Introduction. Stress urinary incontinence (SUI) impacts over 20% of women, and its prevalence is increasing with the aging of population. This review assesses mesh surgery for SUI treatment by analyzing midurethral slings, retropubic urethropexy, bulking agents and artificial sphincters. Methodology. We searched the PubMed database from 1995 to 2023 inclusive, and 31 studies met our inclusion criteria, focusing on women aged 20-70 years old with SUI, excluding nervous system diseases affecting the function of the bladder. Results. Minimally invasive midurethral slings – particularly transvaginal tension-free tape (TVT) and transobturator tension-free vaginal tape (TOT) – have become the standard of care, endorsed by the Food and Drug Administration (FDA) in 2011. TVT offers reduced hospital stays and shorter operating times, with risks including bladder perforation and infections. TOT, while minimizing bladder perforation risks, may increase groin pain. Mini-slings and autologous fascial slings show varying success; the latter has higher success but more complications than Burch colposuspension. Retropubic urethropexy is effective on the long term, but with longer recovery and more complications. Conclusions. Mesh-based midurethral slings (MUS) are pivotal in SUI treatment, providing high short-term success and enhanced quality of life. Effective SUI management requires individualized treatment, with a fine balance between benefits and risks. With emerging regenerative medicine, the future of SUI treatment is promising. Until then, MUS remains a key modality, necessitating careful patient selection and ongoing research to refine the surgical outcomes and improve the quality of life for SUI patients.
Is the mesh necessary for the treatment of female urinary stress incontinence?
Sunt meşele necesare în tratamentul incontinenţei urinare de efort la femei?
First published: 30 iunie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.71.2.2023.8871
Abstract
Rezumat
Introducere. Incontinenţa urinară de efort (IUE) afectează peste 20% dintre femei, iar prevalenţa sa este în creştere, odată cu îmbătrânirea populaţiei. Acest studiu evaluează chirurgia cu meşe de polipropilenă în comparaţie cu alte tratamente pentru IUE, luând în considerare bandeleta suburetrală, uretropexia retropubiană, agenţii de îngroşare uretrală şi sfincterele artificiale. Metodologie. Prin căutarea în baza de date PubMed din aprilie 1995 până în august 2023, un număr de 31 de studii au îndeplinit criteriile noastre de includere. Studiul a inclus paciente cu IUE cu vârsta între 20 şi 70 de ani, fiind excluse bolile sistemului nervos care afectează funcţia vezicii urinare. Rezultate. Tehnicile chirurgicale minim invazive – în special cele cu meşă vaginală fără tensiune (TVT) şi meşă transobturatorie (TOT) – au devenit standardul de îngrijire, avizat de Administraţia SUA pentru Alimente şi Medicamente (FDA) în 2011. TVT oferă reducerea zilelor de spitalizare şi un timp operator mai scurt, având în schimb riscuri precum perforaţia vezicii şi infecţii. TOT minimizează riscul de perforaţie a vezicii, dar poate mări riscul de apariţie a durerii inghinale. Minibandeletele şi sfincterele fasciale autologe au un succes variabil; ultimele au rate ridicate de succes, dar mai multe complicaţii decât colposuspensia Burch. Uretropexia retropubiană este eficientă pe termen lung, dar cu recuperare mai lungă şi cu mai multe complicaţii. Concluzii. Bandeletele suburetrale sunt esenţiale în tratamentul IUE, oferind rate ridicate de succes şi o calitate îmbunătăţită a vieţii. Managementul eficient al IUE necesită un tratament individualizat, care să menţină un echilibru între beneficiile şi riscurile intervenţiei. Cu apariţia medicinei regenerative, viitorul tratamentului IUE arată promiţător. Până atunci, bandeletele suburetrale rămân tratamentul de elecţie al IUE, dar necesită o selecţie atentă a pacientelor şi cercetări continue pentru a îmbunătăţi calitatea vieţii acestor paciente.
Introduction
The International Continence Society (ICS) defines stress urinary incontinence (SUI) as ‘‘the complaint of involuntary leakage on effort or exertion, or on sneezing or coughing’’, which can significantly impair the quality of life(1). SUI impacts over 20% of the female population, and its prevalence is on the rise as the population ages, posing a substantial burden on the affected individuals(2,3).
Corrective surgeries for SUI can be categorized into four main groups: 1) midurethral slings; 2) retropubic urethropexy; 3) urethral bulking agents; 4) artificial sphincters.
Traditionally, the Burch urethropexy, an abdominal surgical procedure involving the suspension of periurethral vaginal tissue to the Cooper ligament (pectineal ligament) bilaterally, has held a prominent position as the gold standard operation(4). This procedure has gained recognition due to its remarkable efficacy in addressing SUI, with reported overall cure rates ranging from 68.9% to 88.9%(4-6).
However, over the past decade, there have been advancements in minimally invasive midurethral sling (MUS) procedures for the treatment of SUI. In 1996, Ulmsten introduced the tension-free vaginal tape (TVT) procedure, which initially showed an 84% cure rate at the two-year follow-up(7). In 2001, Delorme described a new method of inserting the tape which involves passing it through the obturator foramen – transobturator tape (TOT)(8).
Both of these procedures aim to recreate the natural suspension of the urethral fascia by utilizing a polypropylene mesh. The primary distinction between the two techniques lies in how the mesh is placed. Since its introduction in 1996, the midurethral sling has emerged as the new standard in incontinence surgery. This vaginal procedure has gained prominence and has achieved standard of care status, because it offers a higher level of efficacy in comparison to the Burch urethropexy, while being less invasive(9).
In this study we aim to provide a comprehensive review of mesh surgery in comparison to other surgical treatments in the management of SUI.
Methodology
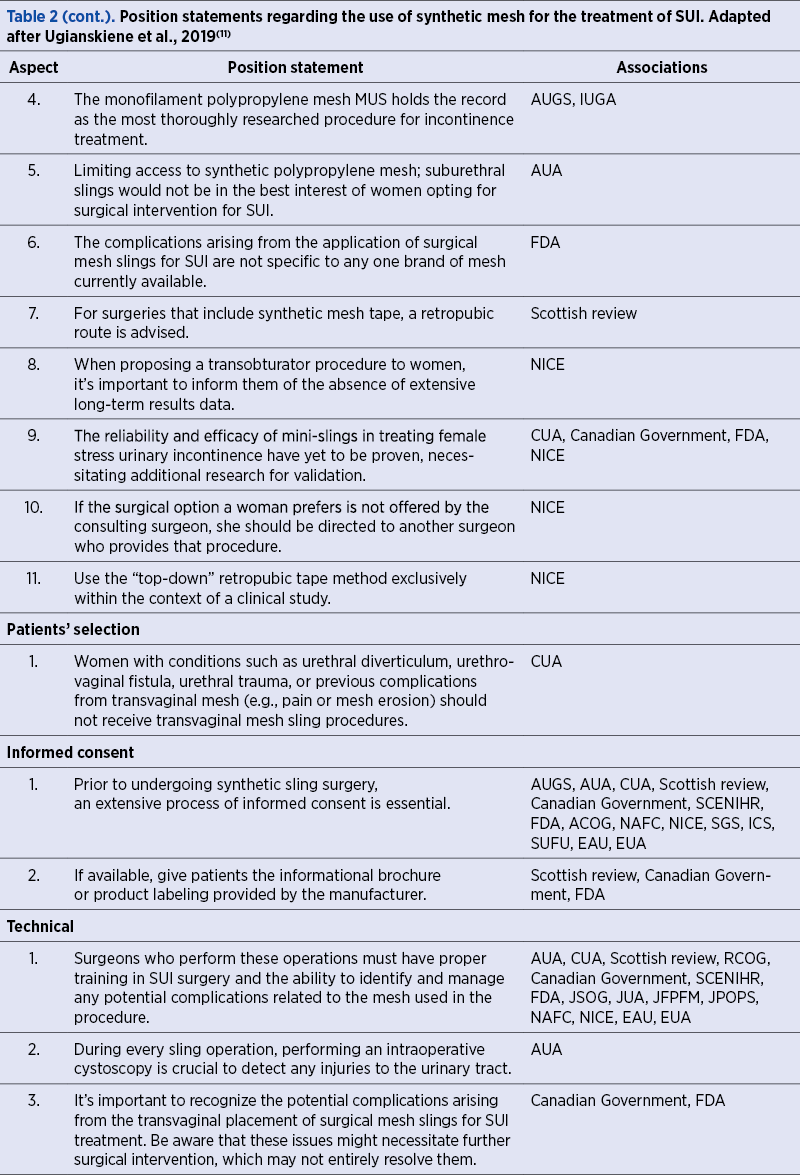
We conducted a literature search through the PubMed database from 1995 to 2023 inclusive, using the following keywords: “stress urinary incontinence”, “transobturator tape”, “continence surgery”, “midurethral sling”, “Burch urethropexy”. We included 31 systematic reviews and meta-analyses, randomized controlled trials (RCTs) and cohort studies in our data synthesis. The inclusion criteria consisted of: female gender, age 20-70 years old, SUI>1 time per week, lack of nervous system affecting the function of the bladder, patients treated with either sling procedures or Burch procedure. We took into consideration the procedure efficacy, the functional results, the patients’ satisfaction, outcomes and follow-up complications. Studies solely addressing the management of complications arising from the use of mesh were excluded. The exclusion criteria consisted of: male gender and diseases of the nervous system affecting the function of the bladder.
Results
A total of 31 studies fulfilled the inclusion criteria. Sling procedures for the management of urinary incontinence can be categorized into several types, including midurethral slings, transobturator tension-free vaginal tape (TOT), and single-incision mini-slings(10,29). Historically, slings were initially developed using either autologous muscle or fascia tissue(26). These slings were positioned at the junction between the urethra and bladder, and secured to either the rectus fascia or Cooper’s ligament(26). While these early slings were effective, they came with significant drawbacks in terms of patient morbidity. Patients who underwent these procedures often experienced complications such as hematomas and hernias at the tissue harvest site(10,26,29).
However, with the introduction of minimally invasive tension-free vaginal tape (TVT and TOT), the landscape of sling procedures evolved significantly(10,13).
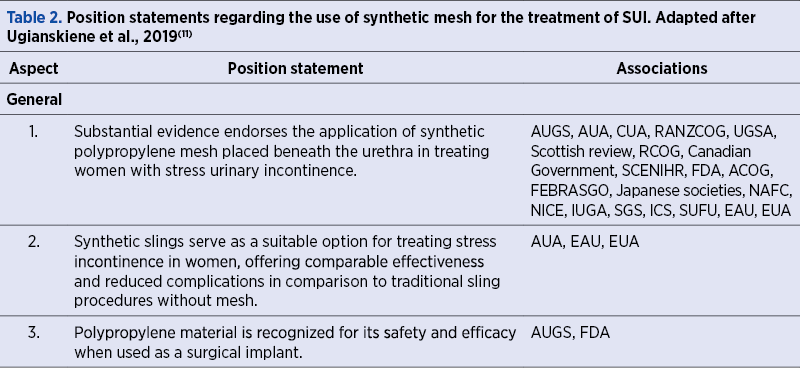
Minimally invasive midurethral slings, including retropubic and transobturator options, have become the predominant surgical choice for SUI(13). Synthetic polypropylene suburethral mesh is extensively supported for the treatment of female SUI by various medical associations and it has been established as safe and effective by the Food and Drug Administration (FDA) in 2011(10).
TVT sling is considered the standard of care for SUI treatment, offering advantages like minimally invasive, vaginal approach, shorter operating time and reduced hospital stay(12-14,21). Complications can include bladder perforation, mesh erosion, voiding problem and urinary tract infections(13). Long-term studies show its safety and effectiveness even after 11 years(20).
However, the TOT technique was introduced to reduce complications associated with the retropubic approach. TOT has a low incidence of bladder perforation, but it can cause higher rates of groin pain(16). Short-term and long-term subjective cure rates are comparable to those of retropubic slings(16,30).
Mini-slings aim to minimize vaginal dissection and reduce operative time. Outcomes vary, with some reports of lower subjective and objective cure rates compared to other slings(24). More long-term data are needed to assess their long-term efficacy(24).
Autologous fascial slings show higher success rates compared to Burch colposuspension at 24 months of follow-up, but with more complications, such as urinary tract infections and de novo urge incontinence(26).
Retropubic urethropexy is effective for treating SUI in the long term; however, it is associated with longer operating times, wound infections and hematoma formation(13).
In a comparison study, MUS procedures were more likely to be rated as very successful by patients and were associated with higher satisfaction rates compared to Burch retropubic urethropexy(28). No significant difference in patient global impression of severity, symptom improvement, complication rates or mesh exposures was found(28).
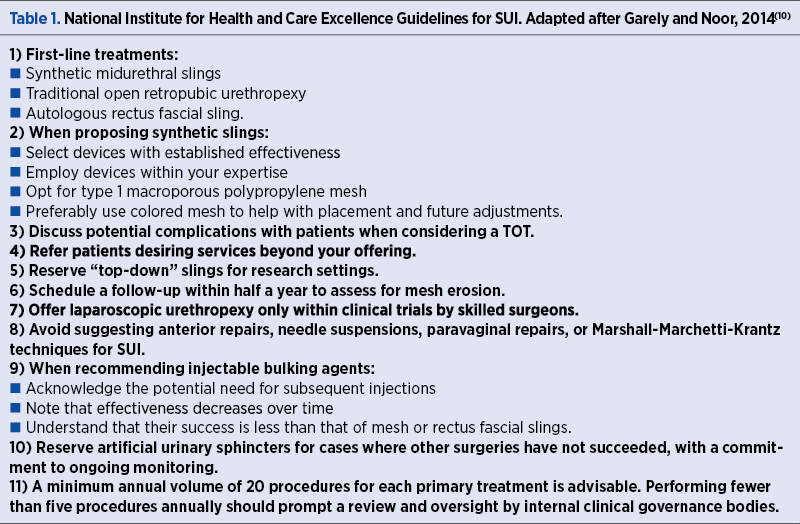
These results provide a comprehensive overview of the various surgical options for treating SUI, their effectiveness and associated complications. They highlight the importance of patient selection and informed consent when choosing the most suitable surgical approach for each individual (Table 1).
Surgical options for SUI
The surgical treatments for SUI can be categorized into four main groups: suburethral slings, retropubic urethropexy, bulking agents and artificial urinary sphincter devices(29). Periurethral bulking agent injections are typically considered for patients who may not be suitable candidates for surgical procedures or have previously undergone surgery with insufficient improvement in SUI symptoms(29). Artificial sphincters are considered a final option and are only used when previous surgical interventions have not yielded the desired results(29).
1. Midurethral slings (MUS)
A sling serves as a supportive hammock positioned under the urethra, with the purpose of enhancing urethral resistance during physical activities(10,27). Typically, slings are crafted from a synthetic polypropylene mesh strip, often referred to as suburethral tape(17). These slings come in various types, including pubovaginal slings located at the urethrovesical junction, MUS (either retropubic or transobturator), and single-incision slings (mini-slings)(27). Currently, midurethral slings have become the predominant surgical option for managing incontinence(27). Complications related to mesh, which are commonly associated with mesh kits used in prolapse surgeries, are not frequently encountered with mesh slings(27). In 2011, the FDA established the safety and effectiveness of mesh slings(10).
1.1. Tension-free vaginal tape sling (retropubic slings)
The FDA granted approval for the use of TVT in the United States of America in 1998(7,12). Since its introduction, it has revolutionized the treatment approach for patients with SUI and it has been considered the standard of care for SUI treatment(21,26). TVT offers several advantages, including its minimally invasive vaginal approach, shorter operating time and reduced hospital stay(21). The available data strongly support the long-term and short-term success of these slings(20). TVT, like all commercially available midurethral slings, is composed of macroporous monofilament (type 1) polypropylene mesh(21).
The procedure involves the insertion of two trocars through the retropubic space, either from a suburethral incision in the vagina to the suprapubic region or from the suprapubic region to the vagina using a top-to-bottom approach(27). During and after the operation, various complications can arise, necessitating prompt identification and appropriate management(12). Common complications include bladder perforation, while more severe complications encompass vascular injuries, injuries to pelvic organs, hemorrhage, mesh erosion or exposure, the onset of urgency and urge incontinence, bladder outlet obstruction, voiding problems and urinary tract infections(12). Reported figures in the literature indicate a prevalence of bladder perforation ranging from 3% to 5%, mesh erosion or exposure after TVT ranging from 1% to 3%, and voiding dysfunction ranging from 2.1% to 3.4%(13,14).
When comparing outcomes between the two surgical approaches, bottom-to-top and top-to-bottom for retropubic sling placement, there were no significant differences in objective cure rates (measured by pad weight) and subjective outcomes (measured by incontinence impact questionnaires)(15). Specifically, there was no statistically significant difference in terms of objective cure rates (83% versus 95%; p≤0.1%) or subjective outcomes (49.9±25.6 versus 45.3±18.4; p=0.46) between the two surgical approaches(15). Furthermore, when comparing adverse events and perioperative complications between these two approaches, there were no statistically significant differences(15). Fewer women experienced bladder perforation, voiding dysfunction, tape erosion and exposure when a bottom-to-top approach was employed(16).
1.2. Transobturator tension-free vaginal tape sling
Another approach to MUS is the transobturator technique(8). The retropubic approach, which involves the relatively blind passage of the trocar through the retropubic space, can sometimes lead to unintended complications like bladder perforations, vascular injuries and bowel injuries(13,14). To reduce these risks, Delorme introduced the transobturator technique in 2001(8).
In the transobturator technique (TOT), particularly designed trocars can be passed through two different routes: either from the inner groin to the vaginal incision (outside-in) or from the vaginal incision to the inner groin (inside-out)(18). The TOT approach has gained popularity, particularly among gynecologists, due to its ability to reduce the risk of bladder, vascular and bowel injuries(18). The incidence of bladder perforation with TOT is as low as 0.3% and there is a reduced occurrence of hematomas and voiding dysfunction(17). The primary complication associated with the transobturator approach is groin pain, which occurs at a rate between 10% and 15%, primarily with the inside-out approach(18).
Postoperatively, there were no noteworthy distinctions in the incidence of de novo urgency or voiding difficulties between the two approaches(18). In a randomized controlled trial, no outcome differences were observed, but the outside-in technique was associated with more vaginal sulcus tears, while the inside-out technique resulted in fewer vaginal fornix injuries but in a higher rate of postoperative groin pain(18-20,30). Concisely, either inside-out or outside-in techniques are adequate treatment options(27).
In a Cochrane review that examined randomized controlled trials comparing the retropubic and transobturator routes, which encompassed 36 trials involving a total of 5.514 subjects, there were no statistically significant differences in the short-term (12-36 months) subjective cure rates between the two groups(16). The short-term cure rates ranged from 62% to 98% for the transobturator route and from 71% to 97% for the retropubic route, with the mean short-term subjective cure rate across both groups being 83.3%(16). For long-term results after five years, four trials involving 714 women reported subjective cure rates which ranged from 43% to 92% in the transobturator group and from 51% to 88% in the retropubic group(16). There was no statistical difference between the two groups, with the mean long-term subjective cure rates in both groups being 84.3%(16). When assessing objective cure rates in both the short and long term, as measured by pad weights, urodynamics and cough stress tests, there were no differences between the two approaches(16). The cure rate for the obturator approach was 85.7%, compared to 87.2% for the retropubic route(16).
Long-term follow-up studies of TVT have indicated that midurethral slings remain safe and effective even after 11 years since placement, with a cohort showing a 77% subjective cure rate and 90% objective cure rate(20).
In a meta-analysis published in the Cochrane Library in 2009, which included 62 randomized studies involving 7101 women, when comparing TVT to Burch procedures, there was no significant difference in objective cure rates(22). However, when MUS (TVT and TOT) were compared to Burch procedures, lower rates of adverse events, such as blood loss, pain, time under anesthesia, hospital stay, infection, hematoma and bowel injuries, were noted(22). In terms of subjective cure, when all slings (TVT and TOT) were included, the combined odds ratio (OR) showed no significant difference but favored slings over the Burch procedure(21,28). The Burch procedure leads to lower rates of reoperation for issues like erosion, bladder outlet obstruction, overactive bladder symptoms and groin pain, because it doesn’t involve the use of mesh(22). Studies comparing retropubic slings with open Burch colposuspension have demonstrated similar cure rates between open Burch colposuspension and TVT(22,23). Evidence from 20 trials comparing open Burch colposuspension with MUS (TVT or TOT) found no significant difference in incontinence rates(22).
1.3. Single-incision slings (mini-slings)
Single-incision or mini-slings were developed with the aim of minimizing vaginal dissection, reducing the need for additional suprapubic or groin incisions and shortening operative time(24). These slings are typically anchored into the obturator internus fascia or the connective tissue of the endopelvic fascia in the retropubic space behind the pubic bone, depending on the chosen approach(24). Complications associated with single-incision slings are similar to those observed with full-length slings (retropubic or transobturator slings)(27).
When compared to transobturator and retropubic slings, the outcomes of mini-slings have been reported to exhibit more variability(24). Their cure rates are generally comparable, although some evidence shows that MUS might be superior to mini-slings(21,24,27). However, in a meta-analysis involving 758 women, both subjective and objective cure rates were found to be inferior for single-incision slings compared to transobturator and retropubic slings(24). Patients who had previously undergone mini-slings were more likely to require repeated surgery for SUI and there was an increased incidence of de novo urgency(24). Nevertheless, shorter operative times and lower pain scores were noted(24). It is important to mention that more long-term data regarding the success and safety of single-incision or mini-slings are needed for a comprehensive assessment of their efficacy(24).
1.4. Autologous rectus fascial sling
An alternative to using synthetic mesh involves using a patient’s own native tissue, crafted into a sling to provide support to the urethra(25). This approach has a history of over 80 years and typically uses materials like the rectus fascia, fascia lata or vaginal wall(5,10). Fascial slings are often chosen for the treatment of recurrent SUI following a synthetic sling procedure or in patients who have had complications after undergoing a synthetic sling procedure(10).
In a randomized controlled trial involving 655 women with SUI, who were randomly assigned to receive either a rectus fascia sling or Burch colposuspension, the success rates were higher for women who underwent the sling procedure at the 24-month follow-up (47% versus 38%; p=0.01)(26). However, more women who underwent the sling procedure experienced urinary tract infections, voiding difficulties and de novo urge incontinence(25). A systematic review of SUI surgeries found that retropubic and autologous fascial slings demonstrated similar efficacy, though fascial slings were associated with a higher incidence of post-surgery voiding dysfunction and de novo urgency(26).
2. Retropubic urethropexy
The fundamental principles of these procedures involve lifting and stabilizing the bladder neck and proximal urethra in a high retropubic position(10,27). Support for the urethra is achieved by securing sutures either to the Cooper’s (iliopectineal) ligament or to the periosteum of the pubic bone(10). When sutures are placed through the Cooper’s ligament, the procedure is known as the Burch procedure(27). In contrast, the Marshall-Marchetti-Krantz (MMK) procedure involves sutures passing through the retropubic periosteum(27). It’s worth noting that the MMK procedure was associated with a rare complication called osteitis pubis (0.74-2.5%), which has since been discontinued(27).
Both of these procedures can be performed through either an open incision or laparoscopically(10). However, it is important to mention that these procedures were linked to longer operating times, wound infections and hematoma formation(21). A Cochrane review in 2012 concluded that open Burch colposuspension is effective for treating SUI in the long term(27). In the first year, the overall cure rate is approximately 85-90% and, after five years, around 70% of patients can anticipate being free from SUI symptoms(27).
In 2014, an RCT conducted by Trabuco assessed the comparison between Burch retropubic urethropexy (n=56) and midurethral sling with concurrent sacrocolpopexy (n=57)(28). There was no difference between the two groups regarding how patients perceived symptom improvement or the severity of incontinence(28). Nevertheless, after six months, women who underwent a midurethral sling procedure were more inclined to rate their treatment for urinary leakage as very successful, with a score of 10 on a visual analog scale ranging from 0 to 10, compared to women who received a Burch procedure (71% [34/48] versus 50% [23/46]; p=0.04)(28). Furthermore, those who had a midurethral sling were more likely to report a higher level of satisfaction compared to those who underwent a Burch procedure (78% [38/49] versus 57% [27/47]; p=0.04)(28). No difference was found in patient global impression of severity or symptom improvement, complication rates or mesh exposures(28).
Discussion
This comprehensive qualitative review of the literature has evaluated the necessity of mesh in the treatment of female SUI. Our research suggests that mesh-based midurethral slings are a valuable minimally invasive option for SUI, demonstrating high short-term efficacy. It is essential, however, to recognize the importance of specialized training for surgeons and a high volume of procedures to ensure the long-term success and patient satisfaction with these techniques(11).
Mesh-based MUS, including both retropubic and transobturator approaches, are associated with substantial improvements in the quality of life for women suffering from SUI(1). The data analyzed were extracted from the 31 selected studies and suggest that these procedures offer similar cure rates to traditional surgical interventions like Burch colposuspension, but with the added benefit of a minimally invasive approach, shorter operative times and potentially less post-operative discomfort. Notably, the transobturator tape (TOT) approach demonstrates a lower incidence of bladder perforations compared to the retropubic tape (TVT) method, albeit with a higher risk of groin pain(22,23).
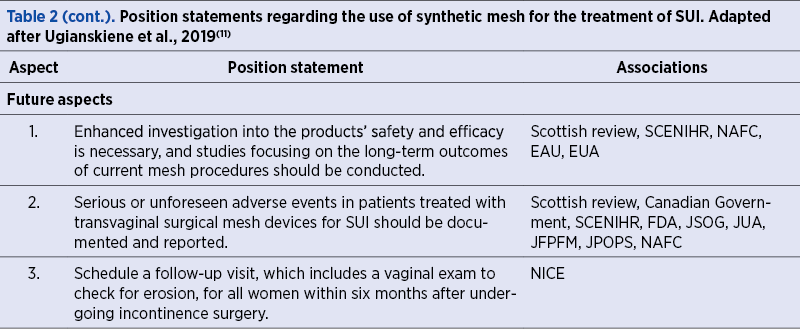
The enduring debate surrounding the use of mesh in urogynecology surgeries has been fueled by concerns over mesh-related complications. Although the FDA has deemed the materials used in these procedures to be safe, the exclusion of studies focusing solely on mesh complications may indicate an underrepresentation of these risks in the current synthesis of evidence. Long-term safety remains a paramount concern, as mesh-related complications can be severe and may not present until several years post-operation. The emergence of single-incision slings (mini-slings) presents a novel approach with the potential for reduced complications; however, our review identifies a need for further long-term studies to validate their efficacy and safety profile(24).
Autologous slings, utilizing the patient’s own tissue, serve as an alternative to synthetic mesh and have shown promising results, particularly in cases of recurrent SUI or when previous mesh surgeries have led to complications(26). While the evidence suggests higher success rates with autologous slings compared to Burch colposuspension, the increased risk of urinary tract infections and voiding dysfunctions cannot be overlooked(26).
Our review supports the notion that the choice of surgical intervention for SUI should be individualized, with a thorough consideration of the patient’s specific circumstances, the surgeon’s expertise and the availability of long-term follow-up care. The shared decision-making process, the informed consent and the adherence to best practice guidelines are crucial for optimizing patient outcomes.
The current landscape of SUI treatment is shifting towards less invasive procedures with a focus on improving the patient’s quality of life. The advent of regenerative medicine and bioengineering may soon offer new alternatives for treatment. However, until such advancements are clinically viable, mesh-based MUS remains a key therapeutic option.
Mesh-based MUS procedures represent a significant advancement in the treatment of SUI, offering an effective and less invasive alternative to traditional surgeries. However, patient selection, surgical expertise and careful consideration of long-term outcomes are essential. As the field of urogynecology continues to evolve, further research is needed to optimize treatment strategies and to address the long-term safety of these interventions.
Future directions and research gaps
While our current surgical approaches are centered on repositioning and correcting weakened anatomical structures, the future holds exciting possibilities. Research is progressing with the premise that achieving a stronger urethral sphincter may be the key to success(31). Initial studies involving stem cells have shown promise(31). Rather than merely providing support to weakened tissue, the focus is shifting toward replacing and enhancing it(31). Early investigations involving skeletal muscle-derived stem cells have paved the way for the use of adipose-derived stem cells, which are easier to cultivate and administer(31).
In the era of molecular and regenerative medicine, the next generation of physician-scientists is poised to lead the field of female pelvic medicine and reconstructive surgery into new frontiers. State-of-the-art bioengineering techniques and well-designed clinical trials hold the potential to offer curative therapies for a wider range of patients. This represents an exciting prospect for the future of medical science in addressing female pelvic health.
Limitations
The limitations of this review include potential biases inherent in the selected literature and the exclusion of studies addressing solely the management of mesh complications. Additionally, the heterogeneity of study designs and outcome measures may limit the generalizability of the results.
Conclusions
The increasing prevalence of SUI in an aging female population necessitates effective and safe surgical interventions. Our comprehensive review underscores the role of mesh-based MUS as a cornerstone in the treatment of SUI. These techniques, characterized by their minimally invasive nature, have been shown to offer high short-term success rates and have positively impacted the quality of life for many women.
Both retropubic and transobturator MUS techniques have been compared favorably to traditional surgical interventions such as Burch colposuspension, providing similar cure rates with the advantage of reduced operative times and recovery periods.
In the realm of alternative treatments, autologous slings offer a viable option, especially in patients with recurrent SUI or previous complications with synthetic mesh. These slings, while demonstrating higher success rates, also carry an increased risk of urinary tract infections and voiding dysfunctions, which necessitates careful patients’ selection and counselling.
It is obvious that individualized treatment planning is imperative, taking into account patient’s preferences, surgeon expertise and the nuanced balance between benefits and potential risks. The shared decision-making process and the informed consent are paramount in aligning treatment choices with patient expectations and clinical guidelines.
Looking ahead, the field of SUI treatment is poised for transformation, with regenerative medicine and bioengineering on the horizon, potentially offering novel treatments that could revolutionize current standards of care. Until these advancements become established clinical practice, mesh-based MUS remain a fundamental treatment modality.
In summary, while mesh-based MUS have marked a significant advancement in SUI treatment, offering a less invasive alternative with a good safety profile, vigilance in patient selection and a commitment to long-term outcome evaluation remain essential. Ongoing research and development will continue to refine the surgical techniques and improve the lives of women affected by SUI.
Despite the progress made in diagnosing, treating and the post-treatment monitoring of SUI patients, the field is continually evolving. As urogynecology surgeons, it is important for us to help emphasize the evidence-based proven utility of these techniques for our patients suffering from SUI.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The Standardisation of Terminology in Lower Urinary Tract function: Report from the Standardisation sub-committee of the International Continence Society. Urology. 2003 Jan;61(1):37–49.
- Hampel C, Artibani W, Espuña Pons M, Haab F, Jackson S, Romero J, et al. Understanding the Burden of Stress Urinary Incontinence in Europe: A Qualitative Review of the Literature. European Urology. 2004 Jul;46(1):15–27.
- Luber K. The Definition, Prevalence, and Risk Factors for Stress Urinary Incontinence. Reviews in Urology. 2004;6(3):S3-9.
- Brubaker L, Cundiff G, Fine P, Nygaard I, Richter H, Visco A, et al. Abdominal Sacrocolpopexy with Burch Colposuspension to Reduce Urinary Stress Incontinence. The New England Journal of Medicine. 2006;354(15):1557–66.
- Bezerra CA, Bruschini H, Cody DJ. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database Syst Rev. 2005;(3):CD001754.
- Alcalay M, Monga A, Stanton SL. Burch colposuspension: a 10-20 year follow up [published correction appears in Br J Obstet Gynaecol 1996 Mar;103(3):290]. Br J Obstet Gynaecol. 1995;102(9):740-745.
- Ulmsten U, Henriksson L, Johnson P, Varhos G. An Ambulatory Surgical Procedure under Local Anesthesia for Treatment of Female Urinary Incontinence. International Urogynecology Journal and Pelvic Floor Dysfunction. 1996;7(2):81–6.
- Delorme E. La Bandelette trans-obturatrice: Un Procédé mini-invasif Pour Traiter l’incontinence Urinaire d’effort De La Femme. Progrès En Urologie. 2001;11(11):1306–13.
- Trabuco EC, Linder BJ, Klingele CJ, Blandon RE, Occhino JA, Weaver AL, et al. Two-Year Results of Burch Compared with Midurethral Sling with Sacrocolpopexy. Obstetrics & Gynecology. 2018;131(1):31–8.
- Garely AD, Noor N. Diagnosis and Surgical Treatment of Stress Urinary Incontinence. Obstetrics Gynecology. 2014;124(5):1011–27.
- Ugianskiene A, Davila GW, Su T. FIGO Review of Statements on Use of Synthetic Mesh for Pelvic Organ Prolapse and Stress Urinary Incontinence. International Journal of Gynecology & Obstetrics. 2019;147(2):147–55.
- Glazener CM, Cooper K, Mashayekhi A. Bladder Neck Needle Suspension for Urinary Incontinence in Women. Cochrane Database of Systematic Reviews. 2017;7(7):CD003636.
- Richter H, Albo M, Zyczynski H, Kenton K, Norton P, Sirls L, et al. Retropubic versus Transobturator Midurethral Slings for Stress Incontinence. The New England Journal of Medicine. 2010;362(22):2066-2076.
- Brubaker L, Norton PA, Albo ME, Chai TC, Dandreo KJ, Lloyd KL, et al. Adverse Events over Two Years after Retropubic or Transobturator Midurethral Sling surgery: Findings from the Trial of Midurethral Slings (TOMUS) Study. American Journal of Obstetrics and Gynecology. 2011;205(5):498.e1–6.
- Andonian S, Chen T, St-Denis B, Corcos J. Randomized Clinical Trial Comparing Suprapubic Arch Sling (SPARC) and Tension-Free Vaginal Tape (TVT): One-Year Results. European Urology. 200547(4):537–41.
- Ford AA, Rogerson L, Cody JD, Ogah J. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2015;(7):CD006375.
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2009;(4):CD006375.
- Abdel-Fattah M, Ramsay I, Pringle S, Hardwick C, Ali H, Young D, et al. Randomised Prospective Single-blinded Study Comparing “Inside-out” versus “Outside-in” Transobturator Tapes in the Management of Urodynamic Stress incontinence: 1-year Outcomes from the E-TOT Study. BJOG: an International Journal of Obstetrics & Gynaecology. 2010;117(7):870–8.