Caracteristicile clinice ale nou-născuţilor cu sindrom de detresă respiratorie care au necesitat transferul cu ambulanţa la alte unităţi spitaliceşti
Clinical characteristics of the newborns with distress syndrome who required transfer by ambulance to other hospital units
Abstract
Introduction. Respiratory distress syndrome (RDS) is a frequent clinical critical disease and it represents a significant cause of death and disability in neonates. The availability of the proper intensive care facilities is different in neonatal services, and this is the reason why neonates must be transported to superior care centres. The purpose of our study was to identify the clinical characteristics of the neonates with RDS who are transported by ambulance to tertiary neonatal services. Materials and method. We realized a prospective study that included newborns with respiratory distress syndrome who required transfer by ambulance from a hospital that could not fulfill the newborn intensive care criteria to another hospital with a superior level of neonatal intensive care. Results. The analyzed group included 133 children with respiratory distress syndrome (RDS) who were transported by ambulance from one hospital to another between 2017 and 2020. The gender distribution showed a proportion of 60.3% males (79 children) and 39.7% (52 children) female newborns. Depending on the degree of prematurity, they are distributed as follows: 9.28% (nine newborns) were extreme preterm (less than 28 weeks), their average weight being 837.22 grams (standard deviation 248.761, CI: [646.01; 1028.44]), 30.93% (30 newborns) were born very preterm (28-32 weeks), their average weight being1388.67 grams (standard deviation 405.656, CI: [1237.19; 1540.14]), and 59.79% (58 newborns) were born moderate and late preterm (32-37 weeks), with an average weight of 2503.28 grams (standard deviation 737.065, CI: [2309.47; 2697.08]). The mean gestational age of the newborns who required resuscitation at birth was 33.06 weeks (standard deviation 4.302, CI: [32.02; 34.10]), and for those who did not need resuscitation the mean gestational age was 34.58 weeks of pregnancy (standard deviation 5.584, CI: [33.20; 35.97]). Conclusions. The neonatal transport represents an important medical issue. The clinical parameters of the newborns with RDS who require transport are represented by: prematurity, low Apgar scores at birth and neonatal resuscitation. Further randomised studies are necessary to bring additional information.Keywords
respiratory distress syndromeambulanceprematuritynewbornRezumat
Introducere. Sindromul de detresă respiratorie (SDR) este o patologie critică importantă şi reprezintă o cauză semnificativă de morbiditate şi mortalitate neonatală. Disponibilitatea mijloacelor adecvate de terapie intensivă este diferită în serviciile neonatale şi acesta este motivul pentru care nou-născuţii trebuie transportaţi la centre de îngrijire superioară. Scopul acestui studiu a fost de a identifica trăsăturile clinice ale nou-născuţilor cu SDR care sunt transportaţi cu ambulanţa la centrele neonatale terţiare. Materiale şi metodă. Am realizat un studiu prospectiv care a inclus nou-născuţi cu sindrom de detresă respiratorie ce au necesitat transferul cu ambulanţa dintr-un spital care nu putea îndeplini criteriile de îngrijire intensivă pentru aceştia la un alt spital cu un nivel superior de terapie intensivă neonatală. Rezultate. Grupul analizat a inclus 133 de copii cu sindrom de detresă respiratorie, care au fost transportaţi cu ambulanţa de la un spital la altul între 2017 şi 2020. Distribuţia în funcţie de sex a arătat o proporţie de 60,3% (79 de copii) a sexului masculin şi de 39,7% (52 de copii) a sexului feminin. În funcţie de gradul de prematuritate, nou-născuţii au fost distribuiţi astfel: 9,28% (nouă nou-născuţi) au fost cu prematuritate extremă (mai puţin de 28 de săptămâni), greutatea lor medie a fost de 837,22 grame (deviaţie standard de 248,761, CI: [646,01; 1028,44]), 30,93% (30 de nou-născuţi) au fost foarte prematuri (28-32 de săptămâni), greutatea lor medie a fost de 1388,67 grame (deviaţie standard de 405,656, CI: [1237,19; 1540,14]) şi 59,79% (58 de nou-născuţi) s-au născut ca prematuri medii sau tardivi (32-37 de săptămâni), cu o greutate medie de 2503,28 grame (deviaţie standard de 737,065, CI: [2309,47; 2697,08]). Vârsta gestaţională medie a nou-născuţilor care au necesitat resuscitare la naştere a fost de 33,06 săptămâni (deviaţie standard de 4,302, CI: [32,02; 34,10]), iar pentru cei care nu au avut nevoie de resuscitare, vârsta medie a fost de 34,58 săptămâni de sarcină (deviaţie standard de 5,584, CI: [33,20; 35,97]). Concluzii. Transportul neonatal reprezintă o problemă medicală importantă. Parametrii clinici ai nou-născuţilor cu RDS care necesită transport sunt reprezentaţi de: prematuritate, scoruri Apgar scăzute la naştere şi resuscitare neonatală. Sunt necesare studii randomizate suplimentare pentru a aduce informaţii suplimentare.Cuvinte Cheie
sindrom de detresă respiratorieambulanţăprematuritatenou-născutIntroduction
Respiratory distress syndrome (RDS) is a frequent clinical critical disease and it represents a significant cause of death and disability in neonates. The pathogenesis of respiratory distress syndrome is complex. It is an acute pulmonary inflammatory disease caused by the lack of pulmonary surfactant induced by various pathological factors. Sometimes, it is difficult to distinguish the neonatal RDS from other diseases(1). Neonates with RDS may need intensive care techniques, especially in early postpartum period(2). The availability of the proper intensive care facilities is different in neonatal services, and this is the reason why neonates must be transported to superior care centres. The purpose of our study was to identify the clinical characteristics of the neonates with RDS who are transported by ambulance to tertiary neonatal services.
Materials and method
We realized a prospective study that included newborns with respiratory distress syndrome who required transfer by ambulance from a hospital that could not fulfill the newborn intensive care criteria to another hospital with a superior level of neonatal intensive care. There were analyzed the clinical and biological parameters of the newborns who were transported. The records were made before and after the transport by ambulance. The present study presents only the clinical characteristics of the newborn before being transported by ambulance. The data were analyzed using SPSS version 23 software. P value was considered statistically significant for values below 0.05.
Results
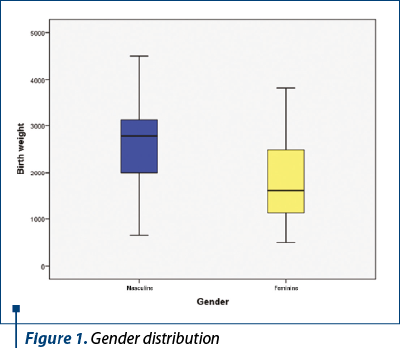
The analyzed group included 133 children with respiratory distress syndrome (RDS) who were transported by ambulance from one hospital to another between 2017 and 2020. The gender distribution revealed a proportion of 60.3% male (79 children) and 39.7% (52 children) female newborns (Figure 1).
At the time of their transport by ambulance, the newborns included in the analysis were aged between 1 hour and 63 days, with a mean age of 3.89 days (standard deviation 10.559, CI: [2.08; 5.71]). Among them, 87.2% (116) of the children included in the study were 1 week old, 6% (eight children) were between 8 and 14 days old, one child (0.8%) was between 15 and 21 days old, 3.8% (five children) were between 22 and 31 days old, and 2.2% (three children) were around 2 months old (58-63 days). Newborns with RDS included in the study had a weight between 500 and 4500 grams at birth, the average weight being 2271.54 grams (standard deviation 918.8, CI: [2113.94; 2429.14]).
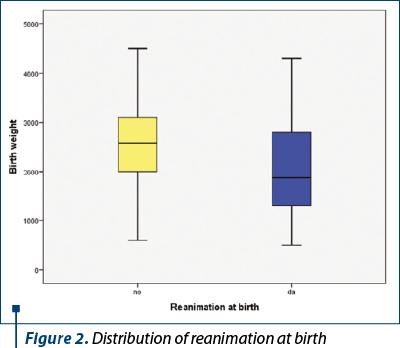
A percentage of 51.1% – representing 68 of the 133 newborns with RDS transferred to other hospitals – were resuscitated at birth, and 48.9% (65 children) did not need resuscitation.
There was a slight increase in cases that required resuscitation at birth among female newborns compared to males, but without a statistically significant association between the sex of the newborn and the need for resuscitation. Thus, 55.8% (29 children) of female newborns with RDS included in the study needed resuscitation at birth, while among boys with RDS, 48.1% (38 children) were resuscitated at birth.
The mean gestational age of the newborns who required resuscitation at birth was 33.06 weeks (standard deviation 4.302, CI: [32.02; 34.10]), and for those who did not need resuscitation, the mean gestational age was 34.58 weeks of pregnancy (standard deviation 5.584, CI: [33.20; 35.97]).
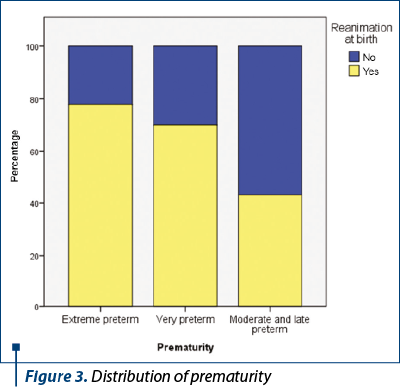
For resuscitated newborns, the mean Apgar score at birth was 5.26 (standard deviation 2.213, CI: [4.74; 5.79]), while for newborns who were not resuscitated at birth the mean Apgar score was 7.86 (standard deviation 0.998, CI: [7.61; 8.11]). It is observed that all babies with Apgar scores up to 5 (including 5) needed resuscitation at birth, and as the Apgar score improved, the need for resuscitation at birth decreased (Figures 2 and 4).
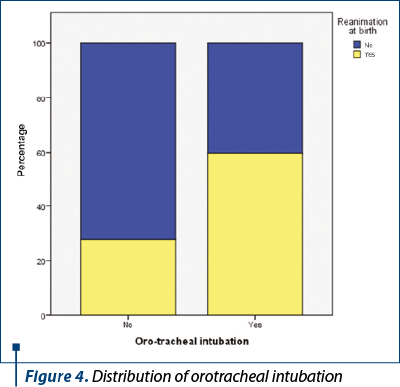
Depending on the gestational age at birth, the study group included 97 babies born prematurely, representing 73.48% of all babies. Depending on the degree of prematurity, they were distributed as follows: 9.28% (nine newborns) were extreme preterms (less than 28 weeks), their average weight being 837.22 grams (standard deviation 248,761, CI: [646.01; 1028.44]), 30.93% (30 newborns) were born very preterm (28-32 weeks), their average weight being 1388.67 grams (standard deviation 405.656, CI: [1237.19; 1540.14]), and 59.79% (58 newborns) were born moderate and late preterm (32-37 weeks), with an average weight of 2503.28 grams (standard deviation 737.065, CI: [2309.47; 2697.08]) – Figure 3.
For the babies with RDS from our study, there was an increased incidence of resuscitation among those born prematurely, compared to those born at term, but this difference is not statistically significant. Thus, 54.6% of children born prematurely needed resuscitation, while among those born at term, only 42.9% needed resuscitation. Although resuscitation at birth is not statistically significantly correlated with the prematurity of the newborns (referring to prematurity in general, regardless of its degree), the risk of preterm infants requiring resuscitation at birth increased by 27% compared to children born at term. However, it is noted that, as the degree of prematurity increased, the incidence of resuscitation at birth increased as follows: 43.1% of moderate or late preterm newborns, 70% very preterm newborns, respectively 77.8% extreme preterm newborns were resuscitated at birth.
Discussion
The transport of the newborns from one hospital to another is a current practice in the daily neonatal medicine. The clinical and biological parameters of the newborns before, during and after transport are extremely important for further neonatal outcome. The literature reports few studies about neonatal transport, especially for newborns with RDS.
The 2003 review of the United Kington neonatal services made several changes, including the centralisation of intensive care into third-level units. It was established the geographical organization of neonatal care into networks. Even though significant changes were made, the neonatal transport is still problematic(3). The same distribution on neonatal hospitals also exists in Romania. Thus, the need of transport of the newborns from inferior to superior tertiary care neonatal units is often required.
To understand the issues of the risk management associated with neonatal transport, which represents a branch of retrieval medicine, one needs to evaluate the infrastructure of the transport teams, to perform issues identification, incident reporting, feedback and learning from experience. The national picture for neonatal transport is evolving in some countries(4). A national survey was conducted in 2015 in order to assess the Neonatal Emergency Transport Services (NETS) status in the 20 Italian regions. Where it was available, NETS are well-equipped and organized, but the reduced volume of activities cannot guarantee the proper levels of skills of personnel. The regions who had a lack of NETS are trying to fill the gap, but continuing efforts to reduce regional differences in quality of services are needed(5).
The rapid resuscitation and the appropriate transportation of newborns can improve the infant’s survival. To gain an understanding of the status of neonatal transport in Japan, there was conducted a survey of neonatal transportation capabilities across the country. Thirteen percent of centers reported problems with the transportation of newborns in fire department ambulances. An adequate medical insurance coverage is required to increase the number of specialized ambulances(6).
The clinical characteristics of the newborns who require transport from a medical unit to another depend on the pathology that determined advanced medical care(7). There are only few communications about newborns with RDS who were transferred. There is a report about the respiratory management of neonates of 23 to 26 weeks of gestation transported after birth outside a tertiary center. This retrospective study realized over a three-year period proved that neonates born at 23 to 26 weeks of gestation outside tertiary centers had high rates of mortality and morbidity. Avoiding hypocarbia, hypercarbia and hyperoxia is challenging in the transport environment(8).
The management of neonates with acute respiratory syndrome often requires advanced intensive care procedures, such as endotracheal intubation and invasive mechanical ventilation(9). The same management was observed for children included in the present study. But it was also observed that applying noninvasive ventilation modalities from birth in the delivery room during fetal-neonatal transition reduced the need for invasive mechanical ventilation, the mortality and the bronchopulmonary dysplasia(10). The ability to perform rapid and correct intensive approach needs trained clinicians and adequated logistics(11). In most of the cases, the inability of medical units to offer these medical services represents the reasons for neonates’ transport.
The originality of our study consists in the unique character of the subject. There is no report regarding neonates’ transport in Romania. Furthermore, there is a lack of information about medical parameters of the newborns with RDS who need such medical action. The limit of the study is the reduced number of the patients and the lack of information regarding follow-up.
Conclusions
The neonatal transport represents an important medical issue. The clinical parameters of the newborns with RDS who require transport are represented by: prematurity, low Apgar scores at birth, and neonatal resuscitation. Further randomised studies are necessary to bring additional information.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Chi M, Mei YB, Feng ZC. A review on neonatal acute respiratory distress syndrome. Zhongguo Dang Dai Er Ke Za Zhi. 201820(9):724-8 [Chinese].
- Jena SR, Bains HS, Pandita A, Verma A, Gupta V, Kallem VR, Abdullah M, Kawdiya A. On behalf of sure group. Surfactant therapy in premature babies: SurE or InSurE. Pediatr Pulmonol. 2019;54(11):1747-52.
- Teasdale D, Hamilton C. Baby on the move: issues in neonatal transport. Paediatr Nurs. 2008;20(1):20-5.
- Ratnavel N. Safety and governance issues for neonatal transport services. Early Hum Dev. 2009;85(8):483-6.
- Gente M, Aufieri R, Agostino R, Fedeli T, Calevo MG, Massirio P, Bellini C. Neonatal Transport Study Group of the Italian Society of Neonatology (SIN). Nationwide survey of neonatal transportation practices in Italy. Ital J Pediatr. 2019;45(1):51.
- Hiroma T, Ichiba H, Wada K, Shiraishi J, Sugiura H, Nakamura T. Nationwide survey of neonatal transportation practices in Japan. Pediatr Int. 2016;58(4):311-3.
- Bellini C. The Neonatal transporter’s brain. Air Med J. 2020;39(1):24-6.
- Maheshwari R, Luig M. Review of respiratory management of extremely premature neonates during transport. Air Med J. 2014;33(6):286-91.
- Hussain WA, Marks JD. Approaches to Noninvasive Respiratory Support in Preterm Infants: From CPAP to NAVA. Neoreviews. 2019;20(4):e213-e221.
- Petrillo F, Valenzano L, Franco C, Calò G, Dentico D, Manzoni P, D’Amato G, Del Vecchio A. Pulmonary recruitment strategy in preterm neonates < 29 weeks of gestational age to reduce the need for intubation in the delivery room. Am J Perinatol. 2019;36(S02):S115-S119.
- Shi Y, De Luca D. NASal OscillatioN post-Extubation (NASONE) study group. Continuous positive airway pressure (CPAP) vs noninvasive positive pressure ventilation (NIPPV) vs noninvasive high frequency oscillation ventilation (NHFOV) as post-extubation support in preterm neonates: protocol for an assessor-blinded, multicenter, randomized controlled trial. BMC Pediatr. 2019;19(1):256.




