Introduction. The aim of this study was to determine the frequency and management of complications of AOM and COM over a period of 15 years in E.N.T Clinic “Iuliu Haţieganu”, University of Medicine and Pharmacy Cluj-Napoca, and to discuss the new concept in their treatment.
Methods. Between January 2001 to December 2015, patients admitted to E.N.T. Department, “Iuliu Haţieganu” University of Medicine and Pharmacy Cluj-Napoca, with the diagnosis of otitis media and an associated intratemporal or intracranian complication were analyzed retrospectively. The overall incidence of all complications and of each complication individually was determined.
Results. A total of 930 patients were diagnosed with otitis media. Complications of otitis media were diagnosed in 35 patients; thus, the incidence of complications was 3.37%. We identified 27 (2.9%) intratemporal complications and 8 (0.86%) intracranial complications. The most frequent complication was labyrinthine fistula in 13 (1.39%) patients.
Conclusion. The incidence of otitis complications remains significant in our department. Chronic otitis media with cholesteatoma is the most frequent etiology of complications. Labyrinthine fistula is the most common complication of otitis media.
Tendințele actuale în managementul complicațiilor intracraniene ale otitelor medii
Current opinions in the management of otitis media complications
First published: 10 martie 2016
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Orl.30.1.2016.649
Abstract
Rezumat
Introducere. Scopul acestui studiu a fost analizarea frecvenței de apariție a complicațiilor asociate otitelor medii, pe o durată de 15 ani, în Clinica ORL a Universității de Medicină și Farmacie „Iuliu Hațieganu”, Cluj-Napoca, precum și prezentarea unor noi tendințe în ceea ce privește abordarea terapeutică a acestora.
Metode. S-a efectuat un studiu retrospectiv pe un număr de 930 de pacienți internați cu diagnosticul de otită medie în Clinica ORL, Universitatea de Medicină și Farmacie „Iuliu Hațieganu”, Cluj-Napoca, și care au asociat o complicație.
Rezultate. Complicații ale otitei medii au apărut la un număr de 35 de pacienți din totalul de 930 diagnosticați cu otită medie, incidența acestora fiind de 3,37%. 27 (2,9%) dintre pacienți au prezentat complicații intratemporale, iar 8 pacienți (0,86%) au prezentat complicații intracraniene. Cea mai frecventă complicație a fost fistula labirintică, prezentă la un număr de 13 pacienți (1,39%).
Concluzii. Incidența complicațiilor otitei medii rămâne semnificativă în serviciul ORL. Otita medie supurată cu colesteatom reprezintă etiologia cea mai frecventă pentru apariția complicațiilor. Fistula labirintică este cea mai frecventă complicație a otitelor medii.
Introduction
The incidence of complications tributary to acute otitis media (AOM)/cronic otitis media (COM) has decreased in the last decade(1). This phenomenon occurred due to increased health care accessibility and advancement in imaging and antibiotic therapy, particularly in developed countries. Nevertheless, in developing countries the complications remain quite frequent, with high morbidity and mortality rates. The differences persist, so that its incidence in developing countries is as high as 0.5-3% and is common in children with low socioeconomic status(2), compared to industrialised countries, for instance Finland, where a study found a 0.004% incidence of complications(3). When it comes to statistics, the reporting results concerning the complications incidence must be carefully interpreted because some articles present the incidence of complications for both AOM and COM and others make a distinction between them.
However, in large series of patients, nearly 80% of extracranial complications and 70% of intracranial complications occurred in children in the first 2 decades of life and 58% were present in patients younger than 20 years(4), as a consequence of AOM that it is the most common bacterial infection of childhood. An estimated 85% of all children experience at least one episode of AOM(5). The patterns of complications are different in AOM versus COM. With AOM, complications occur as a result of associated bacteremia and develop by hematogenous dissemination or by direct extension along preformed pathways. In COM, bacteria gain access to the involved structures most commonly by direct erosion of bone, hematological, propagating along veins, through anatomical pathways and previous surgical or non surgical trauma(6,7).
Regarding COM, a specification has to be underscored. It is well known that chronic suppurative otitis media is classified into two main categories: COM without or with cholesteatoma. The former is considered ‘safe’ regarding its complications, while the latter has been considered a ‘dangerous’ form of disease because of the risks of otogenic complications(8). Although COM with cholesteatoma leads to more frequent complications, there are studies in the literature describing complications in COM without cholesteatoma especially in granulating form of disease(9,10).
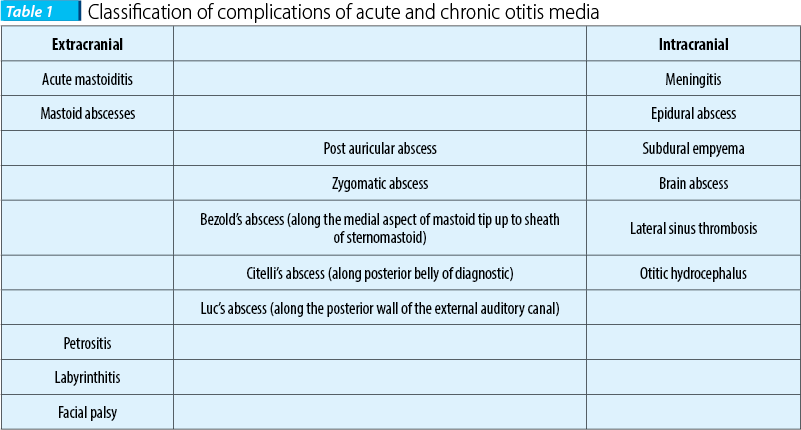
Classically, the complications of otitis media (AOM and COM) are classified into extracranial (intratemporal) and intracranial, as seen in Table 1.
Referring to cholesteatoma complications, there are presented in literature some unusual ones: distant abscesses (parapharyngeal, retropharyngeal abcesses), jugular foramen syndrome, trigeminal neuralgia, secondary malignancies of the temporal bone and the facial nerve, osteomyelitis or fibrous dysplasia of the temporal bone. This study was designed to determine the frequency and management of complications of AOM and COM over a period of 15 years in E.N.T. Clinic of “Iuliu Haţieganu” University of Medicine and Pharmacy, Cluj-Napoca, and to discuss the new concept in their treatment.
Method
The charts of 930 operations for acute and cronic otitis media performed from January 2001 to December 2015 at the Department of Otorhinolaryngology - Head and Neck Surgery, “Iuliu Haţieganu” University of Medicine and Pharmacy, Cluj-Napoca, were analyzed retrospectively. Only the cases with intratemporal and intracranial complications were included in the study. The following data were collected from medical records: age, gender, medical history, type of middle ear infection, associated complications, associated pathology, audiometry and imaging test results. All patients received antibiotic therapy and systemic corticosteroids. The design of this study was aproved by the local ethical committee of the Department of Otorhinolaryngology, University of Cluj-Napoca. The following were reasons for exclusion from the study: no postoperative follow-up, inaccessible records, patients with limited attic, sinus tympani or mesotympanic cholesteatoma.
Results
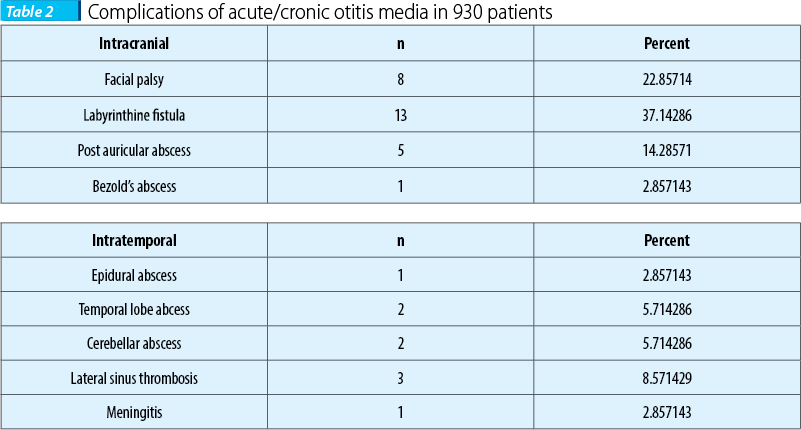
A total of 35 (3.76%) patients out of 930 diagnosed with complications associated with otitis media were identified. The average age for patients included in the study was of 41±6.5 years (95% CI [39.32-42.85]). There were 27 (2.9%) intratemporal complications: facial palsy in 8 (0.86%) patients; labyrinthine fistula in 13 (1.39%) patients; post auricular abscess in 5 (0.53%) patients; Bezold’s abscess in 1 (0.1%) patient and 8 (0.86%) intracranial complications: epidural abscess in 1 (0.1%) patient; temporal lobe abcess in 2 patients (0.21%); cerebellar abscess in 2 (0.21%) patients; lateral sinus thrombosis in 3 patients (0.32%) and meningitis in 1 (0.1%) patient. A patient died from a subdural empyema.
Otitis media was classified as follows: chronic otitis media with cholesteatoma in 23 patients (65.7%); chronic otitis media without cholesteatoma - granulating form in 4 patiens (11.4%) and acute otitis media in 5 patients (0.53%).
Discussion
Complications from chronic ear infections are decreasing because of earlier diagnosis and initiation of appropriate treatments. However, chronic ear infections can still cause intracranial and extracranial complications(11,12). Our study refers to 35 cases of complications occurred with OM (AOM and COM) presented in the E.N.T. Clinic of Cluj-Napoca over a 15-year period. These data reflect a frequency of 3.76% (2.9% intratemporal and 0.86% intracranian).
From these 35 cases, only 9 (0.3%) cases occurred in the last five years, versus 26 cases in the first 10 years (4.02%). Statistics show different results, but in general approximately 5% of patients with cholesteatomatous chronic otitis media develop complications(1).
Facial nerve palsy
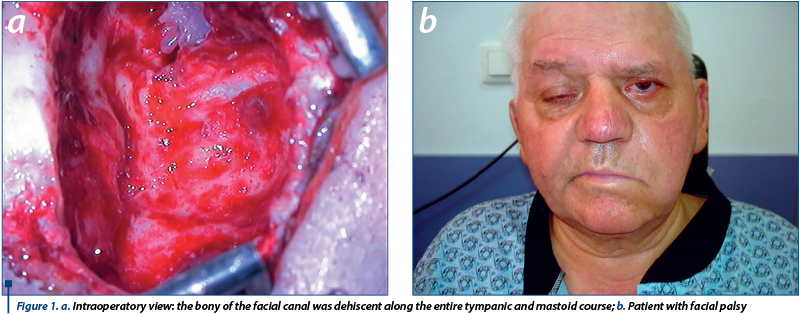
Facial nerve paralysis is an infrequent but serious complication of otitis media (OM), about 0.16% to 5.1%(13,14), and it has a threatening effect on the patient. External compression, bone erosion, osteitis, edema and inflammation of the nerve are some of the proposed etiologic factors(15). Our study comprised a number of 8 cases of OM associated with facial palsy, 0.8% of all cases. Cholesteatoma was found in 4 cases (50%) and granulating otitis media in the remaining 4 cases. Chronic otitis media causing facial nerve paralysis is the most frequent, due to cholesteatoma, and there are some reports in literature showing cholesteatoma involvement in 69-70% of otitis media cases(14,16). Complete eradication of cholesteatoma and facial nerve decompression or repair is the procedure to be chosen for the recovery of the nerve function. Controversies exist in the literature regarding the surgical technique (canal wall up versus canal wall down procedure) and the extent of facial nerve decompression. Some authors prefer bony decompression from the geniculate ganglion to the stylomastoid foramen, and incising the epineurium of the nerve(14). We generally performed CWD procedure with careful removal of the cholesteatoma matrix. The opening of the canal was limited to the smallest area possible, which was with facial nerve edema or redness. This was in agreement with other studies(14). Prognosis for facial paralysis was relatively good in our series of cases. The outcomes of surgical interventions were closely related to the duration between onset and surgery. Two patients with very recent facial palsy exhibited normal facial function within 3-4 days and two patients within 5-6 months postoperatively. One of the patients was referred to our clinic with facial palsy lasting for one month, and in one case there was an advanced cholesteatoma with intratemporal extension. Intrasurgically we found that the bony of the facial canal was dehiscent along the entire tympanic and mastoid course (Figure 1).
Chronic granulative otitis media was also observed in four patients. These cases presented an associated pathology. One case with tuberculous otitis media was a 3-year-old child who presented normal facial function after tuberculostatic treatment and in the other case we performed facial reconstruction with great auricular nerve graft. Two patients were elderly with other major comorbidities such as diabetes and chronic hemodialysis and they showed no improvement beyond House-Brackmann grade II 1-year following surgery.
The possible mechanism for facial palsy in these cases could be the infection that causes compression to the vessels that nourish the facial nerve, which could cause local ischemia and nerve infarction or a direct involvement of the nerve, through bacterial or viral toxins(17).
Labyrinthine fistula
Labyrinthine fistulas may be associated with COM with and without cholesteatoma and also with granulating otitis media. Labyrinthine fistula incidence varies from 4% to 15%(18,19).
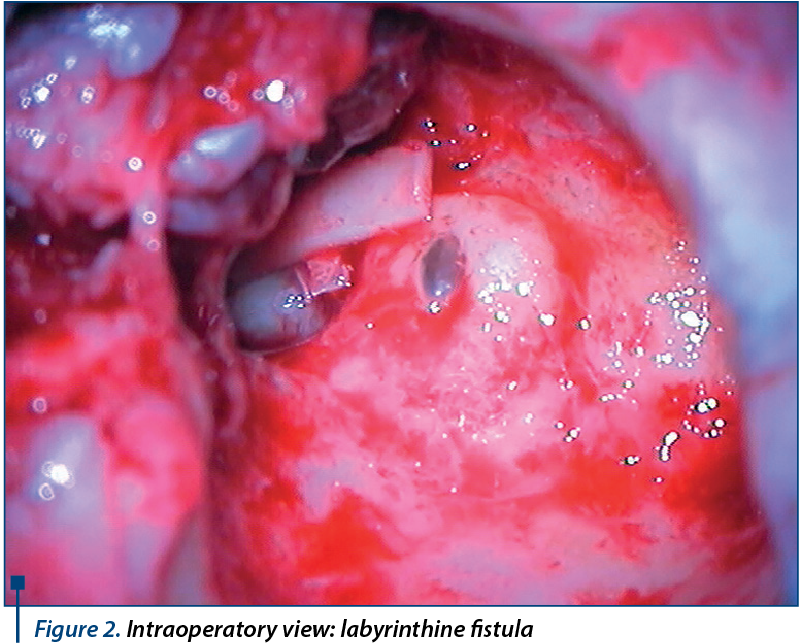
In our series of patients, labyrinthine fistula was the most frequent complication, representing 13.9% . There are different opinions in literature regarding the management of labyrinthine fistulas: some authors initially prefer to leave the matrix in place and remove it later during a preplanned second stage procedure 6 months after the first operation, while others remove the matrix from the beginning(20). We prefer an open tympanoplasty and removal of the cholesteatoma matrix whenever possible. The bony defect is than covered with bone pate, temporalis muscle fascia and conchal cartilage (Figure 2). We prefer this procedure because we usually perform open tympanoplasty with obliteration of the mastoid cavity. We did not observe changes in postoperative bone conduction using this procedure. Neverthless, in cases with only one hearing ear, with a fistula larger than 2 mm, an open technique is indicated with matrix preservation(21,22).
Meningitis
Meningitis can develop by hematogenous spread, through bony erosion, preformed channels and direct extension(23). Although meningitis is considered to be one of the most common intracranial complications of COM with cholesteatoma, we have encountered just one case in our series of patients. This can be the lack of our study. Our department is specialized in adult cases and children are seldom referred to our clinic. High dose antimicrobial therapy and intravenous corticosteroid therapy produce favorable prognosis in the majority of cases(24). A radical surgery for cholesteatoma removal must be performed as soon as the patient is neurologically stable. In our institution, the initial treatment for the patient is performed at the Infectious Disease Department.
Intracranial abscess
It is well known that the most common cause of abscesses in the temporal lobe and cerebellum is chronic ear infection(25). We encountered one case with epidural abscess which was treated using transmastoid excision, one temporal lobe abcess that was urgently treated by a neurosurgeon using bur-hole aspiration, and in two cases of cerebellar abscess in which a craniotomy-like procedure was performed. There was a small temporal lobe abcess (<1 cm) in which a conservative management was followed regarding the neurosurgical procedure and the case was successfully treated by intravenous antibiotics alone. Antibiotic therapy can also be helpful in cases of focal cerebritis stage(26). Concerning cholesteatoma, surgery has to be done at the earliest opportunity for eradication of the disease in any cases when the patient is neurologically stable(27). One of our patients died due to temporal lobe abcess complicated with subdural empyema. The reason was that, unfortunately, the patient presented to our department in the late stage of the disease. Although rarely seen in recent years, mortality remains between 0 and 31% so the follow-up should be very strict every 2 weeks for 6 weeks(28,29).
Lateral sinus thrombosis
Lateral sinus thrombosis incidence has markedly decreased, but mortality is still high(30).
In our series of patients there were three cases, two cases were associated with cholesteatoma and one case was a child who presented with acute otitis media. Thrombosis of the lateral sinus (LST) usually forms as an extension of a perisinus abscess that develops after mastoid bone erosion from cholesteatoma, granulation tissue, or coalescence(31,32). This form is most common in adults or in older children with cholesteatoma, and less common than other types of chronic mastoiditis. Subsequently, adherence of fibrina, blood cells and platelets can produce a mural thrombus. The persistence of the inflammation and the increase in thrombus volume might result in an obliterative LST. In the early course of acute otitis media, LST can be caused also by an osteothrombophlebitis phenomen; if this is the case, the sigmoid bony sinus plate will be intact at the time of surgical exploration(33). All patients with sigmoid sinus thrombosis require early mastoidectomy to treat the underlying mastoid disease adequately. Management of the clot can involve anticoagulation, ligation of the jugular vein in the neck, and opening the sinus and evacuating the infected clot. But if free blood is aspirated, then no further intervention is required(34). Use of anticoagulants is rarely indicated, but anticoagulation should be strongly considered when extension of the clot to the transverse sinus or cavernous sinus is suspected or documented. In the past, routine ligation of the jugular vein in the neck was performed. Currently, this procedure seems unnecessary, but it should be taken into account whenever there is evidence of extension of the clot into the neck, and should be strongly considered when septic emboli are present(35). In all our cases we performed canal wall down procedure, we opened the lateral sinus and evacuated the infected thrombus (Figure 3). Only one case required ligation of the jugular vein in the neck.

Conclusion
Complications of otitis media still exist and represent a challenging task for the E.N.T. specialists. These complications can be managed successfully if diagnosed promptly and appropriately, with adequate medications or meticulous surgery.
Key Points:
Facial nerve palsy - is not a contraindication for reconstruction of the hearing.
Labyrinthine fistula - cholesteatoma matrix can be removed on the fistula regardless its size and tympanoplasty canal wall up/down procedure can be performed.
Intracranial abscess - the abcess should be drained via mastoid whenever possible.
Lateral sinus thrombosis - prognosis is not improved by sinus incision.
Bibliografie
2. Lin YS, Lin LC, Lee FP, Lee KJ. The prevalence of chronic otitis media and its complication rates in teenagers and adult patients. Otolaryngol Head Neck Surg 2009; 140(2):165–170.
3. Leskinen K, Jero J. Acute complications of otitis media in adults. Clin Otolaryngol 2005; 30(6):511-516.
4. Osma U, Cureoglu S, Hosgoglu S: The complications of chronic otitis media: report of 93 cases. J Laryngol Otol 2000; 114:97–100.
5. Gates GA: Acute otitis media and otitis media with effusion. In: Cummings CW, ed. Otolaryngology - Head and Neck Surgery, 1998 3rd ed. St Louis: Mosby-Year Book.
6. Singh M, Jain S, Rajput R, Khatua RK, Sharma D. Retrospective and prospective study of Singapore swing method on healing of mastoid cavity. Indian J Otolaryngol Head Neck Surg 2010; 62:365–71.
7. O’Connor TE, Perry CF, Lannigan FJ. Complications of otitis media in Indigenous and non-Indigenous children. Med J Aust 2009; 191:60–4.
8. Matanda, R. N., Muyunga, K. C., Sabue, M. J., Creten, W. & Van de Heyning, P. Chronic suppurative otitis media and related complications at the University Clinic of Kinshasa. B-ENT (2005)1, 57–62.
9. Mostafa, B. E., El Fiky, L. M. & El Sharnouby, M. M. Complications of suppurative otitis media: still a problem in the 21st century. ORL J Otorhinolaryngol Relat Spec (2009). 71, 87–92.
10. Agrawal S, Husein M, MacRae D. Complications of otitis media: an evolving state. J Otolaryngol. 2005 Jun; 34(Suppl 1):S33–S39.
11. Yorgancılar E, Yildirim M, Gun R, Bakir S, Tekin R, Gocmez C, et al. Complications of chronic suppurative otitis media: a retrospective review. Eur Arch Otorhinolaryngol. 2013 Jan; 270(1):69–76.
12. Quaranta N, Cassano M, Quaranta A. Facial paralysis associated with cholesteatoma: a review of 13 cases. Otol Neurotol 2007; 28:405–407.
13. Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S. Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J Laryngol Otol 1993; 107: 999-1004.
14. Ikeda M, Nakazato H, Onoda K, et al. Facial nerve paralysis caused by middle ear cholesteatoma and effects of surgical intervention. Acta Otolaryngol 2006; 126:95–100.
15. Yetiser S, Tosun F, Kazkayasi M. Facial nerve paralysis due to chronic otitis media. Otol Neurotol 2002; 23:580-8.
16. Savić DL, Djerić DR. Facial paralysis in chronic suppurative otitis media. Clin Otolaryngol Allied Sci 1989; 14:515-7.
17. Telischi FF, Chandler JR, May M, Schaitkin BM. Infection: Otitis media, cholesteatoma, necrotizing external otitis, and other inflammatory disorders. The Facial Nerve. 2000; 20:383-92.
18. Copeland BJ, Buchman CA. Management of labyrinthine fistulae in chronic ear surgery. Am J Otolaryngol 2003; 24:51–60.
19. Moon IS, Kwon MO, Park CY, et al. Surgical management of labyrinthine fistula in chronic otitis media with cholesteatoma. Auris Nasus Larynx 2012; 39:261–264.
20. Ghiasi S. Labyrinthine fistula in chronic otitis media with cholesteatoma. J Pak Med Assoc 2011; 61:352–355.
21. Sanna M, Sunose H, Mancini F, et al. Middle ear and mastoid microsurgery. 2nd ed. Stuttgart: Georg Thieme Verlag; 2012; pp. 449–455.
22. Sanna M, Zini C, Gamoletti R, et al. Closed versus open technique in the management of labyrinthine fistulae. Am J Otol 1988; 9:470–475.
23. Yorgancilar E, Yildirim M, Gun R, et al. Complications of chronic suppurative otitis media: a retrospective review. Eur Arch Oto-rhino-laryngol 2013; 270:69–76.
24. Lebel MH, Freij BJ, Syrogiannopoulos GA, et al. Dexamethasone therapy for bacterial meningitis. Results of two double-blind, placebo-controlled trials. N Engl J Med 1988; 319:964–971.
25. Morwani KP, Jayashankar N. Single stage, transmastoid approach for otogenic intracranial abscess. J Laryngol Otol 2009; 123:1216–1220.
26. Sennaroglu L, Sozeri B. Otogenic brain abscess: review of 41 cases. Otolaryngol Head Neck Surg 2000; 123:751–755.
27. Penido Nde O, Borin A, Iha LC, et al. Intracranial complications of otitis media: 15 years of experience in 33 patients. Otolaryngol Head Neck Surg 2005; 132:37–42.
28. GB, Wanna Dharamsi LM, Moss JR, et al. Contemporary management of intracranial complications of otitis media. Otol Neurotol 2010; 31:111–7.
29. Morwani KP, Jayashankar N. Single stage, transmastoid approach for otogenic intracranial abscess. J Laryngol Otol 2009; 123:1216–1220.
30. García González LA, López Aguado D. Lateral sinus thrombosis due to cholesteatoma. Report of a case and literature review. An Otorrinolaringol Ibero Am. 2005; 32 (6):527-36.
31. Seven H, Ozbal AE, Turgud S. Management of otogenic lateral sinus thrombosis. Am J Otolaryngol 2004; 25:329-33.
32. Bradley DT, Hashisaki GT, Mason JC. Otogenic sigmoid sinus thrombosis: what is the role of anticoagulation? Laryngoscope 2002; 112:1726-9.
33. Kaplan DM, Kraus M, Puterman M, et al. Otogenic lateral sinus thrombosis in children. Int J Pediatr Otorhinolaryngol 1999; 49:177–183.
34. Kuczkowski J, Mikaszewski B. Intracranial complications of acute and chronic mastoiditis: report of two cases in children. Int. J. Pediatr Otorhinolaryngol 2001; 60:227–237.
35. Syms MJ, Tsai PD, Holtel MR: Management of lateral sinus thrombosis. Laryngoscope 1999; 109: 1616-1620.
Articole din ediţiile anterioare
Interferenţe pediatrico-otorinolaringologice
Pediatrul colaborează frecvent cu ORL-istul pentru îngrijirea copiilor cu boli ale căilor respiratorii superioare: diagnosticul unor complicaţii al...
Tromboza sinusului venos lateral
Tromboza sinusului venos lateral (TSL) poate să apară ca o complicaţie intracraniană a otitei medii. În era preantibiotică, mortalitatea e...
Otomastoidită cervicală Bezold - caz clinic
Otomastoidita cervicală Bezold a devenit o patologie rar întâlnită în otologie, ca urmare a utilizării pe scară largă a antibioticelor. Autorii pre...
Empiem subdural de origine otogenă – caz clinic
Empiemul subdural reprezintă o colecţie purulentă localizată între dura mater şi arahnoidă. Acesta apare, cel mai adesea, ca o complicaţie a unei i...