Schimbare de paradigmă în MIS-C – cazul unei furtuni perfecte
Paradigm shift in MIS-C – the case of a perfect storm
Abstract
Acute renal infarction in pediatric patients is a rare occurrence, usually associated with cardiac anomalies, hypercoagulable state, diseases with local thrombotic potential, systemic infections, or autoimmune diseases. Following the COVID-19 pandemic, the medical scientific community established diagnostic criteria for PIMS-TS (Pediatric Inflammatory Multisystem Syndrome – temporally associated with SARS-CoV-2), also known as multisystem inflammatory syndrome in children (MIS-C), a condition found in children exposed to the new type of coronavirus. Three clinical phenotypes have been established: toxic shock syndrome, Kawasaki-like disease, and undefined inflammatory presentation. Cardiovascular manifestations were considered prominent in all clinical scenarios, while renal and neurologic involvement played a secondary role. There is, however, mounting evidence suggesting that MIS-C is in fact a miscellaneous pathology and that a focus change is warranted.Keywords
acute renal infarctionCOVID-19multisystem inflammatory syndrome in childrenRezumat
Infarctul renal acut la copii şi adolescenţi este un eveniment rar, asociat de obicei cu anomalii cardiace, cu status hipercoagulant, boli cu potenţial trombotic local, infecţii sistemice sau cu boli autoimune. În urma pandemiei de COVID-19, comunitatea ştiinţifică medicală a stabilit criterii de diagnostic pentru PIMS-TS (Pediatric Inflammatory Multisystem Syndrome – asociat temporal cu SARS-CoV-2), cunoscut şi sub numele de sindrom inflamator multisistemic la copii (MIS-C), o afecţiune regăsită la copiii expuşi la noul tip de coronavirus. Au fost stabilite trei fenotipuri clinice: sindrom de şoc toxic, boală Kawasaki-like şi patologie inflamatorie nespecifică. Manifestările cardiovasculare au fost considerate dominante în toate scenariile clinice, în timp ce implicarea renală şi neurologică a jucat un rol secundar. Există totuşi dovezi tot mai multe care sugerează că MIS-C este de fapt o patologie diversă şi că o schimbare a focalizării este justificată.Cuvinte Cheie
infarct renal acutCOVID-19sindrom inflamator multisistemic la copiiIntroduction
As of 2022, requests and recommendations for unified guidelines for the diagnosis and management of multisystem inflammatory syndrome in children (MIS-C) cases have emerged(1-3). Previous data focused on the cardiac manifestations of this new syndrome and on the improvement of the systemic inflammatory response, with variations in the treatment recommendations aimed at the administration of antivirals, antibiotics and anticoagulants.
However, recent case reports and in-depth analysis of immunologic and pathophysiologic aspects of the SARS-CoV-2 infections in children led to a better understanding of this multifaceted disease and its systemic implications. This paper presents a new phenotype that may emerge in the MIS-C scenario, focusing on the underlying causes and differential diagnosis problems that may occur.
Case presentation
A 7-year-old female patient, with no prior history of any disease, was admitted to the cardiac intensive care unit for fever (38.5°C), frontal headache, two episodes of generalized tonic-clonic seizures, lasting one minute each, and high blood pressure (SBP=190 mmHg, DBP=80 mmHg). Her symptoms developed 12 hours prior to hospital admission.
Biological tests showed inflammatory syndrome, high D-dimers, leukocytosis, neutrophilia, microcytic hypochromic anemia, and thrombocytosis.
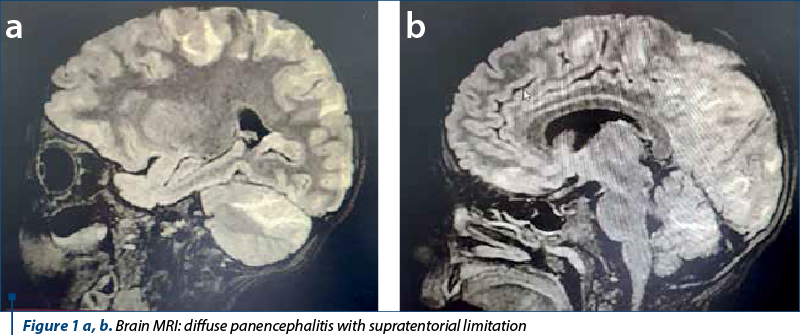
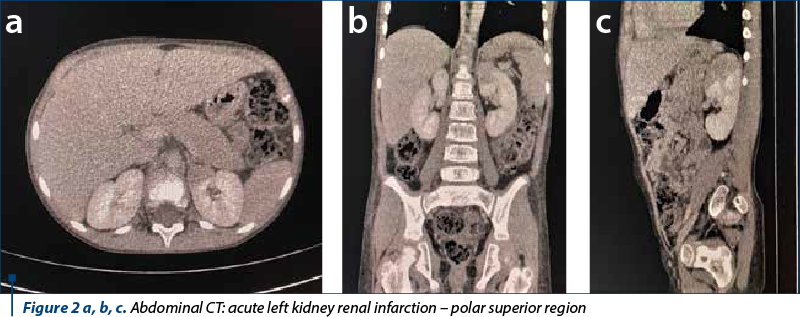
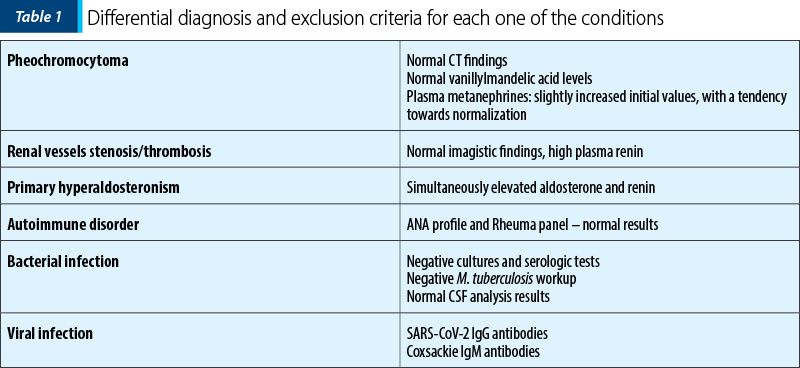
No structural or functional anomalies were diagnosed by echocardiography, EKG or Holter EKG monitoring. Brain MRI was performed, which identified panencephalitis lesions, with supratentorial limitation (Figure 1 a and b). The abdominal CT revealed acute renal infarction involving the superior polar segment of the left kidney, with no other visceral or vascular anomalies (Figure 2 a, b and c). The differential diagnosis followed three directions: renal hypertension, systemic infection, and autoimmune disease. We eliminated each supposition based on imagistic and biological findings (Table 1).
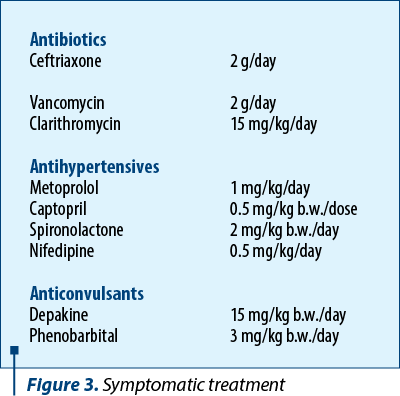
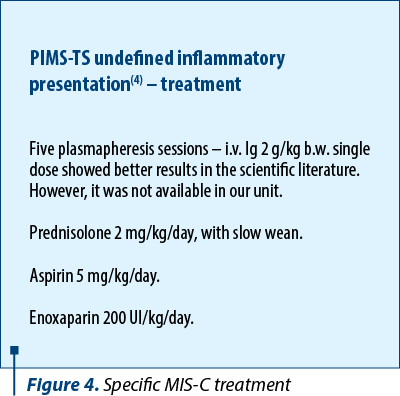
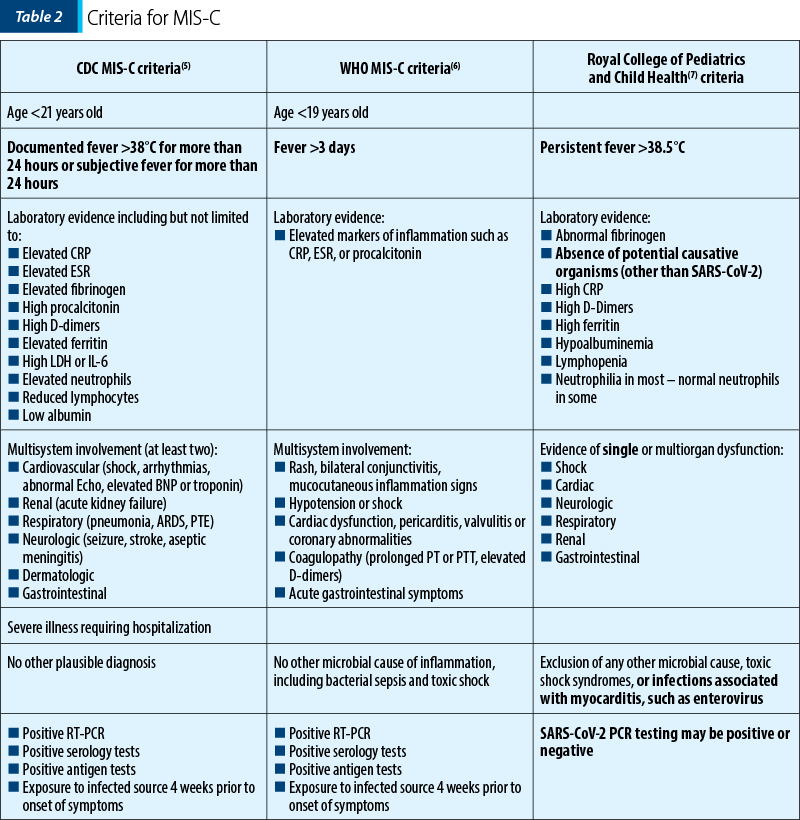
We diagnosed our patient with multisystem inflammatory syndrome in children, based on the case definition and diagnostic criteria established by Centers for Disease Control and Prevention (CDC) – Table 2. As such, she received cardioactive drugs, anticonvulsants, antibiotics, and the established course of treatment for undefined inflammatory presentation type – PIMS-TS(4) (Pediatric Inflammatory Multisystem Syndrome – temporally associated with SARS-CoV-2) (Figures 3 and 4).
Our patient slowly improved with the medical treatment described above, and she was discharged one month after the initial admission, requiring only metoprolol and nifedipine as antihypertensive medications, and Depakine® for seizure prevention. Monthly follow-ups showed significant improvement in both neurologic and cardiologic functions, with grade I hypertension as the sole sequelae. The patient exhibited significant hematuria for another three months after hospital discharge. DMSA scintigraphy confirmed healed renal infarction with normal renal function.
Discussion
Inflammatory status after SARS-CoV-2 infection
The diagnostic criteria of the multisystemic inflammatory syndrome in children after the exposure to SARS-CoV-2 as established by Center for Disease Control, World Health Organization (WHO) and The Royal College of Pediatrics and Child Health (RCPCH) show notable differences which prove important in current practice (Table 2).
Our patient met six out of the six CDC criteria for MIS-C. Currently, there are debates in the medical world regarding the need to establish unique diagnostic criteria for MIS-C(1-3,8), which should not be too inclusive (as it is the case of the RCPCH case definition, which considers a patient a PIMS-TS case regardless of the serological status or the PCR results), nor should it allow for the elimination of cases based on a viral coinfection.
The percentage of pediatric SARS-CoV-2 viral coinfection ranges between 10% and 51%, the most commonly involved pathogens being rhinovirus, enterovirus, adenovirus and respiratory syncytial virus. There is also a specific antibody response pattern for SARS-CoV-2 in children, which translates into a predominance of IgG antibodies for the S and not for N protein, independent of the clinical syndrome, and a lack of correlation between IgM antibodies and symptom onset, meaning decreased serological neutralizing action(9-11).
In our case, the multisystem involvement included neurologic disease manifested through seizure and MRI documented encephalitis. Coxsackie virus infection could have explained the neurological phenomena and the inflammatory syndrome. However, brain MRI modifications associated with Coxsackie infection usually involve the infratentorial regions(12,13). Moreover, the clinical picture and the laboratory evidence were highly suggestive for MIS-C, leaving no other plausible diagnosis.
Multisystem involvement
An interesting aspect of our case is the way in which the multisystem damage occurred. MIS-C is cited as a major cause of cardiovascular dysfunction that can range from cardiogenic shock to Kawasaki-like manifestations or cardiac conduction disorders. Our patient, despite severe neurological and renal symptoms, showed systemic hypertension (HTN) as the only involvement of the cardiovascular system. We excluded other known causes of HTN by means of imagistic, endocrine, nephrologic and cardiologic investigations, leaving neurogenic hypertension as the most probable pathogenesis. The presence of neuronal ACE2 facilitates viral neurotropism, leading to increased levels of chemokines, cytokines and ROS, which in turn impact baroreceptor activity, causing hypertension(14).
ACE2 has also been involved as a facilitating factor for acute renal failure in patients with MIS-C, alongside remnant immune dysregulation and hypercoagulable status. There are other similar reports of children with PIMS-TS who were diagnosed with renal infarction or acute kidney disease. The latter is cited in previously healthy children, with no favorable genetic background or pathologic history, while the former has been diagnosed in patients with thrombophilia or congenital cardiac disease(15-17).
There is also mounting evidence suggesting the impact of SARS-CoV-2 on the endocrine system. The stress response triggered by the viral infection leads to increased levels of metanephrines, which could be mistaken as signs of pheochromocytoma, as it was the case with our patient(18).
Conclusions
MIS-C is a new pathological entity that was mostly linked to severe cardiovascular manifestations. However, recent evidence suggests a paradigm shift. Renal and neurological damage becomes an important aspect in the spectrum of disease manifestations, a fact that should be known by pediatricians, especially since imaging and laboratory tests can be misleading, causing a delay in positive diagnosis and the late initiation of the appropriate treatment.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Algarni AS, Alamri NM, Khayat NZ, et al. Clinical practice guidelines in multisystem inflammatory syndrome (MIS-C) related to COVID-19: a critical review and recommendations. World J Pediatr. 2022;18(2):83–90.
-
Santos MO, Gonçalves LC, Silva PAN, Moreira ALE, Ito CRM, Peixoto FAO, Wastowski IJ, Carneiro LC, Avelino MAG. Multisystem inflammatory syndrome (MIS-C): a systematic review and meta-analysis of clinical characteristics, treatment, and outcomes. J Pediatr (Rio J). 2022;98(4):338-349.
-
Rhys-Evans S. Call for a universal PIMS-TS/MIS-C case definition. Archives of Disease in Childhood. 2022;107(3):e10.
-
Schlapbach LJ, Andre MC, Grazioli S, et al. Best Practice Recommendations for the Diagnosis and Management of Children with Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2 (PIMS-TS; Multisystem Inflammatory Syndrome in Children, MIS-C) in Switzerland. Front Pediatr. 2021;9:667507.
-
Centers for Disease Control and Prevention. HAN Archive – 00432. Health Alert Network (HAN). Available: https://emergency.cdc.gov/han/2020/han00432.asp
-
World Health Organization. Scientific brief: multisystem inflammatory syndrome in children and adolescents with COVID-19. Available from: https://www.who.int/publications/i/item/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19
-
RCPCH. Paediatric multisystem inflammatory syndrome temporally associated with COVID-19 (PIMS) – guidance for clinicians. Available from: https://www.rcpch.ac.uk/resources/paediatric-multisystem-inflammatory-syndrome-temporally-associated-covid-19-pims-guidance
-
Sarkar M, Pal P, Raychaudhuri D, Sen B, Roychowdhoury S, Chattopadhyay A, Hazra A, Mondal R. PIMS-TS vs. MIS-C: Diagnostic Criteria in COVID-19-Associated Hyperinflammation in Children. Indian J Pediatr. 2021;88(11):1149-1150.
-
Zhang DD, Acree ME, Ridgway JP, Shah N, Hazra A, Ravichandran U, Kumar M. Characterizing coinfection in children with COVID-19: A dual center retrospective analysis. Infect Control Hosp Epidemiol. 2021;42(9):1160-1162.
-
Karaaslan A, Çetin C, Akin Y, Demir Tekol S, Söbü E, Demirhan R. Coinfection in SARS-CoV-2 Infected Children Patients. J Infect Dev Ctries. 2021;15(6):761-765.
-
Weisberg SP, Connors TJ, Zhu Y, et al. Distinct antibody responses to SARS-CoV-2 in children and adults across the COVID-19 clinical spectrum. Nat Immunol. 2021;22(1):25–31.
-
Fan YK, Liu YP. Magnetic Resonance Imaging Features of Pediatric Coxsackievirus Encephalitis. J Belg Soc Radiol. 2019;103(1):6.
-
Lindan CE, Mankad K, Ram D, Kociolek LK, Silvera VM, Boddaert N, Stivaros SM, Palasis S; ASPNR PECOBIG Collaborator Group. Neuroimaging manifestations in children with SARS-CoV-2 infection: a multinational, multicentre collaborative study. Lancet Child Adolesc Health. 2021;5(3):167-177
-
Kulkarni PG, Sakharkar A, Banerjee T. Understanding the role of nACE2 in neurogenic hypertension among COVID-19 patients. Hypertens Res. 2022;45(2):254–269.
-
Plouffe B, Van Hooren T, Barton M, Nashid N, Demirkaya E, Norozi K, Rachinsky I, Delport J, Knauer M, Tole S, Filler G. Renal Infarcts – A Perplexing Case in the Middle of the COVID-19 Pandemic. Front Pediatr. 2021;9:669453.
-
Lee M, Hilado M, Sotelo S, Opas LM, Im DD. Acute Kidney Injury in Multisystem Inflammatory Syndrome in Children (MIS-C): A Case Report. SN Compr Clin Med. 2020;2(12):2899-2902.
-
Zhang QY, Tseng MH, Ding JJ, Huang JL. Case Report: Acute Renal Infarction in a Child with Coarctation of Aorta. Front Pediatr. 2021;9:707560.
-
Somasundaram NP, Ranathunga I, Ratnasamy V, et al. The Impact of SARS-CoV-2 Virus Infection on the Endocrine System. J Endocr Soc. 2020;4(8):bvaa082.



