women with twin pregnancy, respectively 80 newborns, out of whom 72 dichorionic twins and 8 monochorionic twins, who did not present congenital anomalies or other severe complications that would lead to neonatal death. Also, none of the patients included in the study presented complications such as: heart diseases, lung diseases, gastrointestinal diseases, kidney diseases, autoimmune disorders, psychiatric diseases or endocrine diseases before the birth, and the delivery was made by caesarean section or without labor. In the twin pregnancy, chorionicity was determined precociously by ultrasound, as of during the pregnancy and confirmed by the placental pathology after the birth.
Study inclusion or exclusion criteria
Criteria for the inclusion in the study: pregnant women with naturally or IVF obtained twin pregnancy who presented complications (pregnancy-induced hypertension, diabetes mellitus, anemia, postpartum hemorrhage and premature membranes rupture) and newborns from twin pregnancy with gestational age above 26 weeks, birth weight higher than 600 g, who presented age-specific complications.
Criteria for exclusion of the study: fetal death, multiple pregnancy, twin pregnancy reduced to sole pregnancy, triplets pregnancy reduced to twin pregnancy.
Study variables
Twin pregnancies were diagnosed at the clinical examinations of the pregnant women at the moment when they appeared at the hospital to give birth through caesarean section or natural birth. These were classified into two categories: IVF pregnancy and spontaneously obtained pregnancy. The information referring to the mothers was taken from the clinical obsevation sheet and registered in a questionnaire designed for the study, and referred to the following: maternal age, parity, pregnancy complications (hypertension, gestational diabetes mellitus, premature birth, premature membranes rupture). Also, data about the birth mode were introduced, respectively vaginal or caesarean section birth. The data about the twins were the following: birth weight, Apgar score, respiratory distress syndrome, congenital anomalies, admission of the newborns in the NICU. The neonatal outcome in the form of birth weight, Apgar score, maturity and NICU admission has been recorded for both the first twin and the second twin.
Gestation age of the twin newborns resulted from assisted reproduction techniques pregnancies was calculated from day zero, the day of the embryo transfer. The gestation age in the twin pregnancy obtained spontaneously was calculated with Naegele’s rule (LMP + 7 days – 3 months + 1 year) and by ultrasound.
Preterm is defined as babies born alive before 37 weeks of pregnancy are completed. There are subcategories of preterm birth, based on gestational age: extremely preterm (less than 28 weeks), very preterm (28 to 32 weeks), moderate to late preterm (32 to 37 weeks)(5).
Birth weight classification: extremely low birth weight (≤999 g); very low birth weight (1000 to 1499 g), low birth weight (1500 to 2499 g), and normal birth weight (≥2500 g)(6).
The Apgar score was classified as low (0-3), moderately abnormal (4-6), and reassuring (7-10)(7).
All the twin newborns were evaluated by the neonatologist through the hospital admission (from birth until discharge).
Pregnancy-induced hypertension is a blood pressure higher than 140/90 mmHg measured twice at a 4-6 hours distance after 20 gestation weeks and without proteinuria(8).
Gestation diabetes mellitus was defined as plasma blood sugar in food intake pause ≥126 mg/dl or as plasma blood sugar every two hours ≥200 mg/dl(9).
The concentration of hemoglobin below 11 mg/dl in the vein blood defined anemia during pregnancy. Postpartum hemorrhage was defined as the loss of more than 500 g of blood from the genital tract for a period ranging between 24 hours and 12 days after birth(10).
The respiratory distress syndrome was decided based on a characteristic pulmonary radiography and the need for O2≥24 hours in the newborns who presented tachypnea, nasal flaring, intercostal and subcostal retraction, expiratory moan, and cyanosis(11).
Ethical considerations
The written informed consent of the patients in the study was obtained at the admission into the clinic, the patients being assured that the information would be confidential and used only for research purposes.
Results
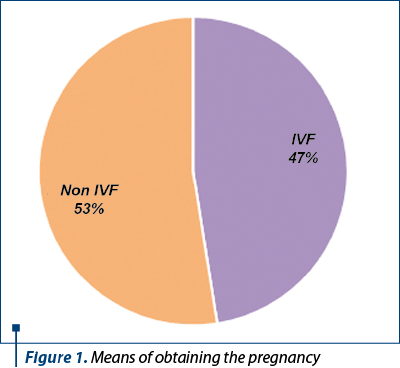
In this study, we performed an analysis on 40 patients who were diagnosed with twin pregnancy, respectively 80 newborns in whom we evaluated the complications occurred during the pregnancy and postnatal. 47% of the patients included in the study obtained the pregnancy through assisted reproduction techniques (IVF) and 53% of the patients obtained the pregnancy spontaneously, as presented in Figure 1.
The maximum incidence of the IVF twin pregnancy was recorded in the patients in the 36-40 years old group, whereas the maximum incidence in the spontaneously obtained pregnancy was for the 26-30 years old age group.
47.5% of the patients who obtained the pregnancy through IVF presented complications, namely 12.5% developed HBP, 5% developed DM, 15% anemia, 12.5% postnatal hemorrhage, and 36.3% developed premature membranes rupture.
52.5% of the patients obtained the pregnancy spontaneously, but a part of them also developed complications during the pregnancy. 2.5% of the patients developed diabetes mellitus, 7.5% developed postnatal hemorrhage and approximately 12.5% experienced premature membranes rupture. The complications occurred during the pregnancy and postnatally are presented in Figure 2.
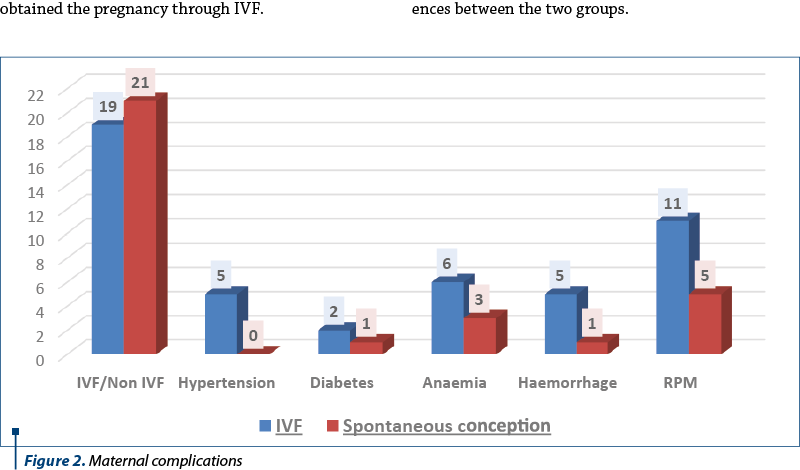
The results also showed that the highest incidence of the complications was in the group of patients who obtained the pregnancy through IVF.
The incidence of maternal complication (such as pregnancy-induced hypertension, gestational diabetes mellitus, anemia, premature rupture of membranes and severe postpartum hemorrhage) in the two groups was not significantly different.
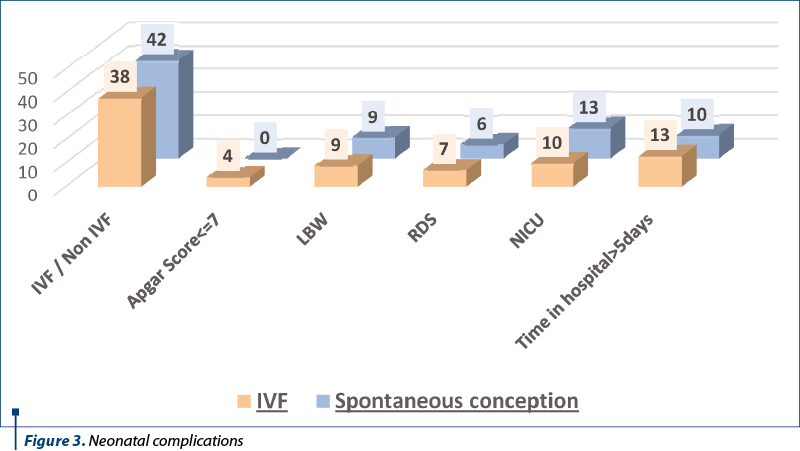
As far as the newborns resulted from twin pregnancy are concerned, 47.5% came from IVF pregnancies and 52.5% came from spontaneously obtained pregnancies. 8.75% of the IVF newborns developed respiratory complications, 3.75% presented other complications, requiring admission in the neonatal intensive care unit for monitoring and treatment, and 16.25% required ≥5 days of hospitalization. Among these, 5% had an Apgar Score ≤7. Regarding birth weight, 11.25% were LBW. The average of the gestation age in the newborns resulted from IVF pregnancy was 35 weeks, whereas for the spontaneously obtained newborns, it was 37 weeks.
The complications identified in the twin pregnancy newborns are presented in Figure 3. The differences between the complications occurred in twin I compared to twin II were not significant.
Discussion
This study aimed at a comparison between the complications occurred in twin newborns resulted from spontaneously obtained pregnancies versus assisted reproduction techniques twins, respectively the maternal complications occurred throughout the gestation period.
Maternal complications such as pregnancy-induced hypertension, diabetes mellitus or the premature rupture of membranes were more frequent in pregnancies obtained through IVF compared to the spontaneously obtained pregnancies. Instead, as far as other complications are concerned, there were no significant differences between the two groups.
The results referring to the newborns showed that there is an association between the ones obtained spontaneously or by IVF and the complications occurred in twin I and twin II which led to their admission in the neonatal intensive care unit.
There was no association between the mode of delivery and the fetal outcome in the form of Apgar score at 5 minutes, NICU admission and perinatal mortality.
Overall, our study indicates that some antenatal complications are more frequent in assisted-conception twin pregnancies than in spontaneous twin pregnancies, but their prevalence is low and, thus, their impact on the morbidity and mortality of an individual assisted-conception twin pregnancy is limited.
Close antenatal and perinatal assessment and care must be given to mothers of twin pregnancies in order to reduce the maternal and fetal complications.
A 2016 study reported that multiple pregnancies after assisted reproductive techniques are the single most likely explanation for the increased rate of gestational hypertension and preeclampsia in mothers who had undergone assisted reproductive treatment(12).
The study performed on the twin pregnancy patients confirmed the presence of the complications occurred both during the pregnancy and in the newborns, due to the infertility treatment and the use of the assisted human reproduction techniques. The caesarean section was the predominant choice of the patients with twin pregnancy included in this study.
Conclusions
It is well known that twin pregnancy is associated with a higher maternal and fetal risk.
The neonatal and twin pregnant woman management should include the awareness of the problems that may appear more frequently in this pregnancy category, respectively the newborns.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Obiechina NJ, Okolie VE, Eleje GU, Okechukwu ZC, Anemeje OA. Twin versus singleton pregnancies: The incidence, pregnancy complications, and obstetric outcomes in a Nigerian tertiary hospital. Int J Womens Health. 2011;3(1):227–30.
- Cheong-See F, et al. Prospective risk of stillbirth and neonatal complications in twin pregnancies: Systematic review and meta-analysis. BMJ. 2016;354:i4353.
- Steptoe PC, Edwards RG. Reimplantation of a human embryo with subsequent tubal pregnancy. Lancet. 1976;1(7965):880-2.
- Tilahun T, Araya F, Tura G. Incidence and risk factors of twin pregnancy at Jimma University Specialized Hospital, Southwest Ethiopia. Epidemiology (Sunnyvale). 2015;5(2):188.
- Preterm birth. Geneva:WHO, 2018. Available at: https://www.who.int/news room/fact-sheets/detail/preterm-birth. Accessed April 2021
- Gill SV, May-Benson TA, Teasdale A, Munsell EG. Birth and developmental correlates of birth weight in a sample of children with potential sensory processing disorder. BMC Pediatr. 2013;13:29.
- Committee Opinion Summary No. 640: Cell-Free DNA Screening for Fetal Aneuploidy. Obstet Gynecol. 2015;126(3):691-2.
- National Guideline Alliance (UK). Hypertension in pregnancy: diagnosis and management. London: National Institute for Health and Care Excellence: Clinical Guidelines. 2019;PMID:31498578.
- Diabetes in pregnancy: management from preconception to the postnatal period. London: National Institute for Health and Care Excellence: Clinical Guidelines. 2020;PMID:32212588.
- Dahlke JD, Mendez-Figueroa H, Maggio L, Hauspurg AK, Sperling JD, Chauhan SP, Rouse DJ. Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol. 2015;213(1):76.e1-76.e10.
- Tsuda H, Kotani T, Nakano T, Imai K, Ushida T, Hirakawa A, Kinoshita F, Takahashi Y, Iwagaki S, Kikkawa F. The rate of neonatal respiratory distress syndrome/transient tachypnea in the newborn and the amniotic lamellar body count in twin pregnancies compared with singleton pregnancies. Clin Chim Acta. 2018;484:293-7.
- Rashid D, Alalaf S. Maternal and perinatal outcomes in twin pregnancies conceived spontaneously and by assisted reproductive techniques: cross-sectional stud. East Mediterr Health. 2020;26(10):1285–93.




