Osteomas are benign tumors of the paranasal sinuses, and are mostly located in the frontal sinus. The evolution of the osteomas is slow and silent. The osteomas are often discovered incidentally on a craniofacial CT scan. Due to the slow growing nature of this tumour, the therapeutic approach is usually “watch and wait”. When symptoms occur, the surgical approach is required. This can be external, endoscopic or combined. The authors report the case of a 55-year-old female patient who was admitted to the hospital with a history of progressive frontal headache for 12 months. The clinical ENT examination and the paralinical exams (nasal endoscopy, computed tomography – head, paranasal sinuses) were suggestive for a left frontal sinus osteoma. The surgical management of the osteoma was a combined approach, including the external Ogston-Luc technique and the endoscopic approach. The postoperative period was uneventful, with no complications, and the drain tube was removed 14 days after surgery.
Frontal sinus osteoma – case report
Frontal sinus osteoma – case report
First published: 26 septembrie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Orl.44.3.2019.2549
Abstract
Rezumat
Osteomul reprezintă o tumoră benignă a sinusurilor paranazale, afectând cu predilecţie sinusul frontal. Are o evoluţie lentă şi silenţioasă, fiind descoperit adesea accidental prin examenul CT efectuat pentru diagnosticul altor patologii rinosinuzale. Atitudinea terapeutică uzuală este „watch and wait”, dar în momentul în care osteomul devine simptomatic, tratamentul de elecţie este chirurgical, prin tehnici endoscopice clasice sau prin abord mixt. Lucrarea prezintă cazul unei paciente în vârstă de 55 de ani care se internează în spital pentru cefalee frontală cronică progresivă debutată în urmă cu aproximativ un an. Examinările clinice şi paraclinice (examinare endoscopică, examen computer-tomografic cranio-cerebral) ridică suspiciunea unui osteom de sinus frontal stâng. Conduita terapeutică de elecţie este cea chirurgicală, prin abord mixt, extern (de tip Ogston-Luc) şi endoscopic. Evoluţia postoperatorie a fost favorabilă, fără complicaţii, tubul de drenaj fiind înlăturat la 14 zile de la operaţie.
Case report
We present the case of a female patient, 55 years old, who was admitted to the hospital with complaints of frontal headache and minor left nasal obstruction for one year. The clinical and endoscopic ENT examinations (pain of the frontal left sinus pressure point, clear nasal fossae), as well as paraclinical examinations (native computed tomography of the paranasal sinuses – Figure 1) showed an extensive, hyperdense, round-ovalar, sessile tumor of the left frontal sinus, of approximately 20/12 mm, with attachment on its anterior wall, expanding through the frontal sinus cavity.

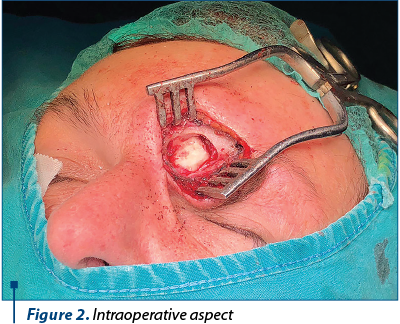
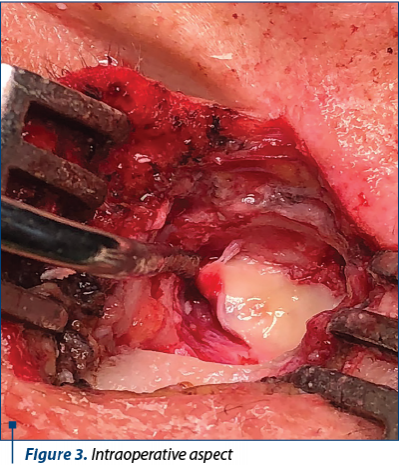
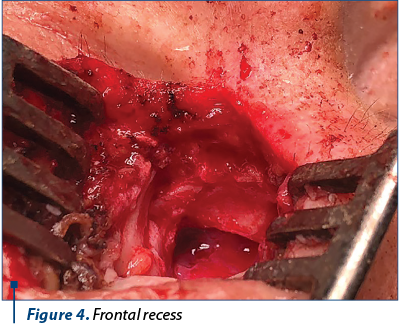
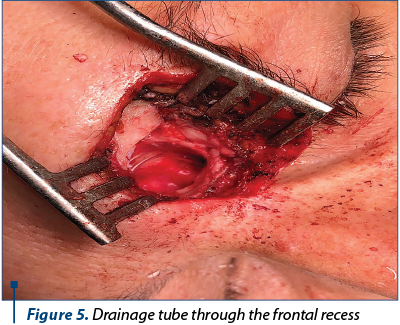
The clinical and paraclinical examinations revealed a voluminous left frontal sinus osteoma. After accurate preoperative preparations, surgery was performed (Figures 2, 3, 4 and 5) using a combined surgical approach: external (Ogston-Luc technique) and endoscopic. We made an arcuate over-brow incision in the medial half of the eyebrow arch, followed by tegument, muscle and periosteum surgical dissection. We performed the trephination of the anterior wall of the left frontal sinus, uncovering the tumoral growth inside the sinus. The tumor was white and had a hard-bone consistency, emerging from the anterior wall of the left frontal sinus. Tumor excision was then performed and the specimen was sent for histopathological examination. Under endoscopic control, a passive drainage tube was mounted in the nasofrontal canal. The tube was then attached to the vestibulum nasi with a suture thread. The left frontal sinus cavity was filled with hemostatic sponge, then we restored the tissue alignment and did the wound dressing.
The histopathologic examination confirmed the diagnosis of left frontal sinus osteoma.
The postoperative evolution was favorable. The patient received i.v. broad-spectrum antibiotics, NSAIDs, analgesic treatment, gastric protection and nasal decongestants. Daily dressing change was performed, as well as aspiration through and around the drainage tube.
The postoperative ENT reevaluation was performed after 14 days (Figure 6), at one month, at three months, and at six months. The patient’s post-surgical evolution was uneventful, without any immediate or long-term complications.

Discussion
Osteoma is the most common tumor of paranasal sinuses, often with a slow and silent evolution. The most frequently involved site is frontal sinus, followed by ethmoid and maxilar sinuses. The sphenoid sinus is rarely involved(1,2). Males are slightly more often affected by this disease than females (M:F ratio = 1.3:1)(3).
In general, the dimension of osteomas may vary between 2 and 30 mm. Osteomas bigger than 30 mm or the ones weighing more than 110 g are considered to be giant(4).
The etiology of osteomas is still unknown. Several hypotheses have been taken into consideration: traumatic or infectious triggers, calcium metabolism disorders, or embryonic malformations(5).
Frontal sinus osteoma grading system(6)
Grade I. The base of attachment is posterior-inferior along the frontal recess. The tumor is medial to a virtual sagittal plane through the lamina papyracea. The anterior-posterior diameter of the lesion is <75% of the anterior-posterior dimension of the frontal recess.
Grade II. The base of attachment is posterior-inferior along the frontal recess. The tumor is medial to a virtual sagittal plane through the lamina papyracea. The anterior-posterior diameter of the lesion is >75% of the anterior-posterior dimension of the frontal recess.
Grade III. The base of attachment is anterior or superiorly located within the frontal sinus and/or the tumor extends lateral to a virtual sagittal plane through the lamina papyracea.
Grade IV. Tumor fills the entire frontal sinus (the current case).
Osteomas are white, hard, well circumscribed, round or oval, sesile (rarely pediculated), bosselated tumors. Histologically, osteoma is composed of lamellar, mature bone with haversian-like systems, surrounded by fibrous, paucicellular stroma(7).
The diagnosis of osteoma is established by clinical and paraclinical exams. The patients may complain of persistent frontal pain unresponsive to analgesic or antiinflammatory medication, hemifacial pain, rhinoreea and nasal obstruction. If the growth of osteoma is also intraorbital, proptosis and/or diplopia may occur. Computed tomography of the head and paranasal sinuses is the gold standard for the diagnosis of osteoma and is also necessary for its management. MRI is useful when intracranial extensions are suspected(8).
The differential diagnosis(9) of frontal sinus osteoma includes: acute suppurative frontal sinusitis or exacerbated chronic frontal sinusitis, other rhinosinusal benign tumors (mucocele, adenoma, papilloma, myxoma, glyoma, inverted papilloma, antrochoanal polyp, dermoid cyst), malignant tumors of frontal sinus (osteosarcoma, meningoencephalocele, Gardner syndrome, orbital/retroorbital tumors).
Being mostly asymptomatic, frontal sinus osteomas grow and extend slowly, being able to cause various neurological and/or ophtalmological complications(10): CSF fistula, meningitis, epidural abcess, subdural empyema, cerebral abcess, cranial nerves paralysis, orbital celullitis, orbitar abcess, optic neuritis.
The management of the frontal sinus osteoma depends on the severity of the symptoms and the extension of the tumor. If the osteoma is discovered incidentally, being small sized and with a slow and silent evolution, then usually the “watch and wait” approach is preferred(11). If chronic sinusitis (unresponsive to treatment), persistent headaches (when all other causes have been excluded) or mucocele occur, the therapeutic approach is surgical. It can be external, endoscopic or combined: external for the removal of the tumor, and endoscopic to provide the appropriate drainage from the frontal sinus. The approach depends mostly on the site and dimension of the osteoma. Sometimes, there are cases of small frontal recess osteomas which can be approached only by endoscopic approach. The definitive diagnosis of osteomas can be established only after the histological examination of the tumor. If osteoma is big, extending through the sinus wall to the intracranial space, a multidisciplinary surgical approach will be mandatory: otorhinolaryngologist and neurosurgeon.
The postoperative complications which may occur are: subcutaneous emphysema, persistent suppurative sinusitis, fistulization, frontal osteomyelitis, supraorbitar nerve branches damage, supraorbitar neuralgia, ecchymosis, palpebral edema, dyplopia, epiphora, frontal recess stenosis, recurrence of frontal sinusitis, and tumoral recurrence.
Conclusions
Although osteomas of paransal sinuses are benign tumors, with a slow and silent growth, they need to be diagnosed in time and followed-up for the establishment of the proper therapeutic approach, depending on the symptoms and/or the complications that may appear.
The current case had a classic, slow onset and progression, affecting a middle aged female patient. The symtoms have occured gradually: progressive headache started 12 months before the admission to the hospital. The presumptive diagnosis was established after clinical and paraclinical examinations (transnasal endoscopy, native computed tomography of the head and paranasal sinuses). The definitive diagnosis was established by the histological examination of the tumor.
Considering the size of the tumor (4th grade, taking into consideration the classification of osteomas mentioned above), the decision regarding the therapeutic approach was taken and the combined approach surgery was performed: external and endoscopic, which allowed the ablation of the tumor, as well as proper postoperative drainage of frontal sinus.
Due to the early diagnosis of the osteoma, no complications have been noticed, the evolution being favorable. ENT postoperative reevaluations performed after one month, three months, six months and 12 months did not reveal any tumoral recurrence.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Celenk F, Baysal E, Karata ZA, Durucu C, Mumbuc S, Kanlikam M. Paranasal sinus osteomas. J Craniofac Surg. 2012; 23:e433–7.
- Georgalas C, Goudakos J, Fokkens WJ. Osteoma of the skull base and sinuses. Otolaryngol Clin North Am. 2011; 44:875– 90.
- Savastano M, et al. Head and Neck Medicine and Surgery. American Journal of Otolaryngology. 2007; 28: 427–429.
- Izci Y. Management of the large cranial osteoma: experience with 13 adult patients. Acta Neurochir (Wien). 2005 Nov; 147(11):1151-5; discussion 1155.
- Cokkeser Y, Bayarogullari H, Kahraman SS. Our experience with the surgical management of paranasal sinuses osteomas. Eur Arch Otorhinolaryngol. 2013; 270:123–8.
- Chiu AG, Schipor I, Cohen NA, Kennedy DW, Palmer JN. Surgical Decisions in the Management of Frontal Sinus Osteomas. American Journal of Rhinology. 2005; 19(2), 191–197.
- Nielse GP, Rosenberg AE. Update on Bone Forming Tumors of the Head and Neck. Head Neck Pathol. 2007 Sep; 1(1): 87–93.
- Castelnuovo P, Valentini V, Giovannetti F, Bignami M, Cassoni A, Iannetti G. Osteomas of the Maxillofacial District. Journal of Craniofacial Surgery. 2008; 19(6), 1446–1452.
- Bacalbaşa A. Cazuri rare în otorinolaringologie, Ed. Medic Art, Bucureşti, 2006.
- Turan Ş, Kaya E, Pınarbaşlı MÖ, Çaklı H. The Analysis of Patients Operated for Frontal Sinus Osteomas. Turk Arch Otorhinolaryngol. 2015 Dec; 53(4): 144–149.
- Turri-Zanoni M, Dallan I, Terranova P, Battaglia P, Karligkiotis A, Bignami M, Castelnuovo P. Frontoethmoidal and intraorbital osteomas: exploring the limits of the endoscopic approach. Arch Otolaryngol Head Neck Surg. 2012 May; 138(5):498-504.
Articole din ediţiile anterioare
Abordul endoscopic al osteomului de sinus frontal
Osteomul rinosinuzal este o patologie frecventă în practica ORL, cea mai comună localizare fiind la nivelul sinusului frontal. Adesea, osteoamele ...