Introduction. The fact that thrombophilia is a factor involved in the pathogenesis of preeclampsia is a hypothesis supported bidirectionally by numerous contradictory results; however, it is estimated that approximately 40% of patients with preeclampsia have a thrombophilic substrate. Most valid studies do not support an association between inherited thrombophilia and preeclampsia, intrauterine growth restriction or spontaneous abortion, thus implicitly not supporting the prophylactic anticoagulant treatment with low-molecular-weight heparin (LMWH) for the prevention of the aforementioned conditions. Materials and method. We selected pregnant women with developing or spontaneous discontinued pregnancy undergoing anticoagulant or antiplatelet treatment. In the context where clear protocols for the administration of anticoagulants in pregnancy have not yet been established, we aimed to perform a comparative analysis of the clinical and anamnestic aspects on which the indication of treatment with antiplatelet, anticoagulant or the two combined in pregnancy were based and the impact on placental function by comparative analysis of the values of the Doppler measurements for the uterine, umbilical and average cerebral arteries of the patients included in the three study groups. Results. Spontaneous abortions or intrauterine fetal death in the antecedents was the main criterion for recommending antiplatelet, anticoagulant or combined treatment. In the presence of a personal history of thrombotic events, the combined treatment of LMWH and low-dose aspirin was chosen. We did not obtain a significant difference in the frequency of spontaneous pregnancy loss between the three study groups, the proportion of this condition being similar. Conclusions. The combined treatment of LMWH and low-dose aspirin in pregnancy was significantly correlated with the values of the resistance and pulsatility index of the uterine arteries closest to the normal values, with an average pulsatility index lower than 1, in particular for the left uterine artery, compared to the results obtained for the single treatment with low-dose aspirin or LMWH.
Analiza comparativă a impactului asupra sarcinii a aspirinei în doză mică, a heparinei de masă moleculară mică şi a tratamentului combinat, obiectivat prin valorile velocimetriei Doppler
Comparative analysis of the impact on pregnancy of low-dose aspirin, low-molecular-weight heparine and combined treatment objectified by values of Doppler velocimetry
First published: 16 martie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.68.1.2020.3036
Abstract
Rezumat
Introducere. Trombofilia ca factor implicat în patogeneza preeclampsiei este o ipoteză susţinută bidirecţional de numeroasele rezultate contradictorii; cu toate acestea, se estimează că aproximativ 40% dintre pacientele cu preeclampsie au un substrat trombofilic. Majoritatea studiilor valabile nu susţin o asociere între trombofilia moştenită şi preeclampsie, restricţia de creştere intrauterină sau avortul spontan, deci implicit nu susţin tratamentul anticoagulant profilactic cu heparină cu greutate moleculară mică (HGMM) pentru prevenirea celor menţionate anterior. Materiale şi metodă. Am selectat femeile gravide, cu sarcină în curs sau oprită din evoluţie, care urmează tratament anticoagulant sau antiplachetar. În contextul în care nu au fost încă stabilite protocoale clare pentru administrarea de anticoagulante în sarcină, am urmărit să realizăm o analiză comparativă a aspectelor clinice şi anamnestice pe care s-a bazat indicarea tratamentului cu antiagregant plachetar, anticoagulant sau cu cele două combinate în sarcină şi impactul asupra funcţiei placentare prin analiza comparativă a valorilor măsurătorilor Doppler pentru arterele uterine, ombilicală şi cerebrală medie ale pacientelor incluse în cele trei grupuri de studiu. Rezultate. Avorturile spontane sau decesul fetal intrauterin în antecedente a fost criteriul principal pentru recomandarea tratamentului antiplachetar, anticoagulant sau combinat. În prezenţa unui istoric personal de evenimente trombotice, tratamentul preferenţial a fost cel combinat, respectiv HGMM şi aspirină în doză mică. Nu am obţinut o diferenţă semnificativă în ceea ce priveşte frecvenţa avorturilor spontane între cele trei grupuri de studiu, proporţia acestora fiind similară. Concluzii. Tratamentul cu HGMM şi aspirină în doză mică, combinat în sarcină, a fost corelat semnificativ cu valorile indicelui de rezistenţă şi pulsatilitate al arterelor uterine, cel mai apropiat de valorile normale, cu un indice mediu de pulsatilitate mai mic decât 1, în special pentru artera uterină stângă, comparativ cu rezultatele obţinute pentru tratamentul cu aspirină în doză mică sau HGMM singular.
Introduction
The overall rate of thrombotic incidents during pregnancy is reported to be 200 cases per 100,000 births(1), and this rate is increasing to 500 per 100,000 cases postpartum and is associated with a maternal mortality rate of 1.2-4.7 per 100,000 pregnancies. The physiological changes during pregnancy cause most of the thrombotic events that occur in the postpartum period. The hormonal changes during pregnancy lead to increased levels of coagulation cascades factors, such as fibrinogen factor VII, VIII, X and von Willebrand. Other physiological changes during pregnancy include increased resistance to activated protein C in the second and third trimesters, decreased protein S activity due to changes in total protein S antigen, increased levels of fibrinolysis pathway inhibitors such as activin fibrinolysis inhibitor and plasminogen activator inhibitor 1 and 2 (PAI-1 and PAI-2)(2).
The prognosis of pregnancies complicated with thrombophilia, the associations with some complications, such as spontaneous abortion, preeclampsia, intrauterine growth restriction and abruptio placentae, have been investigated for a long time.
Previous studies that have analyzed the relationship between thrombophilia and spontaneous abortion reported contradictory results. One of the most influential studies found an association between fetal death and factor V mutation with an odds ratio of 10.9(3), without finding a significant association between thrombophilia and early miscarriage.
An increased average risk for spontaneous abortion in trimesters I and II and a relationship of association with recurrent abortion were also found for the prothrombin gene mutation(4); however, the involvement of other thrombophilic mutations was not clarified. The European Prospective Cohort on Thrombophilia study included 843 thrombophilic women and found an association between the number of thrombophilic mutations and the number of spontaneous abortions, with an odds ratio of 14.3 for fetal death in utero, but did not demonstrate a convincing association between thrombophilic mutations and spontaneous early abortion, the results of this study suggesting that antithrombin deficiency plays a role in the early spontaneous abortion(5).
The fact that thrombophilia is a factor involved in the pathogenesis of preeclampsia is a hypothesis supported bidirectionally by numerous contradictory results; however, it is estimated that approximately 40% of patients with preeclampsia have a thrombophilic substrate(6).
Most valid studies do not support an association between inherited thrombophilia and preeclampsia, intrauterine growth restriction or spontaneous abortion, thus implicitly not supporting the prophylactic anticoagulant treatment with low-molecular-weight heparin (LMWH) for the prevention of the aforementioned conditions.
Numerous meta-analyses, however, concluded that large studies suggest the absence of the effect of anticoagulant treatment on pregnancy in the prevention of complications related to placental function abnormalities, whereas smaller studies show that LMWH can prevent the recurrent complications mediated by placental function abnormalities.
Materials and method
We selected pregnant women with developing or spontaneous discontinued pregnancy undergoing anticoagulant or antiaggregate treatment, which were divided into three study groups: Group 1 included pregnant patients on low-dose aspirin treatment, Group 2 included pregnant patients with LMWH treatment, and Group 3 included pregnant patients on low-dose aspirin plus LMWH treatment.
A total of 385 cases were included in the study, and the groups were divided as follows: Group 1 – 65.6%, Group 2 – 22.7%, and Group 3 – 11.6%. In the context where clear protocols for the administration of anticoagulants in pregnancy have not yet been established, we aimed to perform a comparative analysis of the clinical and anamnestic aspects on which the indication of treatment with antiplatelet, anticoagulant or the two combined in pregnancy was based on, and the impact on placental function by a comparative analysis of the values of the Doppler measurements for the uterine, umbilical and average cerebral arteries of the patients included in the three study groups. The impact of Body Mass Index (BMI) on the treatment targeting decision was analyzed comparatively. This was calculated using the standard international formula and the patients were categorized according to the World Health Organization (WHO) weight classification.
Furthermore, the anamnesis that guides the management of an incipient pregnancy is the history of pregnancy loss, hence we also analyzed the existence of a link between this criterion with the BMI value for each study group. The personal history included the personal thrombotic history, the family history of thrombotic accidents, and the personal history of obstetric complications. The positive history of pregnancy losses was analyzed in detail by categorizing this criterion and if the pregnancy loss was consecutive or not.
Furthermore, we studied the number of pregnancies completed favorably by the birth of a live, term newborn. The modified values of Doppler velocimetry are an adverse prognostic indicator, reflecting a dysfunction of the uterus-placental circulation and implicitly translating a disorder of placental function. Hence, we analyzed the values of the resistance and pulsatility index of the uterine, cerebral and umbilical arteries for cases included in the study and we performed their comparative analysis for the three studied groups.
For all these variables and their corresponding analysis, parametric and non-parametric tests were used to validate the results. The cases included in the study were extracted from the database of project RO19.10 “Improvement of health services in high-risk pregnancy, premature birth and haematological diseases” within the Department of Monitoring of Thrombophilic Pregnancy with High Obstetric Risk, collected prospectively, during the period 2015-2017.
Results
Regarding the distribution of BMI in the three study groups (Table 1), in Group 2, the BMI values were significantly higher in pregnant patients undergoing LMWH treatment than in those undergoing treatment with LMWH and low-dose aspirin combined.
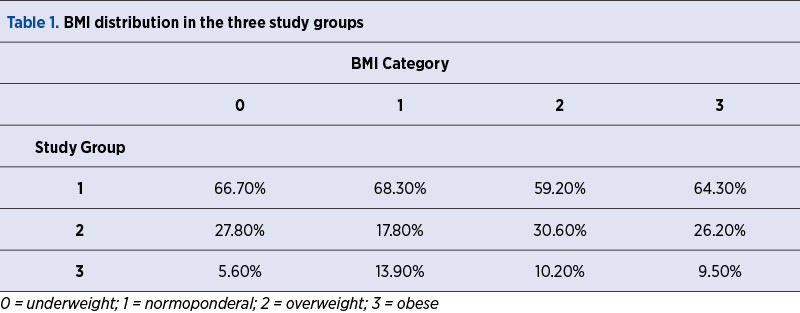
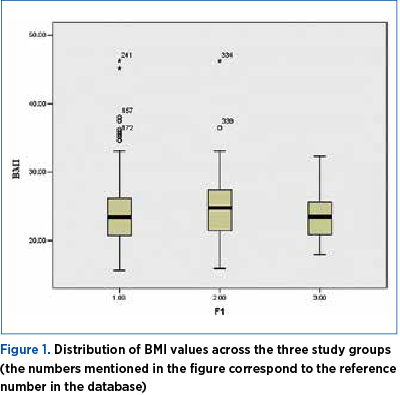
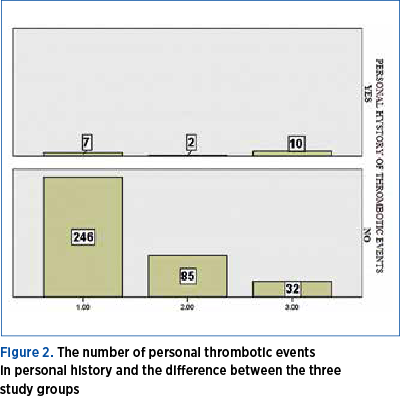
The graphical representation (Figure 1) shows schematically the values of BMI in the three study groups, and they are higher in Group 2. The personal history of thrombotic events is an indicator of anticoagulant treatment in pregnancy and puerperium, depending on its severity. Thus, according to the obtained results, in the presence of a personal history of thrombotic events, the combined treatment of LMWH and low-dose aspirin was chosen (Figure 2). Nonparametric tests demonstrated a statistical difference between the number of personal thrombotic antecedents in the group of pregnant patients treated with LMWH and low-dose aspirin compared with the groups of patients treated with LMWH or low-dose aspirin, alone.
A similar result was obtained for the family history of thrombotic events, also considered a risk factor for thrombosis in pregnancy and an indicator of anticoagulant treatment depending on the severity.
Figure 3 shows a significantly higher number of cases of family history of thrombotic events in Group 3. Hence, in patients with a family history of thrombotic events, the combined treatment of LMWH and low-dose aspirin was chosen.
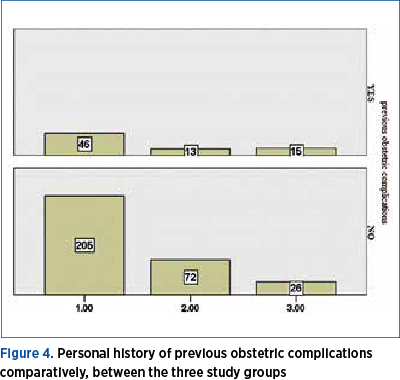
The difference obtained between Groups 3 and 1, respectively between Group 3 and Group 2, was statistically significant, with no statistically significant difference between Groups 1 and 2. For all three study groups, we obtained a personal history of previous obstetric complications, a history that included premature birth, intrauterine growth restriction, abruptio placentae, preeclampsia or eclampsia and intrauterine fetal death, and we compared for statistical significance.
The number of positive histories of obstetric complications was 22% of the first study group, respectively Group 1, of the patients being treated with low-dose aspirin; Group 2 had 18% of the positive history of obstetric complications, and Group 3 had over 50% of cases with a positive history of obstetric complications (Figure 4).

The personal history of the spontaneous loss of a pregnancy or recurrent miscarriages requires the clinician to increase the spectrum of investigations, implicitly to consider the presence of a thrombophilic substrate. Starting from this premise, we further analyzed the history of spontaneous pregnancy loss in terms of the number, succession and gestational age of the pregnancy/their spontaneous loss.
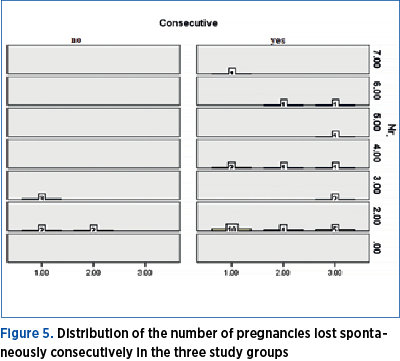
Thus, the situation of the frequency and division by gestational age of the cases included in the three study groups is presented in Figure 5, along with the situation regarding their consecutive character, representing the comparative analysis by nonparametric tests of the total number of pregnancy losses. We did not obtain a significant difference in the frequency of spontaneous pregnancy loss between the three study groups, the proportion of this condition being similar.
Regarding the risk of consecutive pregnancy loss, we observed that it was higher in Group 1 compared to that of the patients undergoing low-dose aspirin treatment.
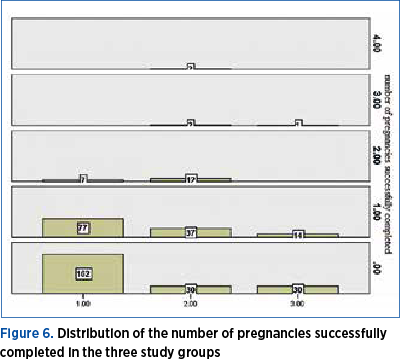
By performing nonparametric tests, we obtained a significant difference for Group 2, respectively of patients undergoing treatment with LMWH, compared with Group 3, that of patients undergoing combined aspirin plus LMWH treatment, regarding the number of pregnancies completed by term birth.
Additionally, there was a significant difference between Group 1, that of patients on aspirin treatment, and Group 2.
Patients undergoing treatment with LMWH had the most favorable history of successfully completed pregnancies (Figure 6). One of the indications for the initiation of low-dose aspirin treatment is the high resistivity index of uterine arteries.
LMWH is reserved, according to existing protocols, to cases of major thrombophilia with other associated risk factors. All pregnancy cases treated with low-dose aspirin, LMWH or combined treatment were subjected to ultrasound examination corresponding to their gestational age.
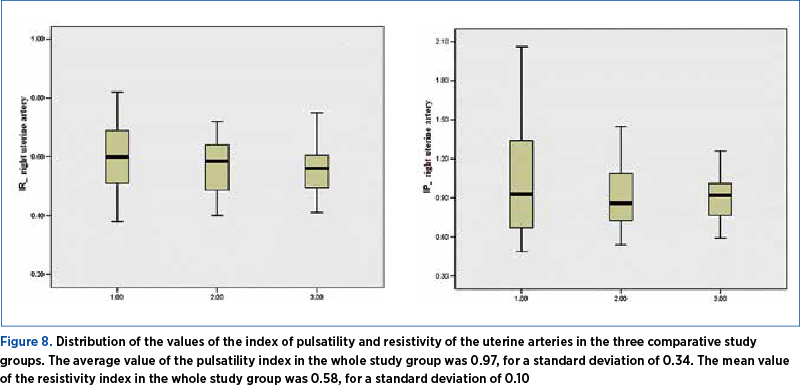
According to the results of the nonparametric tests, we found a statistically significant difference in terms of the values of the index of pulsatility and resistivity of the left uterine arteries between Group 1, that of patients undergoing aspirin treatment, and Group 3, those with combined treatment, LMWH plus aspirin. Group 3 had reduced values compared to Group 1 (Figures 7 and 8). A significant difference for the resistivity and pulsatility index of the uterine right arteries, the cerebral and umbilical arteries was not observed. The average value of the pulsatility index in the whole study group was 1.64, for a standard deviation of 0.265. The mean value of the resistivity index in the whole study group was 0.8, for a standard deviation of 0.057.
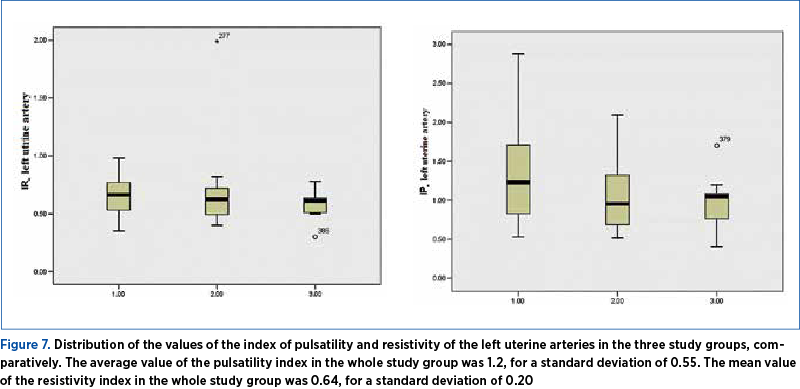
The average value of the pulsatility index in the whole study group was 1.23, for a standard deviation of 0.398. The mean value of the resistivity index in the whole study group was 0.68, for a standard deviation of 0.07.
Discussion
The treatment with LMWH is recommended, according to the guidelines of the Romanian Society of Obstetrics and Gynecology, for patients with known thrombophilia: protein C deficiency, Leiden Factor V mutation, prothrombin gene mutation 20210 and protein S deficiency (moderate risk), and for patients with high-risk thrombophilia who have not had a previous thrombotic episode with prophylactic doses of LMWH or UFH (unfractionated heparin) during pregnancy, started as early as possible and in postpartum.
According to the obtained results, the patients undergoing treatment with LMWH had a significantly higher BMI than those receiving aspirin or both treatments combined. The direction of therapeutic behavior was most likely guided by the results of numerous studies which have shown that obesity is an independent risk factor for spontaneous abortion for euploid pregnancies, yet there are no studies showing the preventive effect of weight loss for this risk.
Contrarily, a study investigating an impressive number of approximately 55,000 pregnancies to analyze the link between intrauterine fetal death and obesity(7) showed that preconceptional obesity is associated with an increased risk of fetal intrauterine death, a risk that increase in direct proportion to the gestational age and which is based on the placental dysfunction.
Both personal and family history of thrombotic injury represent indications of approaching prophylactic anticoagulant treatment in pregnancy(8). According to the obtained results, the incidence of personal thrombotic history was 5% in the study group. In the presence of this factor, the combined treatment of aspirin and LMWH was preferred. In the study group, the treatment decisions were made before the biological objectification of the existence of a thrombophilic pathology.
Low-dose aspirin administered during pregnancy has shown to be effective in facilitating placentation and improving prognosis through preventive effect on the development of preeclampsia. These two combined approaches present two separate mechanisms of action and their overlap could provide the desired evolution of the pregnancy. Additionally, patients with a family history of thrombotic injury had a high incidence of approximately 40% in the study group. More than half of the cases for which aspirin and LMWH combined treatment was chosen had one or more thrombotic accidents in the family history. The family history of thromboembolic disease is a risk factor for the existence of a procoagulant status that can be augmented by the prothrombotic changes associated with pregnancy.
The highest incidence of personal history of obstetric complications was also in the group of patients undergoing combined treatment in pregnancy. The proportion was lower among patients opting for anticoagulant treatment with LMWH alone (18%), respectively Group 2. Conditions such as premature birth, intrauterine growth restriction, abruptio placentae, preeclampsia or eclampsia and fetal death in utero have been associated with the presence of thrombophilia in numerous studies. Each of these complications can translate into placental dysfunction with increased risk of recurrence. In this context, the management of these cases relies on the fact that both low-dose aspirin treatment, as well as anticoagulant treatment facilitate placental function.
Spontaneous abortions or intrauterine fetal death in the antecedents was the main criterion for recommending antiplatelet, anticoagulant or combined treatment. As shown in the results section, the number of pregnancies lost in all three study groups is significant, and the proportion of consecutive spontaneous abortions has dominated in the personal history of patients on low-dose aspirin treatment. Moreover, nulliparity was more common in Group 1 than in Group 2, and a significant proportion of the nulliparous cases were registered in the group of patients undergoing treatment with aspirin and LMWH combined.
A special discussion is offered for the Doppler velocimetry of the cases included in the study. The results obtained in this study showed a significantly lower resistance and pulsatility index in patients undergoing combined treatment with LMWH and aspirin, but only for the left uterine artery. Velocimetry of the uterine arteries is a predictive test for the subsequent unfavorable evolution of the pregnancy, reflecting the situation of the uterus-placental vascularization, and if measured early in the first trimester, it offers the possibility of the prophylactic intervention that could significantly decrease the risk of IUGR (intrauterine growth restriction) and preeclampsia(9). The unfavorable prognosis of pregnancy associated with the values of the initial resistance and increased pulsatility was evaluated to be 75% for the development of preeclampsia and 86% for IUGR, in terms of sensitivity(10).
For the entire study group, the values of the resistance and pulsatility index of the uterine arteries, umbilical and mid cerebral artery (Figures 7 and 8) were normal, however the lowest values, reflecting the most effective treatment in facilitating the vascularization at the uterus-placental level, were for the combined one.
Conclusions
Thrombophilia screening is not mandatory in pregnancy and is recommended only for high-risk cases, based on personal, family and obstetric background. Until relatively recently, this screening involved additional costs. This study demonstrated that thrombophilia screening could help determine the prognosis of pregnancy by directing the anticoagulant and antiplatelet treatment in pregnancy, depending on the clinical and anamnestic condition.
Thus, for obese pregnant patients, the preferred option was prophylactic anticoagulant treatment, considering their risk of developing cardiovascular diseases; this treatment facilitates utero-placental circulation which prevents preeclampsia and the adverse prognosis of pregnancy due to spontaneous abortion or intrauterine fetal death.
The presence in the personal or family history of the thromboembolic events represented a criterion for the administration of the combined therapy of LMWH and low-dose aspirin to the detriment of their administration as separate treatments.
Nulliparity and spontaneous abortion, especially recurrent or intrauterine fetal death, were criteria for low-dose aspirin administration in pregnancy and for a significant number of cases of LMWH supplementation.
The importance of the recorded Doppler velocimetry is also notable. The combined treatment of LMWH and low-dose aspirin in pregnancy was significantly correlated with the values of the resistance and pulsatility index of the uterine arteries closest to the normal values, with an average pulsatility index lower than 1, in particular for the left uterine artery, compared with the results obtained for the single treatment with low-dose aspirin or LMWH.
The introduction of aspirin and/or LMWH treatment had revolutionary results for improving the prognosis of risky pregnancy, both in the context of a thrombophilic substrate and in the presence of other risk factors for preeclampsia, IUGR, spontaneous abortion, intrauterine fetal death or thrombotic events in pregnancy.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
2. Antovic A, Blombäck M, Bremme K, He S. The assay of overall haemostasis potential used to monitor the low molecular mass (weight) heparin, dalteparin, treatment in pregnant women with previous thromboembolism. Blood Coagulation and Fibrinolysis. 2002; 13:3:181–6.
3. Kocher O, Cirovic C, Malynn E, et al. Obstetric complications in patients with hereditary thrombophilia identified using the LCx microparticle enzyme immunoassay: a controlled study of 5,000 patients. American Journal of Clinical Pathology. 2007; 127, 1: 68–75.
4. Rey E, Kahn SR, David M, Shrier I. Thrombophilic disorders and fetal loss: a meta-analysis. The Lancet. 2003; 361, 9361:901–8.
5. Preston FE, Rosendaal FR, Walker ID, et al. Increased fetal loss in women with heritable thrombophilia. The Lancet. 2014; 348, 9032:913–16.
6. van Pampus MG, Dekker GA, Wolf H, et al. High prevalence of hemostatic abnormalities in women with a history of severe preeclampsia. American Journal of Obstetrics and Gynecol. 199l; 180, 5:1146–50.
7. Nohr EA, Bech, Bodil H, Davies MJ, Frydenberg M, Henriksen TB, Olsen J. Prepregnancy Obesity and Fetal Death: A Study Within the Danish National Birth Cohort. Obstetrics & Gynecol. 2005; 106, 2:250-9.
8. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among U.S. adults, 1999–2000. JAMA. 2002; 288:1723–7.
9. Velauthar L, Plana MN, Kalidindi M, et al. First-trimester uterine artery Doppler and adverse pregnancy outcome: a meta-analysis involving 55,974 women. Ultrasound Obstet Gynecol. 2014; 43:500–507.
10. Becker R, Vonk R, Vollert W, Entezami M. Doppler Sonography of uterine arteries at 20-23 weeks: Risk assessment of adverse pregnancy outcome by quantification of impedance and notch. J Perinat Med. 2005; 30:388–94.