The successful restoration of the physiognomic function of the anterior area of the dental arches requires the dentist to have advanced knowledge of the facial, dentofacial and marginal periodontal aspects and, at the same time, to master the techniques of working with adhesive materials. Composite resins are currently the materials of choice for regaining the optimal esthetic appearance in the frontal region, because they present both the ability to preserve dental tissues (through chemical adhesion to the substrate) and extensive esthetic possibilities, which give rise to a wide variety of clinical and therapeutic indications.
Esthetic function direct restoration in the anterior area – case report
Refacerea funcţiei estetice a zonei anterioare prin metode directe – prezentare de caz
First published: 24 noiembrie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ORL.61.4.2023.8964
Abstract
Rezumat
Restaurarea cu succes a funcţiei fizionomice a zonei anterioare a arcadelor dentare impune ca medicul dentist să aibă cunoştinţe avansate despre aspectul facial, dentofacial şi al parodonţiului marginal şi, în acelaşi timp, să stăpânească tehnicile de lucru cu materiale adezive. Răşinile compozite sunt materialele de elecţie la ora actuală pentru redobândirea aspectului optim estetic în zona frontală, deoarece acestea prezintă atât capacitatea de a conserva ţesuturile dentare (prin adeziunea chimică la substrat), cât şi posibilităţi estetice extinse, care dau naştere la o mare varietate de indicaţii clinice şi terapeutice.
Introduction
The esthetic aspect has always been particularly important for each person. We all want to reach an ideal of perfection, even though this is not possible. Modern society puts a special emphasis, which can even mean pressure, so that the facial esthetics is essential for social integration. For this reason, from the dentist’s point of view, we have the duty to integrate dental esthetics into current practice. In dentistry, beauty is reflected by the symmetry, the degree of visibility, proportion and color of the teeth, as well as by other elements that together make up the “recipe” for a harmonious smile(1,2).
The loss of hard tooth substance in the anterior region of dental arches, as a result of carious processes or trauma, has a high impact on the physiognomic function. On the other hand, dental destructions in the lateral areas affect both the health and the esthetic appearance of the oral cavity and the rest of the body(3).
Dental esthetics is actually a business card in our society. The desire to contour beautiful smiles that give confidence in one’s own powers, shared with loved ones and offered without reluctance to the people around, is the main objective of the dentists when performing cosmetic procedures and dental restorations in the frontal area(4,5). The physiognomic function can be affected both by lesions with loss of substance (dental caries, trauma, dental wear, abfraction) and by lesions without loss of hard dental substance (dyschromia, different types of dental anomalies, crowded or ectopic teeth).
Dental esthetics
In the context of the oral rehabilitation of a patient with alterations of the dentomaxillary apparatus, it is important to take into account its functions: masticatory, breathing, swallowing, phonatory and esthetic. The latter, being the most aware by patients, has acquired a very important role in dental restorations. The technological advance and the dental materials industry have facilitated dentist’s work in meeting the esthetic requirements of the patients(6).
The size, shape, position and color of the teeth must harmonize, have proportional and symmetrical relations with the other teeth, but also with the neighboring structures: lips, gums, facial features. All these elements create an esthetic, harmonious appearance of the face.
In restorative dentistry, the dentist encounters a multitude of elements that modify the patient’s dental and dentofacial harmony and, consequently, his/her physiognomic aspect. As a result, the treatment of dental esthetic dysfunction is complex and is carried out depending on the etiology, the degree of dysfunction’s severity, the age and the financial resources of the patient(7). Sometimes, it is mandatory the interdisciplinary approach to the respective clinical situation for a successful result.
The most common ways to restore the physiognomy in the anterior area with direct restorative methods are:
-
direct restorations of the hard dental tissue loss
-
direct veneers with composite materials
-
ameloplasty
-
dental bleaching
-
microabrasion.
Direct restorations with composite materials of the hard dental substance loss in the frontal area represent perhaps the most common therapeutic act that the dentist performs in order to restore the esthetic function in the anterior area(8,9). With the advent of light-curing composite resins in the 1970s, dentistry became more predictable, offering longer working time and better physical properties of the restorative materials.
Today, after decades of development and research in the laboratory supported by clinical studies, composite resins have been confirmed as the restorative materials of choice for both the frontal and posterior areas(10). The progress of adhesive dentistry – respectively, the evolution of amelodentinal adhesion – has allowed the achievement of amazing results, quickly and ultra-conservatively, without the help of the dental laboratory, having at its disposal materials capable of faithfully reproducing the dental morphology and coloristic characteristics(11,12). Special care must be taken in selecting the color but, following the basic principles of determining the color and using the composite resin layered insertion techniques, excellent results can be obtained.
Case report
A patient has presented to the dental practice for improving dental esthetics in the anterior region affected by dental caries in tooth 21 (distal) and tooth 22 (mesial) – Figure 1. For this case, we decided to use Ceram.X Sphere TEC one (Dentsply Sirona), a nanoceramic universal resin composite light curing restorative material, which ensures excellent bonding, resistance and esthetics results.

The treatment steps were as follows: removing the dental biofilm with professional brushing, choose the proper color tooth shade (in this case, the color was A2 on Vita classical shade guide, corresponding to A2 cloud shade for this composite) and dental isolation.
The next step was to remove all the hard dental tissues affected by carious process (enamel and dentin) in both teeth, and two class III cavities have been obtained. The cavities disinfection was done using 2% chlorhexidine (Figure 2).

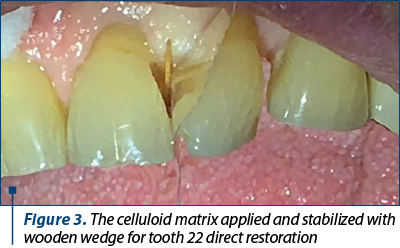
In order to insert the restorative resin composite material, a celluloid matrix has been applied between the two incisors. The strip has been stabilized with a wooden wedge on tooth 22, this one being the first one we will restore. This will enable the establishment of a proper interproximal contact with adjacent teeth and, also, allowing the passage of light during the polymerization of restorative material (Figure 3).
The next stage of treatment consisted in achieving specific dental adhesion stages. We used total-etch technique, for both dentin and enamel: we applied 35% phosphoric acid gel for 15 seconds on dentin and 30 seconds on enamel; then, it was rinsed with water and the tooth surfaces have been dried with air and the bonding system applied. Next, the bonding was cured for 20 seconds and the resin composite was inserted inside the plastic matrix and tooth proximal cavity, using incremental technique, namely stratified layering technique. Every layer was cured for 20 seconds. The A2 cloud shade of Ceram.X Sphere TEC one (Dentslpy Sirona) covers A2, B2 and D2 shades in Vita guide, so we obtained an excellent esthetic result. When we achieved an entire shape and proximal contour of the mesial area in tooth 22, the wooden wedge and matrix were removed and we proceed for finishing and polishing of the restoration, using fine diamond polishing burs, followed by composites abrasive discs and dental polishers (Figure 4).

For the class III distal cavity in tooth 21, the same steps were followed.

Conclusions
Resin composites are without question the material of choice in modern dentistry, with which clinical situations of esthetic function alteration that previously required indirect restorations can be solved. Nowadays, these materials present improved bonding, mechanical and especially esthetics properties which makes possible to faithfully reproduce the color, the shade, the degree of saturation of teeth color, as well as the opacity or translucency in specific areas, like the incisal edges, so an excellent esthetic dental and facial aspect can be obtained.
Acknowledgements. For this article, all the authors have equal contributions.
Conflict of interest: none declared.
Financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.

Bibliografie
-
Popa MB. Estetica în Odontoterapia Restauratoare. Ed. Univ. „Carol Davila”, Bucureşti, 2006.
-
Blatz MB, Chiche G, Bahat O, et al. Evolution of Aesthetic Dentistry. J Dent Res. 2019;98(12):1294–1304.
-
Eltahlah D, Lynch CD, Chadwick BL, Blum IR, Wilson NHF. An update on the reasons for placement and replacement of direct restorations. J Dent. 2018;72:1-7.
-
Gheorghiu IM, Mitran L, Mitran M, Scărlătescu S, Iliescu AA, Perlea P. Direct anterior restoration of hard dental tissue loss – case report. ORL.ro. 2019;45(4):44-46.
-
Tekçe N, Demirci M, Tuncer S, Güder G, Sancak EI. Clinical Performance of Direct Composite Restorations in Patients with Amelogenesis Imperfecta - Anterior Restorations. J Adhes Dent. 2022;24(1):77-86.
-
Brown KM, Gillespie G. Advancements in Composite Resin Material Enable Streamlined Direct Restoration Process. Compend Contin Educ Dent. 2019;40(Suppl 2):2-6.
-
Almulhim KS, AlSheikh R, Abdalla M, Haridy R, Bugshan A, Smith S, Zeeshan M, Elgezawi M. Toward esthetically and biomechanically reliable anterior resin composite restorations: Current clinical experiences among dental practitioners in Saudi Arabia. F1000Res. 2023;12:359.
-
Zhang HY, Hou BX. Clinical application of direct composite resin in esthetic restoration. Zhonghua Kou Qiang Yi Xue Za Zhi. 2023;58(5):409-413.
-
Dietschi D, Shahidi C, Krejci I. Clinical performance of direct anterior composite restorations: a systematic literature review and critical appraisal. Int J Esthet Dent. 2019;14(3):252-270.
-
Mackenzie L, Parmar D, Shortall AC, Burke FJ. Direct anterior composites: a practical guide. Dent Update. 2013;40(4):297-9, 301-2.
-
Shah YR, Shiraguppi VL, Deosarkar BA, Shelke UR. Long-term survival and reasons for failure in direct anterior composite restorations: A systematic review. J Conserv Dent. 2021;24(5):415-420.
-
Demarco FF, Collares K, Coelho-de-Souza FH, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Anterior composite restorations: A systematic review on long-term survival and reasons for failure. Dent Mater. 2015;31(10):1214-24.
Articole din ediţiile anterioare
Direct composite veneers for erosive-abrasive lesions – case report
Tratamentul leziunilor dentare abrazive şi/sau erozive este unul conservator. Una dintre metodele de tratament este faţetarea directă sau indire...
Tratamentul leziunilor dentare necarioase
Leziunile dentare necarioase – fie că sunt cu sau fără pierdere de substanţă – conduc la apariţia tulburărilor fizionomice, având, de asemenea, un ...
Restaurarea directă în zona frontală a distrucţiilor dentare coronare – prezentare de caz
Acest articol prezintă o temă de actualitate în domeniul medicinei dentare restaurative: restaurarea directă a distrucţiilor dentare coronare în...
Sensibilitatea postoperatorie asociată restaurărilor cu răşini compozite
În practica clinică ne confruntăm adesea cu durerea postoperatorie dentinară care apare după restaurarea directă coronară cu răşini compozite. Ar...