The report describes one clinical case of gastroesophageal reflux disease (GERD) associated with worn dentition. The treatment plan includes conventional methods using conventional and modern restorative materials. Oral rehabilitation resulted in functional and esthetic devices with good prognosis in the development of GERD.
Tehnici convenţionale şi moderne în reabilitarea orală a pacienţilor cu boală de reflux gastroesofagian
Conventional and modern techniques in oral rehabilitation of patients with gastroesophageal reflux disease
First published: 01 martie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Orl.42.1.2019.2211
Abstract
Rezumat
Raportul descrie un caz clinic de boală de reflux gastroesofagian (GERD) asociat cu dentiţia uzată. Planul de tratament include metode convenţionale care utilizează şi materiale de restaurare, atât moderne, cât şi convenţionale. Reabilitarea orală a avut ca rezultat dispozitive funcţionale şi estetice cu o bună prognoză în evoluţia bolii de reflux gastroesofagian.
Gastroesophageal reflux disease (GERD) is a chronic disease, characterized by gastric stuff reflux determined by an inadequate relax of the inferior esophageal sphincter. There have been described plenty of risk factors involved in GERD: obesity, diet habits, hiatus hernia, smoking, physical exercises, sleep obstructive apnea, diabetes, slow stomach release, scleroderma, pregnancy, Zollinger-Ellison syndrome.
The most commonly described symptoms and complications are burning stomach, food acid reflux, dental erosions, esophageal constrictors, together with scar tissue formation, esophageal ulcer, painful deglutition, dry persistent cough during nights and asthma.
Countless medical studies have given us a lot of information about the correlations between dental erosions, sleep bruxism and GERD(1,2,3). Most of them come to the conclusion that dental erosion is the unique symptom in most patients. Therefore, the dentist may be the first one who has the opportunity to discover GERD.
Clinical case:
A 45-year-old female patient, with severe hard dental tissue loss.
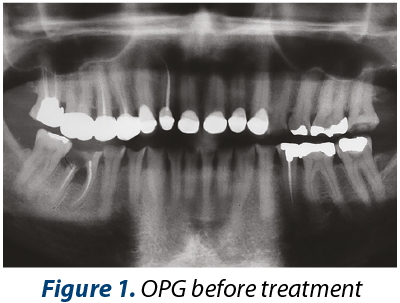



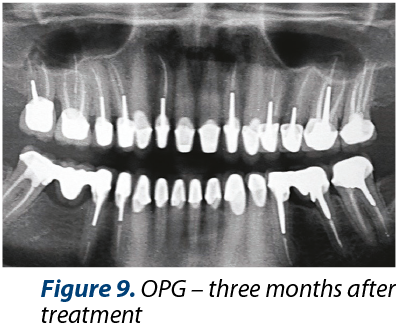
The medical history includes medium dietary controlled GERD. The main dental problems identified are: medium or severe dental loss (erosions, attrition), bad dental restorations, alveolar bone defect after 46 tooth extraction, inadequate anterior guidance, poor esthetics (Figures 2, 3 and 4). Orthopantomogrammes (OPG) were made before (Figure 1) and after (Figure 9) coronary and root treatments.


The final diagnosis included: general dental erosion due to GERD, malocclusion, low decay risk factor, class IV PDI (prosthetic dental index).
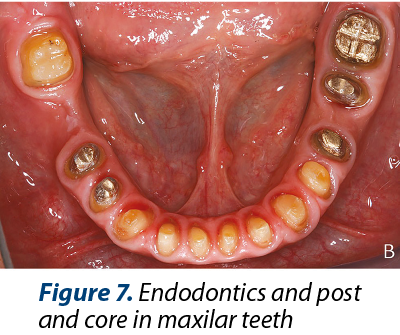

Treatment plan: GERD control, dental and periodontal health condition maintenance (Figure 6 and Figure 7), esthetic dental restorations.

Pre-prosthetic treatment included: dental occlusion analysis on a dental simulator, occlusion splint (Figure 5), occlusion vertical dimension rise with 2 mm, wax-up for esthetic and functional evaluation, temporary prosthesis.
Final treatment plan included:
-
Endodontic treatments with post and core in almost all present teeth.
-
Occlusion splint for rising occlusion vertical dimension.
-
Provisional prosthesis to test esthetics and function in the new therapeutic occlusion, following mutual protection occlusion principle.
-
Gingivectomy on teeth 11 and 21.
-
Premolarisation of tooth 36 (Figure 8).
-
Porcelain metal crowns 35, 36 and fixed dental prothetics (FPD) 47x45.
-
Protection maxillary splint.
-
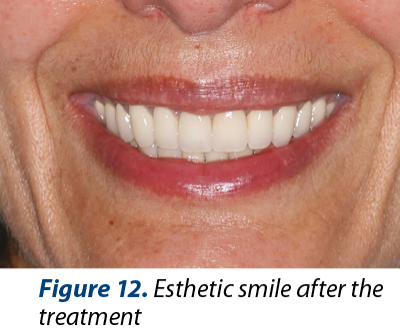
The esthetics was improved (Figures 10, 11 and 12) after the treatment due to rising the crowns heigt in 11 and 21 by gingivectomy and by modifing gingiva architecture in front arch.
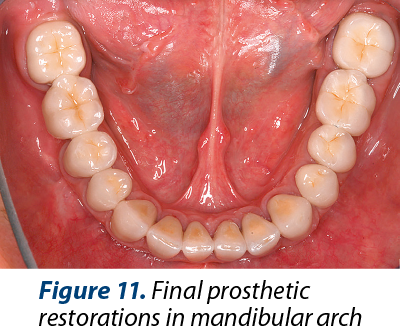
Figure 11. Final prosthetic restorations in mandibular arch
Conclusions
Dental erosions and attrition are common signs in patients with GERD and sleep bruxism.
The most important thing for a good prognosis of the treatment plan is to identify the factors involved in hard dental tissue loss before oral rehabilitation.
The patients with GERD and sleep bruxism have progressive dental loss lesions, and functional and esthetic disorders class IV diagnostic index.
Ussualy, the patients come in the latest stages of the hard tissue dental loss, needing most of the time complete oral rehabilitation.
The patient motivation, medical experience and finance are important.
Compliance with ethics requirements
The authors declare no conflict of interest regarding this article.
The authors declare that all the procedures and experiments of this study respect the ethical standards of the Helsinki Declaration from 1975, as revised in 2008, as well as the national law. The informed consent was obtained from the patient included in the study.
No funding for this study.
Bibliografie
- Marsicano JA, de Moura-Grec PG, Bonato RC, Sales-Peres M de C, Sales-Peres A, Sales-Peres SH. Gastroesophageal reflux, dental erosion, and halitosis in epidemiological surveys: a systematic review. Eur. Journal Gastroenterology Hepatol. 2013; 25:135-41.
- Gregory-Head BL, Curtis DA, Kim L, Cello J. Evaluation of dental erosion in patients with gastroesophageal reflux disease. J Prosthet Dent. 2000; 83:675-80.
- Ali DA, Brown RS, Rodriguez LO, Moody EL, Nasr MF. Dental erosion caused by silent gastroesophageal reflux disease. J Am Dent Assoc. 2002; 133:734-7.