Fetal horseshoe kidney – a type of congenital anomaly of the kidney and urinary tract (CAKUT) where the lower poles of both kidneys are fused – is often linked to other conditions, highlighting the importance of a comprehensive evaluation. This paper provides an overview of this condition, elucidating the intricacies of its detection during prenatal ultrasound examinations. Focusing on the second trimester, when detailed fetal anatomy scans are conducted, the paper explores the specific ultrasound markers crucial for accurate diagnosis, the proper management, and the patients’ counseling in these cases. By examining the nuances of fetal horseshoe kidney, this paper contributes with valuable insights to the field of prenatal diagnosis, proactive care, and informed decision-making for affected families.
Horseshoe kidney – fetal ultrasound diagnosis
Rinichiul în potcoavă – diagnostic prenatal ecografic
First published: 27 noiembrie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.42.4.2023.8991
Abstract
Rezumat
Rinichiul în potcoavă este o anomalie congenitală a rinichiului şi tractului urinar (CAKUT) în care polii renali inferiori sunt fuzionaţi. Fiind adesea asociat cu alte malformaţii, acest diagnostic necesită o evaluare minuţioasă a anatomiei fetale, cât şi testare prenatală invazivă. Articolul oferă o prezentare generală a acestei afecţiuni, subliniind complexitatea detectării sale în timpul examinărilor ecografice prenatale. Anomaliile sistemului renal se diagnostichează de obicei în cadrul morfologiei din trimestrul al doilea, când se efectuează scanări detaliate ale anatomiei fetale. Lucrarea are contribuţii valoroase în domeniul diagnosticului prenatal, prezentând markerii ecografici esenţiali şi paşii corecţi pentru diagnostic şi management, cât şi consilierea adecvată în asemenea cazuri.
Introduction
The spectrum of congenital anomalies of the kidney and urinary tract (CAKUT) is broad, ranging from mild cases involving unilateral hydronephrosis to severe instances characterized by renal agenesis. Ultrasound examinations play a pivotal role in visualizing kidneys as early as nine weeks of gestation, although kidney assessment primarily occurs during the second-trimester anomaly scan, usually between 20 and 24 weeks. The evaluation of the urinary tract focuses on the anatomy of kidneys, ureters and fetal bladder, but there are also considered parameters such as amniotic fluid volume, the progression of abnormalities, and anomalies in associated structures(1).
Fetal ultrasound examinations during the second trimester are pivotal in identifying various congenital anomalies, including urinary tract abnormalities like horseshoe kidney. This condition, where the lower poles of both kidneys fuse in front of the descending aorta, affects approximately 1 in 400 births and shows a higher prevalence in male fetuses(2). This is the most common type of renal fusion anomaly. It consists of two distinct functioning kidneys on each side of the midline, connected at the lower poles (or, rarely, at the upper poles) by an isthmus of functioning renal parenchyma or fibrous tissue that crosses the midline of the body(3). This finding is frequently asymptomatic and detected incidentally during renal imaging. However, it can be associated with an increased risk for infections, nephrolithiasis with consequent hydronephrosis, ureteropelvic junction obstruction and vesicoureteral reflux. In addition, an increased risk for extrarenal disorders has been associated with this disorder(4).
Ultrasound diagnosis
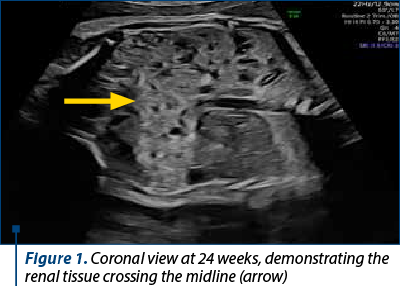
Horseshoe kidney diagnosis is made through meticulous ultrasound examinations. The fusion of lower kidney poles, forming a distinct “U” or “s-shaped” structure, is best demonstrated on coronal and transverse scans, where renal tissue crosses the midline (Figure 1). Notably, a normal bladder and amniotic fluid volume is observed in these cases, aiding in accurate diagnosis(1).
Associated abnormalities
Horseshoe kidney is often linked to other conditions, highlighting the importance of a comprehensive ultrasound evaluation. There is an increased risk for extrarenal disorders: 30% of the cases can have associated gastrointestinal tract and vertebral malformations, CNS disorders, cardiovascular disease, hydronephrosis, and genital anomalies.
Approximately 30% of cases are associated with Turner syndrome, and 20% are observed in trisomy 18(5). Syndromes like caudal regression syndrome, characterized by sacral agenesis or hypoplasia, hypoplastic vertebral bodies, and anal atresia, are found in 15% of cases. In addition, the horseshoe kidney has been described in association with 11p13 deletions at WAGR (Wilms tumor, aniridia, genitourinary abnormalities, and mental retardation) locus. Also, it has been reported in diverse single-gene disorders, such as Fanconi anemia, tuberous sclerosis complex, Townes-Brocks syndrome, Aicardi-Goutières syndrome, SOX2 gene-related anophthalmia syndrome, Alagille syndrome, and many other monogenic disorders. Furthermore, the horseshoe kidney was reported to be associated with several copy number variants detectable by chromosomal microarray analysis (CMA). For instance, it has been reported in patients with a rare 3q29 microdeletion syndrome, characterized by mild-to-moderate mental retardation, slightly dysmorphic facial features and nonspecific malformations(6-8). Of note, in most of these conditions, renal fusion is usually associated with additional anatomic abnormalities.
Investigations and follow-up
Detailed ultrasound examinations are crucial for the accurate diagnosis. The management of prenatally detected horseshoe kidneys frequently includes genetic counseling and recommendations for invasive prenatal testing – amniocentesis(9,10).
For ongoing monitoring, ultrasound scans every four weeks are recommended to detect potential late-onset hydronephrosis, a common complication. This proactive approach ensures timely interventions and comprehensive care.
Management and prognosis
Standard obstetric care and delivery are pursued for cases of horseshoe kidney. In isolated forms, the prognosis is generally favorable. However, postnatal follow-up is imperative due to the significant risk of infections, hydronephrosis and nephrolithiasis, observed in 70% of cases(9,10). Regular follow-ups facilitate early detection and intervention, enhancing the child’s overall quality of life.
Recurrence and genetic considerations
The recurrence risk of isolated horseshoe kidney is not significantly increased. In cases associated with Turner syndrome, there is no elevated risk of recurrence. However, when horseshoe kidney is a part of trisomy 18, the recurrence rate is approximately 1%, emphasizing the importance of genetic counseling for affected families(5).
Conclusions
The accurate ultrasound diagnosis of fetal horseshoe kidney is key in providing proactive care. Genetic counselling is essential, ensuring informed decision-making for affected families. Timely monitoring and counseling contribute to the overall well-being of the child and help in addressing potential complications effectively.
Conflict of interest: none declared.
financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.

Bibliografie
-
Savvidou M, Dhillon KH. Urinary tract abnormalities. In: Coady AM, Bower S. Twining’s textbook of fetal abnormalities. 3rd Ed, Churchill Livingstone/Elsevier, Philadelphia. 2015;479-517.
-
Basar H, Basar R, Basar MM, Erbil M. The comparison of the incidence of horseshoe kidney in autopsy cases versus urologic patient population. Okajimas Folia Anat Jpn. 1999;76(2-3):137–9.
-
Yoshinaga K, Kodama K, Tanii I, Toshimori K. Morphological study of a horseshoe kidney with special reference to the vascular system. Anat Sci Int. 2002;77(2):134–9.
-
Caccetta F, Caroppo M, Musio F, et al. Rene a ferro di cavallo: non è una semplice anomalia di fusione. Analisi di due casi clinici e revisione della letteratura [Horseshoe kidney: not a simple fusion anomaly]. G Ital Nefrol. 2015;32(4):gin/32.4.4.
-
Arslansoyu-Camlar S, Soylu A, Abaci A, Turkmen MA, Ulgenalp A, Kavukcu S. Horseshoe kidney with growth retardation: don’t forget Turner syndrome. Turk J Pediatrics. 2016;58(2):227–9.
-
Je BK, Kim HK, Horn PS. Incidence and spectrum of renal complications and extrarenal diseases and syndromes in 380 children and young adults with horseshoe kidney. AJR Am J Roentgenol. 2015;205(6):1306–14.
-
Fantes JA, Bickmore WA, Fletcher JM, Ballesta F, Hanson IM, van Heyningen V. Submicroscopic deletions at the WAGR locus, revealed by nonradioactive in situ hybridization. Am J Hum Genet. 1992;51(6):1286–94.
-
Hindryckx A, De Catte L. Prenatal diagnosis of congenital renal and urinary tract malformations. Facts Views Vis Obgyn. 2011;3(3):165-74.
-
Allan PL. Kidneys: anatomy and technique. In: Allan PL, Baxter GM, Weston M. Clinical ultrasound. 3rd Ed, Livingstone Elsevier, Edinburgh Scotland. 2011;413-27.
-
Kovo-Hasharoni M, Mashiach R, Levy S, Meizner I. Prenatal sonographic diagnosis of horseshoe kidney. J Clin Ultrasound. 1997;25(7):405–7.