Preinvasive cervical lesions have a long period of evolution towards cervical cancer, therefore their early detection and treatment, along with anti-HPV vaccination, are a necessity in preventing the occurrence of invasive cervical cancer. Genital HPV infection is the most common sexually transmitted infection. The objective of the study was to establish the prediction of the cervicovaginal cyto-tumor examination and the colposcopic examination for cervical dysplastic lesions and the histopathological examination of the fragments obtained by cervical biopsy, as well as the reevaluation of the histopathological diagnosis of certainty of dysplastic lesions, in the context of the increased incidence of cervical cancer in our country. Cervicovaginal cyto-tumor examination and colposcopic examination had a good correlation with the histopathological diagnosis of the biopsied cervical fragment in cases where they were concordant. In case of discordant cytological and colposcopic results, cervical biopsy with histopathological examination establishes the diagnosis of certainty. Since the incidence of cervical cancer is high in our country, the biopsy with histopathological examination is necessary to establish the diagnosis of dysplastic lesions and the subsequent therapeutic behavior.
Cytological, colposcopic and histopathological correlations in the diagnosis of cervical intraepithelial neoplasia
Corelaţii citologice, colposcopice şi histopatologice în diagnosticul neoplaziilor intraepiteliale cervicale
First published: 30 aprilie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.71.1.2023.8136
Abstract
Rezumat
Leziunile preinvazive cervicale au o perioadă lungă de evoluţie spre cancerul de col uterin, astfel încât depistarea precoce şi tratarea lor, alături de vaccinarea anti-HPV, reprezintă o necesitate în prevenţia apariţiei cancerului cervical invaziv. Infecţia genitală cu HPV este cea mai comună infecţie transmisă sexual. Obiectivul acestui studiu a fost stabilirea predicţiei examenului citotumoral cervicovaginal şi a examenului colposcopic pentru leziunile displazice cervicale şi examenul histopatologic al fragmentelor obţinute prin biopsie cervicală, precum şi reevaluarea diagnosticului histopatologic de certitudine al leziunilor displazice, în contextul incidenţei crescute a cancerului de col în ţara noastră. Examenul citotumoral cervicovaginal şi examenul colposcopic au avut o corelaţie bună cu diagnosticul histopatologic al fragmentului cervical biopsiat la cazurile în care au fost concordante. În situaţia discordanţei dintre rezultatele citologice şi colposcopice, biopsia cervicală cu examen histopatologic stabileşte diagnosticul de certitudine. Întrucât incidenţa cancerului de col uterin este mare în ţara noastră, efectuarea biopsiei cu examen histopatologic este necesară pentru stabilirea diagnosticului leziunilor displazice şi a conduitei terapeutice ulterioare.
Introduction
Preinvasive cervical lesions have a long period of evolution towards cervical cancer, therefore the early detection and treatment, along with anti-HPV vaccination, are a necessity in preventing the occurrence of invasive cervical cancer.
Cervical cancer ranks first among female genital cancers, being the second cause of death in our country, after malignant breast tumors(1). The insufficient addressability of women to cervical cyto-tumor screening is the main reason for this situation, therefore it is necessary to increase the educational and hygienic-sanitary level of the population. The reduction of risk factors, the prophylaxis through anti-HPV vaccination and Babeş-Papanicolau screening through early detection and monitoring of cervical cancer precursor lesions can reduce the incidence of cervical cancer in Romania(2-4).
Genital HPV infection is the most common sexually transmitted infection. The risk of genital HPV infection is 80% in women over 50 years old, the most common being in women under 25 years old(5,6). The main cause of cervical lesions is the persistent infection with the human papillomavirus. High-risk HPV strains are present in cervical intraepithelial neoplasia and invasive cervical cancer(7-9).
Worldwide, in countries with a low incidence of cervical cancer, the prevalence of chronic HPV infection is 5-10%. The prevalence of persistent HPV infection is 10-20% in countries with a high incidence of cervical cancer. Vaccination against HPV prevents infection with high-risk strains, leading to a decrease in the risk of cervical dysplasia and cervical cancer(10-12).
Cytological screening with the Babeş-Papanicolau test or in the Bethesda system together with viral genotyping for the detection of DNA-HPV with high oncogenic risk can detect high-grade lesions and cervical cancer(13-17). High-grade lesions (HSIL, ASC-H) have an increased risk of developing into an invasive cancer, and to prevent the worsening of the lesion, cytological and viral monitoring is necessary, with histological evaluation after cervical biopsy(8,18-20).
Inconclusive or abnormal cervical cytology requires colposcopic examination to visualize the squamocylindrical junction, the characteristics and extent of the lesions, targeted biopsy from the suspicious area, and endocervical curettage in the case of extensive lesions in the endocervical canal.
Biopsied tissue fragments are subjected to histopathological examination to establish a definitive diagnosis of cervical lesions. The histopathological examination establishes the presence of atypical cells that characterize cervical intraepithelial neoplasia (CIN), especially those with a high evolutionary risk.
The objective of the study was to establish the prediction of the cervicovaginal cyto-tumoral examination and the colposcopic examination for cervical dysplastic lesions, along with the histopathological examination of the fragments obtained by cervical biopsy, as well as the reevaluation of the histopathological diagnosis of certainty of dysplastic lesions, in the context of the increased incidence of cervical cancer in our country.
Materials and method
The study was carried out between January 2020 and December 2022 and included a group of 47 selected patients, aged between 22 and 62 years old. The patients underwent exfoliative cytology for cervical cyto-tumor examination, colposcopic examination and cervical biopsy with histopathological examination.
For the collection of exfoliative cytology, the patients kept sexual rest, did not use intravaginal tampons or local contraceptives, did not perform irrigation or intravaginal treatments 24-48 hours before the collection, and they were not examined by vaginal tact in the morning in which the sampling was performed. Cytology was collected from the level of the exocolus, the squamocylindrical junction and the endocolus. The results were interpreted according to the Bethesda classification, in parallel with the Babeş-Papanicolaou classification.
For the colposcopic examination, the following were needed: videocolposcope, transparent bivalve speculum, long tampon-holding forceps, sterile cotton swabs, sterile compresses, 3% aqueous acetic acid solution, and Lugol’s solution. The colposcopic examination included the examination of the exocolus, the accessible area of the cervical canal, the bottoms of the vaginal sac, the examination of the vagina and the vulva. Through simple direct colposcopy, the cervix was examined without prior preparation, dried with the help of cotton swabs. The Hinselmann test was performed by staining with 2-3% acetic acid, then the Lahm-Schiller test by staining the cervix and vagina with Lugol’s solution. The colposcopic examination was considered satisfactory if the entire cervical lesion and the entire transformation area were visualized. If these two conditions were not respected, the colposcopic examination was considered unsatisfactory. To quantify the results, regarding cervical intraepithelial neoplasia, the modified Reid Colposcopic Index was used, taking into account the classification of colposcopic images in grades updated by Coppleson(21). It was considered that the Reid score between 0 and 4 points corresponds to low-grade CIN, and the Reid index between 5 and 8 points corresponds to high-grade CIN, according to Richart’s intraepithelial neoplasia classification.
The histopathological diagnosis was established on the basis of tissue fragments obtained by cervical biopsy. The biopsy was performed primarily from the lesions with the most severe appearance, but also from the rest of the cervical lesions, even though the epithelium had apparently minor changes. Endocervical curettage was performed in cases where the endocervical canal was not visualized.
The results of the histopathological examination were compared with the results of the cytological examination and colposcopy to evaluate the degree of concordance, overestimation and underestimation of the cases.
Results
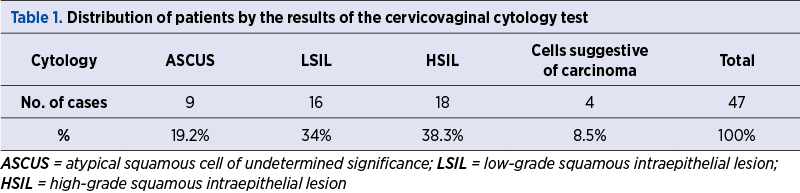
The results of the cytological examination were reported as positive for cellular abnormalities, as follows: ASCUS in nine cases (19.2%), LSIL in 16 cases (34%), HSIL in 18 cases (38.3%), cells suggestive of squamous neoplasia in four cases (8.5%) – Table 1 and Figure 1.
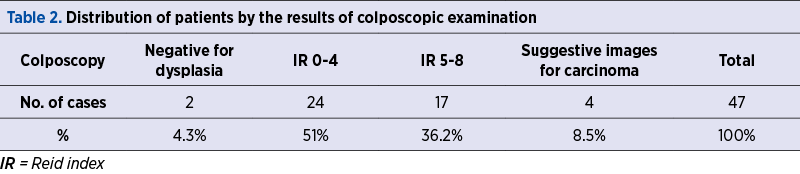
The colposcopic examination was negative for dysplasia in two cases (4.3%). The Reid score totaled between 0 and 4 points in 24 patients (51%), and between 5 and 8 points in 17 patients (36.2%). Images suggestive of squamous neoplasia were identified in three patients (8.5%) – Table 2 and Figure 2.
The histopathological examination on the fragments obtained by cervical biopsy were reported as follows: low-grade CIN in 23 patients (48.9%), high-grade CIN in 20 cases (42.6%), and squamous neoplasia in four cases (8.5%) – Table 3 and Figure 3.
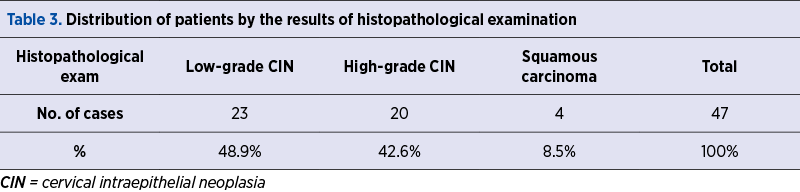
The histopathological examination of low-grade CIN in 23 patients (48.9%) was established in seven cases with ASCUS, 14 cases with LSIL, two cases with HSIL, and from the colposcopic point of view, two cases were negative for dysplasia. IR 0-4 was established in 17 cases, and IR was established 5-8 in four cases (Tables 4 and 5).
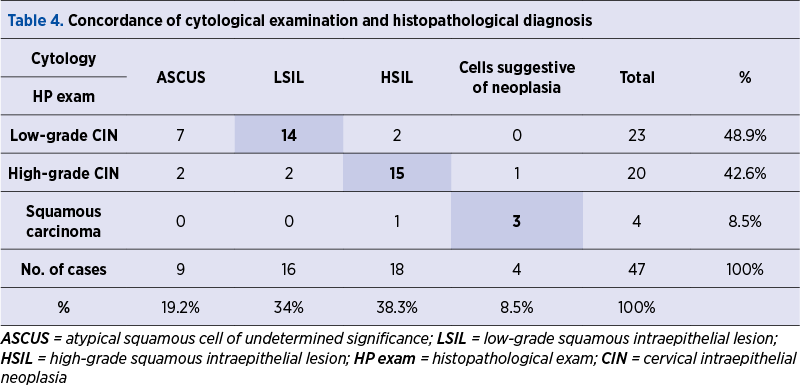
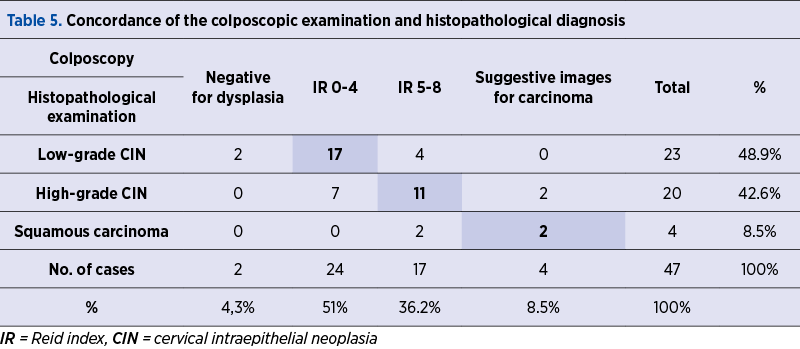
The histopathological examination of high-grade CIN in 20 patients (42.6%) was established in two cases with ASCUS, two cases with LSIL, 15 cases with HSIL, and one case with cells suggestive of squamous neoplasia. From the colposcopic point of view, there were seven cases with IR 0-4, 11 cases with IR 5-8, and two cases with images suggestive of squamous neoplasia (Tables 4 and 5).
The histopathological examination of squamous neoplasia in the four cases (8.5%) established histopathologically revealed three cases of cytology suggestive of squamous neoplasia and one case with HSIL, and from the colposcopic point of view, there were two cases with colposcopic changes suggestive of squamous neoplasia and two cases with IR 5-8 (Tables 4 and 5).
Discussion
The Babeş-Papanicolaou cervical cyto-tumor screening detects cell abnormalities early in most cases of cervical intraepithelial neoplasia or cancer in situ, the therapeutic behavior being optimal in these patients. The specificity of the test is approximately 98%, the sensitivity being lower and variable. Thus, it is necessary to periodically repeat the screening every three years, between 21 and 65 years old, even in asymptomatic patients(22,23). False-negative test results are caused by the incorrect sampling or non-identification of abnormal cervical cells.
It should be noted that, although atypical squamous cells were detected in nine cases (19.2%), their significance could not be precisely determined, and they were classified as ASCUS. For low-grade and high-grade intraepithelial neoplasia and squamous cancer, the prediction based on the cytological examination was consistent with the result of the histopathological examination in 32 cases (68%), in three cases (6.4%) it was overestimated, and in three cases (6.4%) it was underestimated (Figure 4).
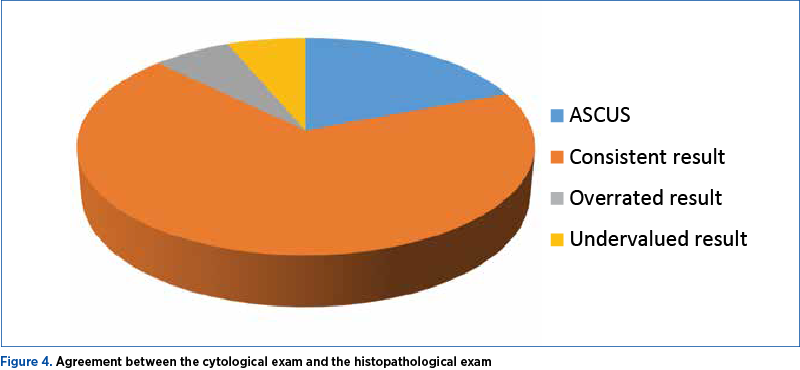
By analyzing the diagnostic groups, the best prediction was for high-grade CIN, which correlates best with the HSIL result (75%) – Figures 1 and 3. In cases of low-grade CIN, the correlation with the LSIL cytological result was 60.9%. Squamous cancer was correlated with the result of the cytological examination in a proportion of 75%.
These results confirm the data from specialized literature regarding the cervicovaginal cyto-tumor examination, which is a test with high sensitivity and specificity in detecting cervical intraepithelial neoplasia, but with low specificity in terms of predicting the degree of dysplasia.
Colposcopy is the best investigation for the visualization and biopsy of cervical lesions in patients with abnormal cytology. The sensitivity of the method in detecting high-grade cervical intraepithelial neoplasia is approximately 70%, which indicates cytological and colposcopic monitoring(24-26).
Analyzing the prediction based on the colposcopic examination, in the case of intraepithelial neoplastic lesions and squamous carcinoma, the histopathological result was concordant in 30 cases (63.8%), overestimated in six cases (12.8%), and underestimated in 11 cases (23.4%) – Figure 5.
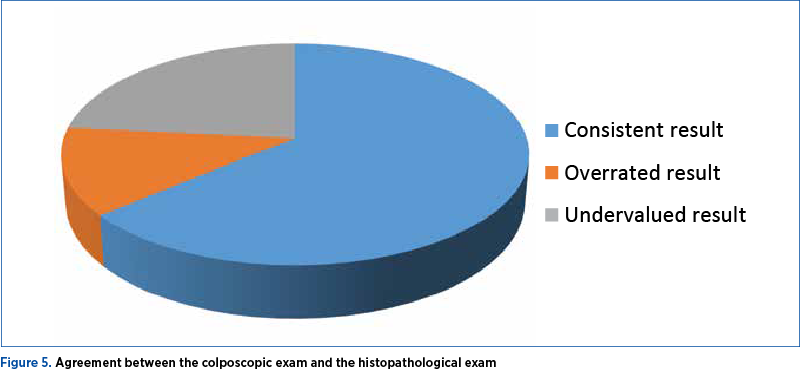
In cases of low-grade CIN, the degree of correlation with the colposcopic result IR 0-4 was the highest (73.9%), and in patients with high-grade CIN, the correlation with IR 5-8 was 55%. For patients with histopathologically confirmed squamous cell carcinoma, the correlation with colposcopic changes was 50% (Figures 2 and 3).
Colposcopy is a reliable investigational method, but with certain limits in the case of multiple or mixed cervical lesions where the basic aspects can be masked.
Precolposcopic biopsy identifies approximately 60-70% of high-grade lesions, therefore a larger number of biopsies is recommended, even from apparently normal epithelium(27,28).
Comparatively analyzing the levels of concordance with the histopathological diagnosis of the biopsied tissue fragments, by diagnostic group, we found that for low-grade neoplasms there is a percentage difference of 13% in favor of the colposcopic examination, while for high-grade neoplasias the percentage difference is 20% in favor of the cytological examination. For squamous cancer, the percentage difference of 25% is in favor of the cervicovaginal cyto-tumor examination.
Data interpretation must be done with caution, because part of the cervical biopsy indications are determined by the results of these two examinations, cyto-tumoral and colposcopic.
It is noteworthy that, although it is very suggestive for the diagnosis, the positive concordance of the two tests found in 27 patients represents 57.5% of the 47 cases detected with intraepithelial neoplasia or squamous cancer.
In a significant percentage (42.5%), the suspicion raised by one of the investigations and the attempt to elucidate the inconclusive cases contribute to the establishment of the final diagnosis.
Conclusions
Cervicovaginal cyto-tumor examination and colposcopic examination had a good correlation with the histopathological diagnosis of the biopsied cervical fragment in cases where they were concordant.
For low-grade CIN, high-grade CIN and squamous cancer, the prediction based on the cytological examination was consistent with the result of the histopathological examination in a large proportion; the best prediction was for high-grade CIN, which correlated best with HSIL, denoting a high sensitivity and specificity in detecting CIN, but a low specificity in predicting the degree of dysplasia.
Analyzing the prediction based on the colposcopic examination, in the case of CIN and squamous carcinoma, the histopathological result was consistent with the result of the colposcopic examination in a large proportion; in cases of low-grade CIN, the degree of correlation with the IR 0-4 colposcopic result was the highest.
In cases of discordant cytological and colposcopic results, cervical biopsy with histopathological examination establishes the diagnosis of certainty. Since the incidence of cervical cancer is high in our country, the biopsy with histopathological examination is necessary to establish the diagnosis of dysplastic lesions and the subsequent therapeutic behavior.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
National Center of Statistics in Public Health, Bucharest, 2021. https://insp.gov.ro/centrul-national-de-statistica-in-sanatate-publica-cnssp/.
-
Coravu V, Ţurcan G, Ţurcan N, Grădinaru-Fometescu D, Sajin M, Cîrstoiu MM. Analysis of the results of national screening programs for early active diagnosis of cervical cancer and proposal of improvement strategy. Ginecologia.ro. 2021;33(3):30-5.
-
Iancu FC. The awareness campaigns on cervical cancer prevention
-
and their effects in the female population of Bucharest. Ginecologia.ro. 2019;25(3):46-9.
-
Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Romania. Summary Report 2016-02-26. https://hpvcentre.net/statistics/reports/ROU_FS.pdf
-
Centers for Disease Control and Prevention: Sexually transmitted diseases treatment guidelaines 2002. MMWR. 2002;51(6):1.
-
Dunne EF, Unger ER, Sternberg M. Prevalence of HPV infection among females in the United States. JAMA. 2007;297(8):813-9.
-
Nagy V, Rancea AC, Peltecu G, Anghel R, Ghilezan N. Cancerul de col uterin: ghid de diagnostic şi tratament. Radioter Oncol Med. 2006;1:7-15.
-
American Cancer Society. Cancer facts & figures 2017. Atlanta (GA): ACS; 2017. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf. Retrieved February 22, 2017.
-
Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC, Thompson TD, et al. Human papillomavirus-associated cancers - United States, 2008–2012. MMWR. 2016;65:661–6.
-
Colombo N, Carinelli S, Colombo A, Marini C, Rollo D, Sessa C; on behalf of the ESMO Guidelines Working Group, Clinical Parctice Guidelines, Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(Suppl 7):vii27-vii32.
-
Bohîlţea RE, Grigoriu C, Gheorghe CM, Ducu I, Mihai B, Mitran M, Berceanu C, Vlădăreanu R. Update of international guidelines for cervical cancer screening. Ginecologia.ro. 2021;34(4):33-8.
-
ACOG. Committee Opinion No. 704: Human Papillomavirus Vaccination. Obstet Gynecol. 2017;129(6):1.
-
ACOG. Women’s Health Care Physicians. Cervical cancer screening guidelines. FAQ085, Sept 2017. https://www.acog.org/Patients/FAQs/Cervical-CancerScreening.
-
Screening for Cervical Cancer. US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674-86.
-
Ronco G, Dillner J, Elfström KM, Tunesi S, Snijders PJ, Arbyn M, et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383(9916):524–32.
-
Huh WK, Ault KA, Chelmow D. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Obstet Gynecol. 2015;125(2):330–7.
-
ACOG. Committee Opinion No. 624: Cervical cancer screening in low-resource settings. Obstet Gynecol. 2015;125(2):526–8.
-
Stewart Massad L, Einstein MH, Warner K. 2012 Updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 Suppl 1):S1-S27.
-
Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Screening for cervical cancer: US Preventive Services Task Force Recommendation Statement. US Preventive Services Task Force. JAMA. 2018;320(7):674–86.
-
ACOG Practice Bulletin No. 168. Cervical cancer screening and prevention. Obstet Gynecol. 2016;128(4):e111–e130.
-
Coppleson M, Dalrymple JC, Atkinson KH. Colposcopic differentiation of abnormalities arising in the transformation zone. Obstet Gynecol Clin North Am. 1993;20(1):83-110.
-
Bibbo M, Wilbur DC. Comprehensive cytopathology, 3th Ed., Saunders-Elsevier, 2008.
-
WHO. Screening and early detection of cancer. Cervical cancer screening. Cytology screening. 2010. http://www.who.int/cancer/detection/cytologyscreen/en/index.html. Accessed: December 27.
-
Cantor SB, Cardenas-Turanzas M, Cox DD. Accuracy of colposcopy in the diagnostic setting compared with the screening setting. Obstet Gynecol. 2008;111(1):7-14.
-
DeSantis T, Chakhtoura N, Twiggs L. Spectroscopic imaging as a triage test for cervical disease: a prospective multicenter clinical trial. J Low Genit Tract Dis. 2007;11(1):18-24.
-
Gage JC, Anson VW, Abbey K. Number of cervical biopsies and sensitivity of colposcopy. Obstet Gynecol. 2006;108(2):264-72.
-
Pretorius RG, Zhang WH, Belinson JL. Colposcopically directed biopsy, random cervical biopsy, and endocervical curettage in the diagnosis of cervical intraepithelial neoplasia II or worse. Am J Obstet Gynecol. 2004;191:430-4.
-
ACOG Practice Bulletin No. 99: Management of abnormal cervical cytology and histology. Obstet Gynecol. 2008;112(6):1419-44.