Stroke is an unusual fetal event, more frequently associated with premature birth and almost always appearing in the presence of a predisposing factor. There are cases described in literature in patients with Crohn’s disease, but also in patients with thrombophilia, especially with antiphospholipid syndrome. It is also described in fetal and neonatal cases of alloimmune thrombocytopenia.
Fetal stroke and thrombophilia – coincidence?
Accident vascular fetal într-un caz de trombofilie maternă – coincidenţă?
First published: 26 mai 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.40.2.2023.8050
Abstract
Rezumat
Accidentul vascular fetal este un eveniment neobişnuit, asociat mai frecvent cu naşterea prematură şi care apare aproape întotdeauna în prezenţa unui factor predispozant. Există cazuri descrise la pacienţi cu boala Crohn, dar şi la pacienţi cu trombofilie, în special cu sindrom antifosfolipidic. De asemenea, poate apărea în cazuri de trombocitopenie aloimună fetală sau neonatală.
Introduction
Stroke is an unusual fetal event, more frequently associated with premature birth and almost always appearing in the presence of a predisposing factor. There are cases described in literature in patients with Crohn’s disease, but also in patients with thrombophilia, especially with antiphospholipid syndrome (APS).
Case presentation
A 38-year-old patient, at her first pregnancy, with a gestational age of 36 weeks, diagnosed with thrombophilia, under treatment with low molecular weight heparin – LMWH (Clexane® 0.6 ml/24 h), from the eighth week of pregnancy, presented to the emergency room for reduced fetal movement.
A cardiotocography (CTG) was performed which showed abnormal results, including a low value for short term variability (STV) of 3.3. An ultrasound exam was performed which revealed an abnormal central nervous system (CNS) aspect that suggested either a severe brain hemorrhage or a preexistent brain lesion. The results were compared with preexistent tests. The patient had a 22-week anomaly scan that revealed a normal CNS and a 33-week scan that revealed normal images. A CTG had been performed seven days prior to admission and revealed a normal trace. Anticoagulant treatment was decided in the first trimester together with the hematologist, due to the presence of homozygous factor V Leyden, detected during the screening for thrombophilia.
Lab tests revealed normal coagulation (prothrombin time test, INR and partial thromboplastin time test). Based on previous knowledge from literature about fetal stroke, we tested the patient for the lupus anticoagulant and antiphospholipid antibodies. Both results were negative. Crohn’s disease was excluded through anamnesis.
Due to the association with thrombophilia and the subsequent treatment with LMWH, an overdose of anticoagulant was considered as a cause. A board of hematologists, obstetricians and maternal-fetal specialists analyzed the case and decided it was a correct dosage that was unlikely to generate such complications. The board decided to test the patient for alloimmune antiplatelet antibodies. The test came back positive for maternal antibodies against HPA-1a.
The patient was counseled regarding the unfavorable prognosis of the fetus, but after considering the special situation of the patient (first pregnancy at 38 years old and the unfavorable CTG result), a caesarean section was decided. We delivered a fetus of 2810 g, with an Apgar score of 7. At his transfontanellar postnatal ultrasound examination, the stroke was confirmed. The child presented petechiae and a low level of platelets (25,000/microliter of blood). Unfortunately, the postnatal evolution was unfavorable, with exitus happening 10 days postnatally.
Discussion
FNAIT and stroke
Fetal and neonatal alloimmune thrombocytopenia (FNAIT) is defined as a lowering of the number of fetal platelets below 150,000/microliter that results from maternal antibodies attacking fetal platelets with incompatible antigens. Though a rare occurrence, FNAIT is reported as the main cause of severe fetal thrombocytopenia (below 50,000/microliter) and the most common cause of fetal stroke in term babies(1).
Fetal stroke is a rare event, with approximately 10 cases at 100,000 births. It tends to be more severe with subsequent pregnancies and earlier in pregnancy, so in any cases with thrombocytopenia and stroke/intracerebral hemorrhage, we should look for FNAIT and devise a plan for future pregnancies(1,2).

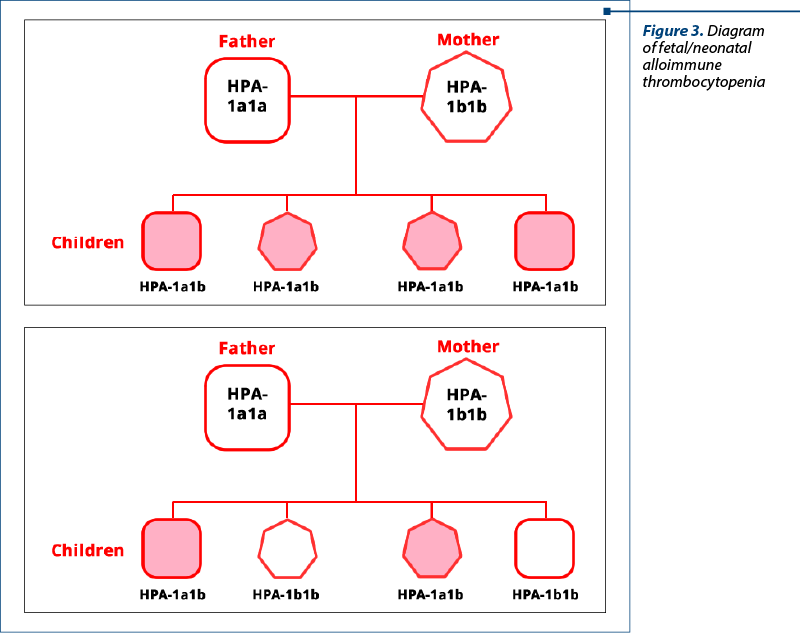
FNAIT is the platelets’ equivalent of red blood cells immunization. Platelets contain an antigen that is missing from the maternal platelets. Human platelets antigens (HPA) are inherited and each child inherits half of their antigens from each parent. For example, a child may inherit HPA-1a from the mother and HPA-1b from the father, and their type would be HPA-1a1b. Alternatively, the child might inherit HPA-1a from both the mother and the father, and it would be HPA-1a1a(1,3). A model of the inheritance is presented in Figure 2.
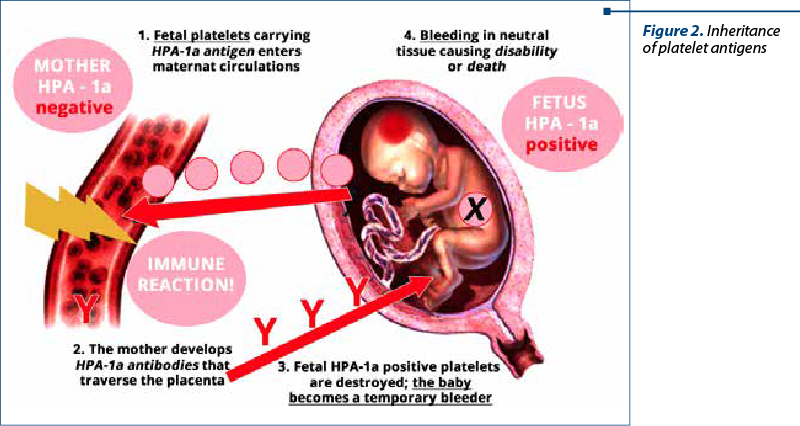
After a fetomaternal bleeding, maternal IgG antibodies are created against these antigens, they cross the placenta and reach the platelets antigen; this results in platelet destruction in the same way with erythrocytes’ Rh immunization. This leads to fetal/neonatal thrombocytopenia with different degrees of severity. The most common type of human platelet antigen is HPA-1a. Almost 80% of FNAIT cases have maternal antibodies against HPA-1a, all the rest of the antigens adding up to the rest of 20%. Studies have shown that in Caucasian women 92% have the HPA-1a type (either HPA-1a/HPA-1a, or HPA-1a/HPA-1b) and 2% are HPA-1a negative (HPA-1b/HPA-1b)(1,3,5). These data we can extrapolate to the Romanian population.
Causes of fetomaternal hemorrhage are:
-
Caesarean section
-
Vaginal birth
-
Abruptio placentae
-
Manual extraction of the placenta
-
Threatened abortion (our patient was admitted to the hospital on multiple occasions with this diagnosis)
-
Amniocentesis
-
Chorionic villus sampling (CVS)
-
Cephalic version.
Thrombophilia and fetal stroke
Antiphospholipid syndrome is an autoimmune disease that generates multiple complications in pregnancy when antiphospholipid antibodies are present. Antiphospholipid antibodies are well known for their thrombotic capacity that can generate complications to both the mother and the fetus. The signs that can determine us to look for antiphospholipid syndrome are repeated pregnancy loss, intrauterine growth restriction, preeclampsia and premature birth – all associated with placental and blood vessel pathology.
Although rare, fetal stroke has been described in newborns and fetuses from mothers with obstetrical antiphospholipid syndrome. This is the reason we tested our patient, who had other thrombophilia tests present, for antiphospholipid antibodies as well. The present literature describes cases with fetal brain hemorrhage and recommends testing for obstetrical antiphospholipid syndrome every time an unexplained fetal bleeding occurs(5).
Conclusions
Thrombophilia is part of the cases we face more and more often, due to the diagnostic possibilities. Although the attitude towards anticoagulant treatment is variable, anticoagulant treatment is part of the treatment scheme. Always when the patient receives anticoagulant treatment, this is the first suspect as a cause of hemorrhagic incidents, from subchorionic hematoma to abruptio placentae. Sometimes, when we are not sure about the cause, alternative explanations must be explored. The present case represents an exceptional situation obtained from a large group of patients with thrombophilia, who benefited from a pregnancy exploration that is different from the routine monitoring of a normal pregnancy. However, exceptional investigations are necessary in exceptional situations, and they can lead to a correct diagnosis and conduct.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
Mella MT, Eddleman K. Neonatal alloimmune thrombocytopenia. Int J Clin Transsf Med. 2015;3:29-40.
-
Lin TH, Lee CN, Su YN. Lethal fetal stroke in utero. Taiwan J Obstet Gynecol. 2013;52(2):264-6.
-
Platelet antigens and antibodies in pregnancy. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/14677/platelet-antigens-and-antibodies-in-pregnancy.pdf
-
Dębska M, Uhrynowska M, Guz K, Kopeć I, Lachert E, Orzińska A, Kretowicz P, Antoniewicz-Papis J, Dębski R, Łętowska M, Husebekk A, Brojer E. Identification and follow-up of pregnant women with platelet-type human platelet antigen (HPA)-1bb alloimmunized with fetal HPA-1a. Arch Med Sci. 2018;14(5):1041-7.
-
Bouw MC, Nij Bijvank SWA, Bouwhuis JW, van Wezel-Meijler G. Fetal intraventricular hemorrhage due to antiphospholipid syndrome: a case report. Front Pediatr. 2021;8:622597.