Endometrioma – the tip of the iceberg?
Endometriomul ovarian – vârful aisbergului?
Abstract
Endometriosis is a chronic disease that affects around 10% of women who are of reproductive age. It may lead to significant morbidity, and it is a serious public health concern. Ovarian lesions, such as endometriomas or traditional ovarian cysts, are the most common localizations of endometriosis. Transvaginal ultrasonography is the first-line imaging modality for predicting deeply infiltrating endometriosis and is a straightforward diagnostic technique with a good diagnostic accuracy for endometriomas. A total of 437 patients who underwent preoperative ultrasonography examination and underwent surgery for deeply infiltrating endometriosis were included in our retrospective observational study. Of these, 45.2% (152 patients) had an endometriosis cyst diagnosis alone, with no further deep endometriosis lesions detected by ultrasonography; nevertheless, a number of patients had numerous deeply infiltrating lesions diagnosed intraoperatively. The objective of the present research was to evaluate the correlation between the sonographic identification of ovarian endometriomas and the detection of particular extraovarian endometriotic lesions, such as parametrial, rectovaginal and intestinal lesions, using transvaginal ultrasound.Keywords
transvaginal ultrasounddeeply infiltrating endometriosisfirst-line diagnosticRezumat
Endometrioza este o boală cronică ce afectează aproximativ 10% dintre femeile aflate la vârsta reproductivă. Poate conduce la morbiditate importantă şi reprezintă o problemă semnificativă de sănătate publică. Localizările cele mai frecvente sunt reprezentate de leziunile ovariene, care se manifestă sub formă de endometrioame ovariene. Ecografia transvaginală este modalitatea imagistică de primă linie pentru diagnosticarea endometriozei infiltrante profunde şi este o tehnică simplă, cu o bună acurateţe a diagnosticului pentru endometrioame. Studiul nostru este o analiză observaţională retrospectivă în care au fost incluse 437 de paciente care au avut o intervenţie chirurgicală pentru endometrioză infiltrativă profundă după evaluarea ecografică preoperatorie. 152 de paciente, reprezentând 45,2%, au avut un diagnostic de chist (sau chisturi) endometriozice, fără a avea asociate leziuni suplimentare de endometrioză profundă diagnosticate ecografic. Cu toate acestea, în cadrul intervenţiei chirurgicale minim invazive, un număr semnificativ de paciente au fost diagnosticate cu leziuni de endometrioză profund infiltrativă. Obiectivul acestui studiu a fost de a evalua corelaţia dintre identificarea ecografică a endometriomului ovarian şi detectarea anumitor leziuni endometriozice extraovariene, cum ar fi leziunile parametriale, rectovaginale şi intestinale, folosind ecografia transvaginală.Cuvinte Cheie
ecografie transvaginalăendometrioză profund infiltrativădiagnostic de primă linieIntroduction
About 10% of women of reproductive age have endometriosis, a chronic illness that may cause serious morbidity, being ultimately a major public health problem(1). One type of endometriosis, known as deeply infiltrating endometriosis (DIE), occurs when the disease extends more than 5 mm below the peritoneal surface(2). Histologically, endometriosis is classified into three forms: ovarian endometrioma, deeply infiltrating endometriosis, and peritoneal superficial endometriosis(3). Endometriosis associates infertility and varying degrees of pelvic pain(3). While, ideally, laparoscopy is the gold standard for diagnosing endometriosis in women with chronic pelvic pain based on visual inspection of the pelvis, a number of authors have shown that imaging evaluation can be used to map the disease before surgery, particularly in cases of ovarian endometriomas and deep infiltrative endometriosis(4). The most common localizations are represented by ovarian lesions, which appear as traditional ovarian cysts called endometriomas(2). Transvaginal ultrasonography (TVS) is a simple diagnostic tool for endometriomas with a high diagnostic accuracy and is the first-line imaging modality for predicting deep infiltrating endometriosis and endometriosis-related pelvic adhesions, such as ovarian fixation and pouch of Douglas obliteration(5,6).
Research has demonstrated a substantial correlation between DIE, pelvic adhesions and endometriomas(7). Furthermore, the stage of endometriotic disease is known to have an impact on infertility, in addition to the existence of endometrioma(7). TVS may be used to stage endometriosis prior to surgery, which means that this imaging modality can help with both surgical planning and fertility counseling for women who have endometriomas(8). Undiagnosed DIE associated with endometriomas is one of the main causes of incomplete surgical excision due to various factors, such as the experience of the surgeon and the lack of a multidisciplinary team(7). To decide on the best course of action – surgery or medication – patients should be transferred to tertiary centers with accurate TVS findings and a thorough ultrasonographic mapping of their lesions(9). The underestimate or misinterpretation of severe adhesions and DIE may lead to inadequate care, particularly in women who are infertile(10). In this case, the diagnosis may be done too late, after multiple attempts of assisted reproductive technologies (ART), which might result in repeated unsuccessful in vitro fertilization (IVF) cycles(11).
The objective of this research was to evaluate the correlation between the sonographic identification of ovarian endometrioma and the detection of particular extraovarian endometriotic lesions, such as parametrial, rectovaginal and intestinal lesions, using transvaginal ultrasound.
Materials and method
A total of 437 patients diagnosed with endometriosis were included in our retrospective, observational study, in which we included the patients who were evaluated preoperatively by ultrasound and then went through a minimally invasive surgical intervention (laparoscopically/robotical) between January 2020 and December 2022. Most of the patients presented for dysmenorrhea, dyspareunia and/or infertility. The patients were operated by the same surgeon at the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology and Memorial Hospital from Bucharest, Romania. The research received approval from the institutional review board of both institutions, and a comprehensive ethical evaluation was not necessary, due to the retrospective and observational design of the study. We included all patients who were diagnosed by transvaginal ultrasound with an endometriotic cyst (endometrioma) with more than 30 mm diameter and/or deep infiltrating endometriotic lesions.
Results
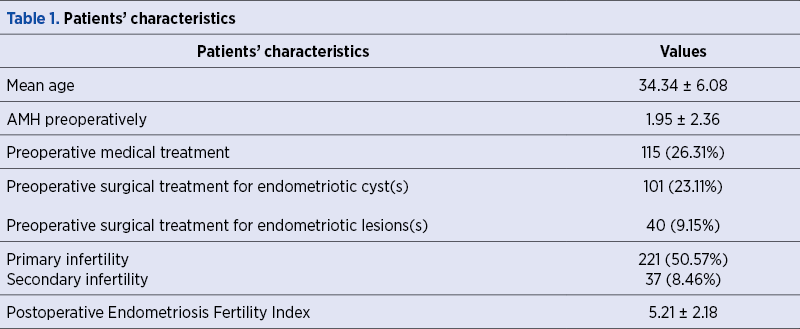
Following the investigation of the 437 patients included in our study, we have seen that the mean age of the cohort was 34.34 years old (Table 1). Out of the 437 patients, 336 (76.88%) were found to have either single or bilateral endometriotic cysts after transvaginal ultrasound evaluation. Additionally, 226 patients (51.71%) were diagnosed with one or more deep infiltrating endometriosis nodules through ultrasound examination. It is worth noting that 162 patients had both endometriotic cyst(s) and deep infiltrating endometriosis nodules. Among them, 59.03% were affected by primary or secondary infertility, with an average anti-Müllerian hormone (AMH) level of 1.95 ng/mL (Table 1). Additional characteristics of the patients are included in Table 1.
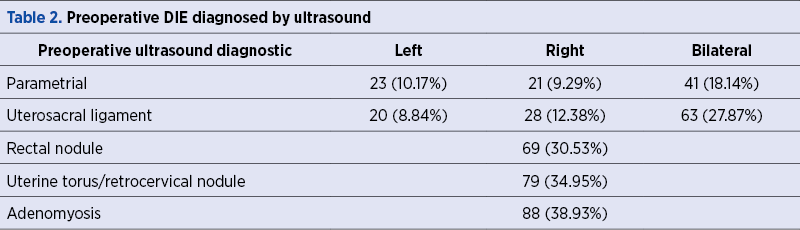
The assessment by TVS showed deep infiltrating endometriotic nodules in 51.71% of patients in addition to ovarian endometriomas. As seen in Table 2, deep infiltrating rectosigmoid endometriosis, adenomyosis and DIE at the level of parameters, uterosacral ligaments and torus uterinus were also found in these patients.
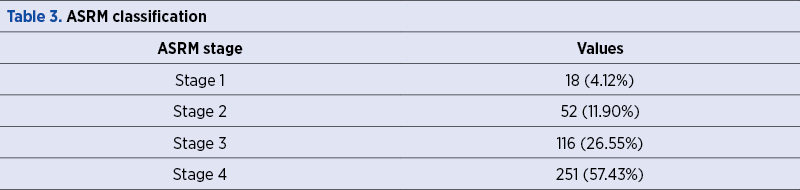
Subsequently, all the patients underwent a laparoscopic or robotic surgical procedure. During this procedure, unilateral or bilateral cystectomy was performed, along with complete removal of deep endometriosis lesions. In some cases, rectosigmoid resection or rectal shaving was performed to remove rectosigmoid endometriosis. Postoperatively, both American Society for Reproductive Medicine (ASRM) staging and #ENZIAN staging were used, and we note that most patients were classified as ASRM stage IV (57.43%) – Table 3.
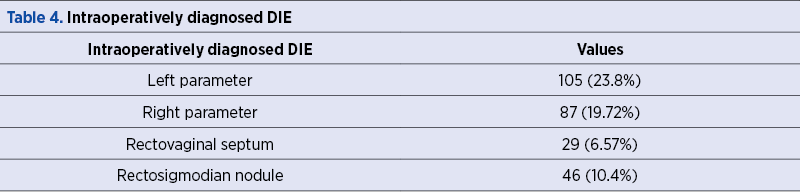
Among the patients who were diagnosed with an endometriotic cyst, 45.2% of the patients (152) assessed by ultrasonography had a diagnosis of endometriosis cyst(s) alone and no other deep endometriosis lesions diagnosed preoperatively. As it can be seen in Table 4, these patients had deep endometriosis lesions discovered during the procedure at several locations, including the parameter level, the rectovaginal septum and, also, rectosigmoid endometriotic nodule.
Postoperatively, the evolution of the patients was favorable. We had no recurrence and no intraoperative complications. There were no postoperative complications and no conversion to laparotomy. The histopathologic exam confirmed in all cases that the excised lesions were endometriotic.
Discussion
As it was shown, ovarian endometriomas and deep endometriosis lesions are frequently discovered during transvaginal ultrasound assessment. In certain cases, deep endometriosis lesions that were not visible before surgery were discovered during the surgical procedure, when endometriosis cysts were the only visible lesions by ultrasound. The question therefore arises: is ovarian endometrioma only the tip of the iceberg for deep endometriosis lesions at the peritoneal or even intestinal level, which are often hidden?
Previous research has shown that an ovarian endometrioma is a predictor for the severity of the disease in women with deeply infiltrating endometriosis(7). On the contrary, few studies have been conducted regarding the distribution patterns of DIE lesions in patients with ovarian endometriomas. As these lesions are often symptomatic and indicator of a more multifocal and severe illness, the current research examined lesion distribution features in women diagnosed preoperatively with ovarian endometriosis alone, with no other ultrasonographic sign of ultrasound and DIE discovered intraoperatively.
If surgery is chosen, the complete excising of all of the DIE lesions is the only method to provide a meaningful improvement in the painful symptoms(12). Moreover, the DIE lesions are more severe when an endometrioma is present(7). While it is true that there is no substantial correlation between the existence of an endometrioma and the infiltration of the uterosacral ligaments, this is not the case for the other posterior DIE lesions like vaginal, ureteral or intestinal deeply infiltrating endometriosis, where literature shows such a correlation(13). Complete excision of the DIE lesions of the rectosigmoid require complex surgical techniques, which carry a significant risk of complications(13,14).
The literature indicates that between 5% and 12% of women with endometriosis have intestinal endometriosis(15). Otherwise, intestinal endometriosis that was associated with ovarian endometrioma accounted for 10.4% of cases in our study, similar to the frequency seen in other studies(15). Kondo stated that intestinal DIE and DIE lesions were more strongly associated with women who presented ovarian endometriosis(16).
The results of this study highlight the need of precise mapping of the pelvic locations and precise transvaginal ultrasound examination. Furthermore, it is imperative that every woman diagnosed with an endometrioma get a thorough transvaginal ultrasound examination. When surgery is planned, the use of ultrasound staging may help ensure that women are appropriately sent to an advanced laparoscopic surgeon(17). A complete and correct surgical intervention may reduce the painful symptoms, but it may also enhance the reproductive results, which is important, because more than 50% of the women were impacted by infertility, as revealed by our study.
Conclusions
To assist in the identification and mapping of endometriotic lesions and/or pelvic adhesions, a transvaginal ultrasound should be carried out in all women with infertility, pelvic discomfort and/or suspicion of endometriosis. Preoperative transvaginal ultrasound is crucial for women with endometriomas in order to anticipate the difficulty of the surgery during a laparoscopy, as well as for staging the disease severity.
The results of this study, along with the aforementioned ones, enable us to draw the conclusion that, in cases of ovarian endometrioma, a specialist should perform appropriate preoperative mapping for deeply infiltrating endometriotic lesions in order to diagnose all the existing lesions. Surgical procedures are often complicated and require the total removal of all endometriotic lesions. A multidisciplinary team that is specialized in the treatment of deeply infiltrating endometriosis must perform the surgical treatment.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.
Bibliografie
- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98(3):511-519.
- Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10(5):261-275.
- Koninckx PR, Meuleman C, Demeyere S, Lesaffre E, Cornillie FJ. Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil Steril. 1991;55(4):759-765.
- Piketty M, Chopin N, Dousset B, et al. Preoperative work-up for patients with deeply infiltrating endometriosis: transvaginal ultrasonography must definitely be the first-line imaging examination. Hum Reprod. 2009;24(3):602-607.
- Guerriero S, Condous G, van den Bosch T, et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: a consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet Gynecol. 2016;48(3):318-332.
- Reid S, Lu C, Casikar I, et al. Prediction of pouch of Douglas obliteration in women with suspected endometriosis using a new real-time dynamic transvaginal ultrasound technique: the sliding sign. Ultrasound Obstet Gynecol. 2013;41(6):685-691.
- Chapron C, Pietin-Vialle C, Borghese B, Davy C, Foulot H, Chopin N. Associated ovarian endometrioma is a marker for greater severity of deeply infiltrating endometriosis. Fertil Steril. 2009;92(2):453-457.
- Exacoustos C, Zupi E, Carusotti C, et al. Staging of pelvic endometriosis: role of sonographic appearance in determining extension of disease and modulating surgical approach. J Am Assoc Gynecol Laparosc. 2003;10(3):378-382.
- Menakaya U, Reid S, Lu C, Gerges B, Infante F, Condous G. Performance of ultrasound-based endometriosis staging system (UBESS) for predicting level of complexity of laparoscopic surgery for endometriosis [published correction appears in Ultrasound Obstet Gynecol. 2017 May;49(5):667]. Ultrasound Obstet Gynecol. 2016;48(6):786-795.
- Hudelist G, Keckstein J. Die Wertigkeit der Vaginalsonographie in der präoperativen Diagnostik der Adenomyose und tief infiltrierenden Endometriose [The use of transvaginal sonography (TVS) for preoperative diagnosis of pelvic endometriosis]. Praxis (Bern 1994). 2009;98(11):603-607.
- Opøien HK, Fedorcsak P, Omland AK, et al. In vitro fertilization is a successful treatment in endometriosis-associated infertility. Fertil Steril. 2012;97(4):912-918.
- Chapron C, Fauconnier A, Vieira M, et al. Anatomical distribution of deeply infiltrating endometriosis: surgical implications and proposition for a classification. Hum Reprod. 2003;18(1):157-161.
- Remorgida V, Ferrero S, Fulcheri E, Ragni N, Martin DC. Bowel endometriosis: presentation, diagnosis, and treatment. Obstet Gynecol Surv. 2007;62(7):461-470.
- Chopin N, Vieira M, Borghese B, et al. Operative management of deeply infiltrating endometriosis: results on pelvic pain symptoms according to a surgical classification. J Minim Invasive Gynecol. 2005;12(2):106-112.
- Sznurkowski J, Emerich J. Czestsza lewostronna lokalizacja torbieli endometrialnych [Left lateral predisposition of endometrioma]. Ginekol Pol. 2005;76(1):33-36.
- Kondo W, Ribeiro R, Trippia CH, Zomer MT. Associação entre endometrioma ovariano e endometriose profunda infiltrativa [Association between ovarian endometrioma and deep infiltrating endometriosis]. Rev Bras Ginecol Obstet. 2012;34(9):420-424.
- Cranney R, Condous G, Reid S. An update on the diagnosis, surgical management, and fertility outcomes for women with endometrioma. Acta Obstet Gynecol Scand. 2017;96(6):633-643




