Aim. This study was undertaken to determine the prevalence of Trichomonas vaginalis infection in women of reproductive age from Kosovo. Methodology. The study was carried out in the Obstetrics and Gynecology Clinic of the Faculty of Medicine, University of Pristine, Kosovo, between April and July 2022. The study population consisted of a total of 207 women. Sexually active women aged at least 20 years old were included in the study. A semi-structured questionnaire was distributed to the participants to seek for information such as age, marital status, occupation and pregnancy status. Every woman’s informed consent was sought before the collection of specimens by qualified medical personnel. The specimens were carefully and aseptically collected from the high vaginal area using well-labeled, sterile, non-abrasive high vaginal swab sticks. A few drops of normal saline were added to each swab stick, and a wet mount examination was performed within less than half an hour of collection in order to get optimal results. The wet preparation of the vaginal discharge was made by applying a drop from the sample to a small area of a clean glass slide with a cover slip in order not to trap air bubbles. The wet smear was examined microscopically for motile T. vaginalis with a low-power objective (x10) and then with a high-power objective (x40). The vaginal secretion was characterized by the presence of epithelial cells, white blood cells and red blood cells. The T. vaginalis trophozoite was identified by its oval, flagellated and distinctive motility (jerky movement). Results. An overall prevalence rate of 12.56% was found in Kosovo. The prevalence of T. vaginalis infection differed from place to place. It varied as well among age groups, showing the highest prevalence in the age group of 30-39 years old (13.63%), and the lowest in the age group of 20-29 years old (5.70%). The prevalence varied with marital groups, being the highest in divorced women (30.76%) and the lowest among singles (6.74%). The prevalence rate was also observed to be highest among the employed (19.71%) and lowest among students (14.81%) and unemployed (7.33%). T. vaginalis infection was observed in non-pregnant women in a prevalence rate of 15.20%. Conclusions. T. vaginalis infection is prevalent in women of reproductive age, as evident in our country. The infection is common in sexually active female participants, especially in those with multiple sex partners. Proper personal hygiene, faithfulness to one sexual partner, and massive public awareness on the prevention and control of T. vaginalis are advised to reduce its prevalence among women of reproductive age in our country.
Prevalence of Trichomonas vaginalis infection in women of reproductive age in Kosovo
Prevalenţa infecţiei cu Trichomonas vaginalis la femeile de vârstă reproductivă din Kosovo
First published: 30 aprilie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.71.1.2023.8144
Abstract
Rezumat
Introduction
Trichomonas vaginalis is a protozoan parasite that causes a sexually transmitted disease (STD). The infection invades the urogenital tract of sexually active women and men, causing substantial vaginal and cervical ulceration(1). After bacterial vaginosis and candidiasis, this infection ranks third among the diseases that usually cause vaginal symptoms. Trichomonas vaginalis, the causative organism, is extremely specific for the genitourinary tract and has been isolated from all genitourinary areas(2). Trichomonas vaginalis has been known as a broad-based parasite of the genital tract in both males and females. The life cycle of this parasite is not well known, as it is recognized to be only as trophozoites and doesn’t have a cystic stage(3). The trophozoite is an oval parasite with five flagella and an axostyle used to anchor to surfaces(4). It has a yearly prevalence of about 180 million cases in the world(5). Many cases of trichomoniasis are localized in regions of small income, mainly in Africa, where the prevalence rate is estimated between 15% and 37%(6-8), due to a dearth of sufficient facilities for healthcare(5). The infection is largely acquired through sexual contact and rarely through nonsexual contact, by contact with fomites(2). The symptoms of Trichomonas vaginalis infection are usually seen in women more than in men(9); they may comprise frothy greenish, foul-smelling vaginal discharge followed by vulvovaginal irritation, postictal bleeding, high frequency in micturition, lower abdominal pains and dysuria(10). Low-birth-weight infants, neonatal mortality, preterm delivery, preterm rupture of membranes and morbidity are consequences related with pregnancy(11). The public health significance of this infection is underscored by the fact that Trichomonas vaginalis infection is prevalent in women of reproductive age and is linked with serious adverse pregnancy consequences(12). This infection could also increase the risk of human immunodeficiency virus (HIV) transmission and of other STD infections, which are significantly more common in women(13). This study was designed to determine the prevalence of Trichomonas vaginalis infection among women of reproductive age in Kosovo.
Materials and method
The study was carried out in the Obstetrics and Gynecology Clinic of the Faculty of Medicine, University of Pristine, Kosovo, between April and July 2022. This clinic offers tertiary healthcare.
Study population
The study population consisted of a total of 207 women. Women of reproductive age not less than 20 years old were included in the study. A structured questionnaire was distributed to the participants to seek for information such as age, marital status occupation, and pregnancy status. The obtained data were used to determine the independent variables in the transmission of T. vaginalis infection.
Ethical consideration and exclusion criteria
An ethical approval letter was obtained from the Chamber of Doctors of Kosovo, to facilitate the study. Participation was voluntary, and the informed consent was sought from each participant before the collection of specimens. The study was conducted with strict adherence to the ethical standards and procedures for research with human participants. The participants selected for the study were all women visiting the Obstetrics and Gynecology Clinic. Sexually active women aged 20 years and older were included in the study. The females in their menstrual period were exempted from the study.
Specimen collection
Specimens of vaginal discharge were carefully collected aseptically from the high vaginal area using a well-labeled, sterile, non-abrasive swab stick. The samples were collected with the aid and supervision of the medical staff of the hospitals. The samples were taken to the hospital laboratory units and microscopically examined within two hours of collection.
Parasitological examination
A few drops of normal saline were added to each vaginal swab stick. Each specimen was then placed on a clean, grease-free slide covered with a cover slip and examined microscopically with low power (x10) and high power (x40) objectives(10). Identification of the presence of T. vaginalis was done according to Onyido et al.(14) which stated that the presence of T. vaginalis is detected by the characteristic jerky movement of the parasite and identified by the characteristic four flagella, axostyle, and oval shape.
Data analysis
The data obtained were analyzed using IBM SPSS Statistics, version 21.0. Differences and associations between categorical variables were tested using Pearson’s chi-square test and considered statistically significant at p<0.05. The resulting output was presented in tables.
Results
Table 1 shows the overall prevalence of T. vaginalis infection in the Obstetrics and Gynecology Clinic. Out of 207 women examined, 26 (12.5%) were positive, while 181 (87.4%) were negative.
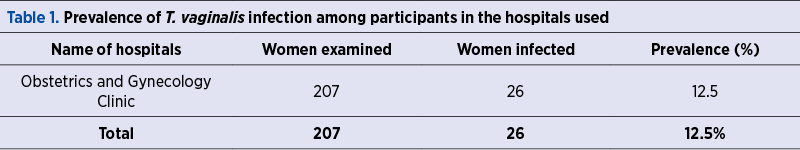
Table 2 shows the age-specific prevalence of T. vaginalis infection among the participants. Out of the 69 women from the age group 20-29 years old, 12 (5.70%) were positive. In the age group of 30-39 years old, nine (13.63%) out of 66 were positive. Of the 58 women in the age group of 40-49 years old, five (9.09%) were positive. In the last age group, 50-59 years old, none of the 17 women examined were positive. T. vaginalis infection was significantly higher among reproductive women aged 30-39 years old (13.63%) than in other age groups (p<0.05).
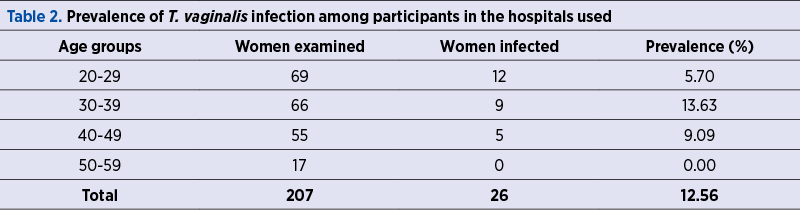
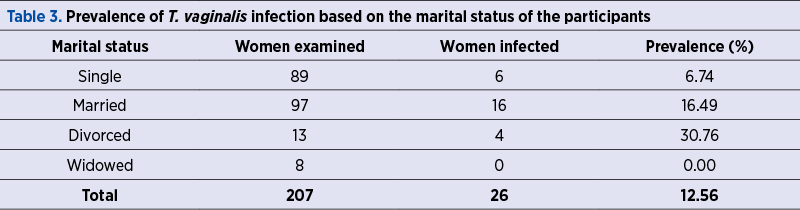
Table 3 shows the rate of prevalence of T. vaginalis infection according to the marital status of the participants. Out of the 89 single participants, six (6.74%) tested positive. Out of 97 married women examined, 16 (16.49%) were positive. Four (30.76%) out of 13 divorced women were positive. All eight widowed women used for the study were negative. T. vaginalis infection has a likelihood of being significantly higher in divorced women than in married and single women (p<0.05).
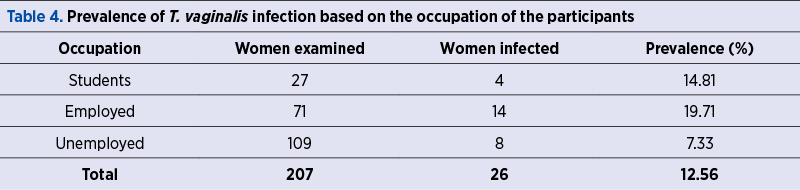
Table 4 shows the prevalence of T. vaginalis infection based on the occupation of the participants. Out of 71 employed examined, 14 (19.71%) were positive. Out of 27 students who participated in the study, four (14.81%) were found to be positive. Among the unemployed, eight (7.33%) out of 109 turned out to be positive. Hence, T. vaginalis infection is likely to be significantly higher in employed than in students and unemployed (p<0.05).
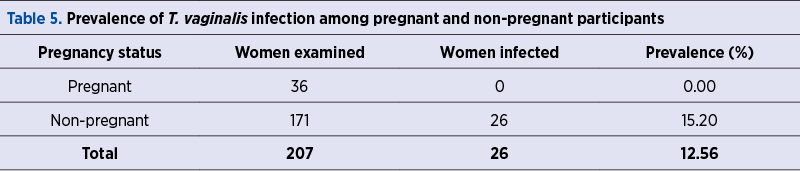
Table 5 shows the prevalence of T. vaginalis infection among pregnant and non-pregnant women who participated in the study. All 36 pregnant participants were negative. However, 26 (15.20%) of the 171 non-pregnant women included in the study were positive. T. vaginalis was observed only among non-pregnant women. T. vaginalis infection was significantly higher in non-pregnant women (p<0.05).
Discussion
This study showed an overall prevalence of 12.56%, out of the 207 women from the Obstetrics and Gynecology Clinic, Pristine, Kosovo. The prevalence of 12.56% observed in this study could be explained by the fact that the majority of cases of trichomoniasis are localized in regions of low income, compared to African countries, where the prevalence rate ranges from 11% to 37%(8,14-18).
T. vaginalis infection prevalence varied with respect to age. The highest prevalence was reported among women aged 30-39 years old (13.63%) and the lowest in the age group of 20-29 years old (5.70%). This result is consistent with the findings of Auta et al.(3), who recorded the highest prevalence among women aged 30-36 years old (9.32%) and the lowest prevalence in the age group of 26-30 years old (6.10%). The result is in disagreement with the findings of Iwueze et al.(17), who observed the highest prevalence in the age group of 21-30 years old (47.2%) and the lowest prevalence among women aged 31-40 years old (8.6%). Nevertheless, the result is similar to the findings of Onyido et al.(14), who observed a prevalence of 35% among the 30-39 years old age group, and 0% amidst the younger age group of 20-29 years old. The result recorded among women aged 40-49 years old (9.09%) corresponds with the findings of the aforementioned authors, who also observed prevalence rates of 4.7%, 9.6% and 8%, respectively, among women aged 40-49 years old. On the contrary, none of the women in the age group of 50-59 years old was positive, which is not in agreement with the findings of Onyido et al.(14) (21.43%) and Iwueze et al.(17) (8%). The age-specific prevalence could be as a result of a higher sexual activity amongst the age group of 20-29 years old and probably as a result of the asymptomatic persistence of earlier infections and inadequate hygiene. However, T. vaginalis infection remains prevalent among highly sexually active women aged 30-49 years old. Onyido et al.(14) reported that 2-3 million infections occur normally among sexually active women. Hence, it is justified since sexual intercourse is the primary route of T. vaginalis infection.
The prevalence of T. vaginalis also varied with marital status, with divorcees (30.76%) having the highest prevalence and singles showing the lowest prevalence (6.74%). A prevalence level of 16.49% was observed among married women. The high prevalence among divorced women could be due to their more active sexual life, as having multiple sex partners plays a vital role in the prevalence rate. The prevalence among married and single women could be as a result of infected partners, poor hygiene and the persistence of the infection without treatment.
T. vaginalis prevalence differed according to the occupations of the participants. The employed undoubtedly had the highest prevalence (19.71%), followed by students (14.81%), and the unemployed had the lowest prevalence (7.33%). The result is not in agreement with the findings of Obiukwu et al.(16), who observed that the prevalence was higher in students (6.7%), employed (2.7%) and unemployed women (1.3%). The high prevalence among employed could be due to the fact that employment encompasses all sorts of travel. The low prevalence among unemployed and students could be a result of a high level of literacy, fewer travel and proper awareness. However, the prevalence was slightly higher in the present study and could be due to the practice of poor hygiene, sexual activity, and occasionally non-sexual contact with fomites or surfaces that are contaminated by an infected individual’s fluid(2).
Trichomonas vaginalis infection was not detected in all the pregnant women who participated in the study; a prevalence rate of 15.20% was observed in non-pregnant women. The infection was not prevalent in pregnant women, probably as a result of incorrect collection of vaginal discharge from the high vaginal wall.
Conclusions
Trichomonas vaginalis infection is prevalent in women of reproductive age, as evident in our country. The infection is common in sexually active female participants, especially in those with multiple sex partners. Proper personal hygiene, faithfulness to one sexual partner, and massive public awareness on the prevention and control of T. vaginalis are advised to reduce its prevalence among women of reproductive age in our country.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
Krieger JN. Trichomonas vaginalis and Trichomoniasis. McGraw-Hill, New York, 2010, 587-589.
-
Ogomaka IA, Nwachinemere AV, Obeagu EI. Prevalence of Trichomoniasis among adults in Oru-East L.G.A, Imo State, Nigeria. Medical Public Journals. 2018;9:1-2.
-
Auta IK, Ibrahim B, Henry D. Prevalence of Trichomonas vaginalis among Pregnant Women Attending Antenatal Clinic in Two Health Facilities within Kaduna Metropolis, Kaduna, Nigeria. Science World Journal. 2020;15(1):89-99.
-
Swygard H, Sena AC, Hobbs MM, Gohen MS. Trichomoniasis clinical manifestations diagnosis and management. Sexually Transmitted Infections. 2004;80:91-95.
-
World Health Organization. Global Prevalence and Incidence of selected Curable Sexually Transmitted Diseases Overview and Estimates. World Health Statistics. 2012.
-
Okoko FJ. Prevalence of Trichomoniasis among Women at Effurun Metropolis, Delta State, Nigeria. Crescent Journal of Biological Sciences. 2011;4(2):45-48.
-
Sam-wobo SO, Ajao OK, Adeleke MO, Ekpo UF. Trichomoniasis among Antenatal Attendees in a Tertiary Health Facility, Abeokuta, Nigeria. Munis Entomology and Zoology Journal. 2012;7(1):380-384.
-
Chinedum OK, Ifeanyi OE, Ugwu UG, Ngozi GE. Prevalence of Trichomonas vaginalis Among Pregnant Women Attending Hospital in Irrua Specialist Teaching Hospital in Edo State. Nigeria Journal of Medical and Dental Sciences. 2014;13(9):79-82.
-
Smith DA, Ramos N. Trichomoniasis. E-Medicine Specialties. 2010. http://www.emedicine.mediscape.com.
-
Center for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guideline. Morbidity and Mortality Weekly Report. 2006;55:1-94.
-
Johnson HL, Ghanem KG, Zenilman JM, Erbelding EJ. Sexually transmitted infections and adverse pregnancy outcomes among women attending inner city public sexually transmitted diseases clinics. Sex Transm Dis. 2011;38(3):167-171.
-
Silver BJ, Guy RJ, Kaldor JM, Jamil MS, Rumbold AR. Trichomonas vaginalis as a cause of perinatal morbidity: a systematic review and meta-analysis. Sex Transm Dis. 2014;41(6):369-376.
-
Kissinger P, Adamski A. Trichomoniasis and HIV interactions: a review. Sex Transm Infect. 2013;89(6):426-433.
-
Onyido AE, Umeanaeto PU, Irikannu KC, Ekwunife CA, Ezeanya LC, Nwangwu UC, Ugha CN, Obiechina IO. Prevalence of Trichomonas vaginalis among the rural women of Ekwumili Community, Anambra State, Southeastern Nigeria. Nature and Science. 2014;12(5):129-134.
-
Gundiri MA, Okwuosa VN. Prevalence of urinary and intestinal tracts parasites in Kwampe, Langtong, North Nigeria. Nigerian Journal of Parasitology. 2005;26:19-22.
-
Obiukwu MO, Onyido AE, Duru JU, Aleke O. Trichomonas vaginalis infection in Anambra State: Demographic and Behavioural Predictors. Journal of Advancement in Medical and Pharmaceutical Sciences. 2010;4(11):16-20.
-
Iwueze MO, Ezeanya LN, Okafor FC, Nwaogu OC, Ukibe SC. Prevalence of Trichomonas vaginalis infection among women attending hospitals/health centers in Onitsha Community, Onitsha North Local Government Area of Anambra State. The Bioscientists. 2014;2(1):54-64.
-
Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015 [published correction appears in MMWR Recomm Rep. 2015 Aug 28;64(33):924]. MMWR Recomm Rep. 2015;64(RR-03):1-137.