Introduction. Congenital syphilis is a well-known infectious disease caused by the passing of Treponema pallidum from the infected mother to the fetus. In most cases, it leads to fetal death. Still, in the survivors, it can manifest clinically as early congenital syphilis in the first two years of life or late congenital syphilis afterward. Current epidemiological data suggest that the incidence is very low in developed countries due to screening. Case report. We report the case of a 2-month-old male infant who presented with a sepsis-like picture, generalized edema, and hepatosplenomegaly. He had elevated inflammatory markers (C-reactive protein and procalcitonin), acute kidney injury, and fulminant liver failure. The radiographic exam revealed periostitis of the long bones. The brain magnetic resonance imaging (MRI) revealed encephalitis, ventriculomegaly and cerebral atrophy, suggesting neurosyphilis. The diagnosis of congenital syphilis was confirmed by the positive Venereal Disease Research Laboratory (VDRL) test. We initiated the treatment with penicillin, then we associated ceftriaxone for neurological involvement. He also needed blood transfusions due to severe anemia and thrombocytopenia, diuretics, and hydrocortisone treatment. Conclusions. There are cases when screening methods are omitted, therefore congenital syphilis should always be considered in the differential diagnosis of sepsis in young infants.
Sifilisul congenital, o boală încă prezentă în era modernă: prezentare de caz şi analiza literaturii de specialitate
Early congenital syphilis, an old disease still occurring in the modern era: case report and literature review
First published: 16 martie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Pedi.61.1.2021.4724
Abstract
Rezumat
Introducere. Sifilisul congenital este o boală infectocontagioasă cauzată de pasajul spirochetei Treponema pallidum de la mama infectată la făt. În majoritatea cazurilor, conduce la moartea fătului, însă la supravieţuitori se manifestă clinic sub formă de sifilis congenital precoce în primii doi ani de viaţă sau sifilis congenital tardiv după vârsta respectivă. Datele epidemiologice recente sugerează o scădere marcantă a incidenţei bolii în ţările dezvoltate, ca rezultat al testelor de screening aplicate la nivel internaţional. Prezentare de caz. Prezentăm cazul unui sugar de sex masculin, în vârstă de 2 luni, cu un tablou clinic sugestiv pentru sepsis, edeme generalizate şi hepatosplenomegalie. Paraclinic, avea markerii inflamatori mult crescuţi (proteina C reactivă şi procalcitonina), injurie renală acută şi insuficienţă hepatică fulminantă. La examenul radiografic al membrelor s-a decelat periostită la nivelul oaselor lungi, iar imagistica prin rezonanţă magnetică cerebrală a evidenţiat modificări de encefalită, ventriculomegalie şi atrofie cerebrală, sugestive pentru neurosifilis. Diagnosticul a fost confirmat prin titrul Venereal Disease Research Laboratory (VDRL) pozitiv. Am iniţiat tratament antibiotic cu penicilină G şi am asociat ceftriaxonă, având în vedere afectarea neurologică. Pacientul a necesitat şi tratament suportiv, constând în transfuzii de masă eritrocitară şi trombocitară, diuretice şi hidrocortizon intravenos. Concluzii. Deşi screeningul pe parcursul sarcinii se aplică în majoritatea statelor dezvoltate, există cazuri în care este omis. Astfel, sifilisul congenital ar trebui să fie luat în considerare întotdeauna în diagnosticul diferenţial al sepsisului la sugarul mic.
Introduction
Congenital syphilis is currently considered a rare disease in Romania due to the screening campaign for pregnant women. According to the latest reports from 2018, in our country there were registered five cases with congenital syphilis in one year, the incidence being 0.03 out of 1000 live births(1). Congenital syphilis is caused by the in utero transmission of a spirochete, Treponema pallidum, from mother to fetus. It often leads to abortion, but it is a significant cause of morbidity in the remaining cases. Based on the onset age, congenital syphilis can take two forms: early congenital syphilis, presenting in the first two years of life, and late congenital syphilis, after 2 years old(2,3). The World Health Organization (WHO) strategies and recommendations for reducing mother-to-fetus transmission of sexually transmitted diseases have reduced the incidence of cases. Still, congenital syphilis remains a significant public health issue(4). In Romania, the screening is performed during the first trimester of pregnancy and repeated in the delivery room. It consists of nontreponemal tests – Venereal Disease Research Laboratory test (VDRL) or Rapid Plasma Reagin test (RPR)(2). However, there are situations in which the screening is omitted, leading to severe cases of infection with Treponema pallidum in neonates or infants.
Case presentation
We are reporting the case of a 2-month-old male infant who presented to the emergency room for fever, irritability, diarrhea and abdominal bloating. He was born at 37 weeks of gestation, by caesarean section for maternal indication (uterine scar). The pregnancy was normal and periodically monitored at the local hospital. There was no consanguinity of the parents, and the mother was without past medical history. At birth, his weight was 3100 g, his height was 50 cm, and the Apgar score was 10 points. He started breastfeeding immediately after birth and received immunization for hepatitis B virus and tuberculosis. At the age of 2 months, he presented fever and vomiting, for which he received symptomatic treatment at home. A few days later, he was admitted to our hospital with persistent fever, diarrhea, lethargy and dehydration signs. On examination, he weighed 4600 grams. He was irritable, with a tendency to opisthotonus posture and spasticity of the upper limbs. The temperature was normal. He was pale with cold extremities, congested pharyngeal mucosa, and nasal congestion with mucous discharge. The heart rate was 150 beats per minute, blood pressure was 91/50 mmHg, and the respiratory rate was 40 breaths per minute. The abdomen was very distended due to ascites, hepatomegaly (8 cm below the costal border), and splenomegaly. He had important edemas of the extremities and dactylitis of the upper limbs’ index and middle fingers (Figure 1).

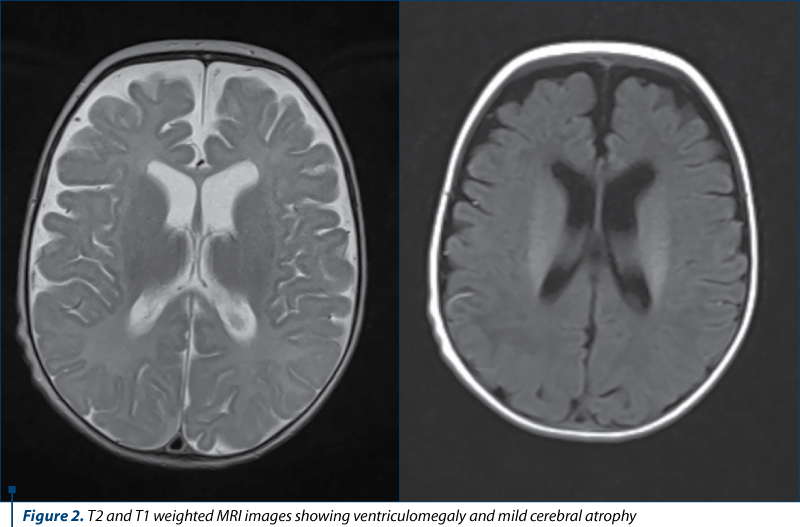
He was initially admitted to the intensive care unit. The laboratory results showed leukemoid reaction (leucocytes count 46,000/µL), anemia (hemoglobin 8.2 g/dL), thrombocytopenia (26,000/µL), severe hypoglycemia (8 mg/dL), and metabolic acidosis (pH: 6.99; pCO2: 34 mmHg; HCO3: 8.4 mEq/L; lactate >20 mmol/L). He had increased acute-phase reactants (C-reactive protein 25 mg/dL, procalcitonin 12 ng/mL), increased level of the liver enzymes (alanine transaminase 750 U/L, aspartate transaminase 2550 U/L), hypoalbuminemia, prolonged prothrombin time (39 seconds), and increased INR (2.44). He also had altered kidney function (creatinine 2.31 mg/dL and urea 94 mg/dL), severe hyponatremia (128 mEq/L) and hyperkalemia (6.5 mEq/L). Serologic tests for hepatitis viruses A, B, C, Epstein-Barr virus, cytomegalovirus, Toxoplasma gondi, herpes simplex virus 1 and 2, and human immunodeficiency virus were negative. He had a positive Rapid Plasma Reagin (RPR) test and a positive Venereal Disease Research Laboratory (VDRL) titer (6.23 RLU). The radiographic exam of the limbs revealed periostitis and osteochondritis of the femur and tibia and bone destruction regions on the tibial metaphysis. The cerebral magnetic resonance imaging (MRI) described ventriculomegaly, mild cerebral atrophy, and encephalitis lesions (Figure 2). The ophthalmologic exam was normal and the otolaryngologic examination revealed bilateral purulent rhinitis with bilateral otitis.
Based on the clinical presentation and the other investigations, the diagnosis was early congenital syphilis, acute liver failure (ALF), acute kidney injury, acute encephalitis, rhinitis, osteochondritis, anemia, thrombocytopenia, lactic acidosis, and severe hypoglycemia.
The patient received antibiotic treatment (penicillin G 150,000 U/kg/day given every 6 hours, ceftriaxone 100 mg/kg/day i.v.), hydrocortisone for the dactylitis, intravenous electrolytes, glucose, albumin infusion, and erythrocyte transfusion (due to severe anemia). As he presented significant peripheral edema, he received furosemide and spironolactone. After three weeks of treatment, the patient was recovered with no liver abnormality and the complete resolution of the inflammatory state. The periodic monthly follow-up showed normal physical development and normal laboratory parameters.
The follow-up neurological exam revealed only mild hypotonia.
Discussion
Congenital syphilis is a rare diagnosis nowadays in developed countries due to antenatal screening strategies. Unfortunately, it is still a public health burden, due to its incidence worldwide of 473 cases per 100,000 live births, being the second most common infectious cause of stillbirth(5). In Europe, the incidence of congenital syphilis is 1.1 cases per 100,000 live births(6). The burden of morbidity and mortality due to congenital syphilis is high. The latest reports described an annual rate of 143,000 early fetal deaths and stillbirths, 62,000 neonatal deaths, 44,000 low-birth-weight and preterm babies, and 102,000 infected infants(7). Syphilis can be transmitted from the mother to the fetus through the placenta in every infection stage. During the latent period, the disease’s transmission to the fetus can occur without knowing that the mother is sick(8). The infection can be transmitted less frequently during childbirth, from contact with contagious lesions(9).
The case we described was a severe form of early congenital syphilis, in which the screening tests omitted the mother’s infection. He developed almost all the complications that can occur in the early stages of congenital syphilis: fulminant liver failure, encephalitis, severe hypoglycemia, purulent rhinitis, osteochondritis, and periostitis of the tibia and femur.
Skeletal involvement is present in 70-80% of cases. The characteristic lesions consist of metaphyseal osteochondritis, destruction of the proximal tibial metaphyses, periostitis with periosteal new bone formation, and osteitis(10). As we observed in our case, periostitis and osteochondritis are usually symmetrical and involve the long bones’ shaft(11). The patient also presented the Wimberger sign, consisting of erosions of the tibial metaphysis(11). This type of bone manifestation is usually asymptomatic and revealed by the Rx. In other cases, it can lead to fractures and epiphyseal dislocations, causing severe pain and refusal to move the affected limb (“pseudoparalysis of Parrot”)(12,13). Our patient also had dactylitis of the index and the middle fingers that resolved without complications after a five-day course of hydrocortisone. Nevertheless, a careful evaluation is needed to detect any sign of paralysis and to apply specific rehabilitation measures.
He had marked leukocytosis, severe thrombocytopenia and anemia. As a consequence, he was lethargic and had impaired respiratory function, with tachypnea. The anemia was normochromic and normocytic, and responded well to the transfusion therapy. The thrombocytopenia resolved after the administration of platelet concentrates. The leukocytosis normalized after the antibiotics treatment. The Coombs-test negative anemia is a frequent encounter in the early phase of the disease. An extensive review of congenital syphilis demonstrated that almost 90% of affected infants were anemic(14,15). The pathogenesis is heterogenic and not fully understood, but some causes, like hypersplenism, impaired hematopoiesis by bone marrow changes, and nutritional deficiency, have been implicated(15). White blood cells (WBC) changes range from leukocytosis to leukopenia.
In some cases, as in our patient, the leukocyte number is so high that it can mimic malignant disease(14). Thrombocytopenia is present in one-third of the affected patients(16). Despite the low platelet count, our patient did not have clinical manifestations such as petechiae and bleeding. He tolerated transfusion therapy very well, with an excellent clinical course.
The liver involvement was severe, with marked hepatomegaly, fulminant hepatitis, acute liver failure with hypoalbuminemia, ascites, and peripheric edema. Given that it can be associated with very severe hypoglycemia, we must suspect a metabolic disorder that can be excluded after the negative screening tests for metabolic diseases. The most common metabolic disorders presenting in this age group are tyrosinemia and galactosemia. Other causes of acute liver failure in the neonatal period are perinatal infections with herpes viruses, cytomegalovirus, and parvovirus. Herpes simplex virus is the most common and carries a high mortality. Some severe hematological diseases, like hemophagocytic lymphohistiocytosis and congenital leukemia, can present in the neonatal period with pancytopenia, hepatosplenomegaly and acute liver failure(17). Hepatomegaly is a characteristic feature of congenital syphilis and can be detected in antenatal ultrasound examinations of the affected mothers(18). Hepatomegaly is probably due to acute syphilitic hepatitis or to increased extramedullary hematopoiesis due to heart failure and anemia(19). Liver involvement usually slowly resolves, as it did in our patient, or can worsen transiently after the penicillin treatment(9).
Acute encephalitis was another complication in our case, representing one of the two forms of neurosyphilis. Neurosyphilis usually manifests in the first months of life with the common signs of acute bacterial meningitis or encephalitis, or later as chronic meningovascular neurosyphilis with progressive hydrocephalus and developmental regression(9). In our case, we started early the treatment with penicillin and ceftriaxone, with an excellent evolution. An extremely rigorous follow-up is still necessary. Usually, there are no specific lesions for neurosyphilis, but in many cases, as in our patient, ventriculomegaly, inflammatory infiltrates and ischemic-hemorrhagic lesions can be found.
Less common manifestations of early congenital syphilis, not present in our case, include pneumonitis, nephrotic syndrome, myocarditis, and fibrosis of the gastrointestinal tract(12). Syphilitic pneumonitis is a severe complication that can lead to respiratory failure. In a study conducted by Pieper et al., the most common radiological picture of syphilitic pneumonitis consisted of coarse nodular pattern in addition to band-like opacities radiating from the hilar regions(20). Renal involvement is not frequent and can vary from simple albuminuria to nephrotic syndrome. It can result from the spirochete’s direct invasion of the kidney or secondary to a hypersensitivity reaction(21). Myocarditis is a rare finding, manifesting as gummatous myocarditis in tertiary syphilis(22). Intrauterine invasion of the gastrointestinal tract by the spirochetes leads to chronic inflammation, which can result in fibrosis. Although rare, this manifestation is significant during childhood due to the chronic malabsorption and failure to thrive(23).
In late congenital syphilis, symptoms often begin after 2 years of age or even later. They include pseudoparalysis of Parrot, neurodevelopmental delay, interstitial keratitis, sensorineural deafness, and Hutchinson’s teeth. The last three signs are also known as “the Hutchinson triad”(12,24-26). This form is characterized by the scars and sequelae of the early infection. The prolonged periostitis results are frontal bossing, saber shins (anterior bowing of the tibia), and scaphoid scapula. The destruction of the nasal cartilage leads to “saddle nose deformity”. Dental anomalies can also be found, with notched and widely spaced central incisors, called the Hutchinson’s teeth. Other sequelae include sensorineural deafness caused by the osteochondritis of the otic capsule, ocular involvement with uveitis and interstitial keratitis, and other neurological abnormalities as manifestations of neurosyphilis(9,12).
Early serological diagnosis in congenital syphilis is essential, leading to a significant decrease in severe cases. We should correlate the maternal serological data with the infant’s symptoms and laboratory results for a better accuracy. According to the Center for Disease Prevention and Control (CDC), any newborn from a seropositive mother, regardless of the presence of symptoms, should be tested with a non-treponemal test(25). The most frequently used are the non-treponemal antibodies, VDRL, and RPR tests, and the infant’s titer must be at least four-fold higher than the mother’s for the diagnosis of congenital syphilis(27). In our case, we performed the RPR and VDRL titer. These, correlated with clinical symptoms, were the basis for the diagnosis of congenital syphilis. Other specific tests are the darkfield microscopy study and the direct T. pallidum haemagglutination assay (TPHA), the T. Pallidum particle agglutination assay (TPPA), and the fluorescent Treponema antibody absorption assay (FTA-ABS). Still, they demonstrate IgA, IgM, and IgG antibodies without distinguishing them, so they cannot differentiate the transplacental passage of the antibodies of actual infection(27).
Penicillin has remained the most recommended and the most effective treatment for the Treponema pallidum infection. It is also the only antimicrobial drug recommended for congenital syphilis, neurosyphilis and syphilis in pregnancy(9). For the pediatric patients, the regimen consists of aqueous benzathine penicillin G, 50,000 U/kg/dose i.v., given every 12 hours in the first seven days of life and every 8 hours after that, for ten days, or procaine penicillin G, 50,000 U/kg/dose i.m., once daily, for ten days(26). Our patient received a 14-day course of penicillin associated with ceftriaxone due to severe sepsis and neurological involvement. On the first day after the penicillin treatment initiation, a small percentage of patients can develop an acute complication named the Jarisch-Herxheimer reaction; the rapid destruction of the Treponemas causes fever, tachypnea, hypotension and can lead to cardiovascular collapse(12). Our patient responded very well to the treatment, without any complications. European guidelines recommend that infants born to syphilitic mothers who completed the treatment before giving birth should also receive benzathine penicillin G, 50,000 units/kg i.m., in a single dose(28).
For patients who received adequate treatment in the first two months of life, the prognosis is excellent, but there is insufficient data for the long-term evolution of these cases. We administered an appropriate antimicrobial regimen early, therefore we expect a good prognosis, without any severe consequences. There are possible complications and sequelae described, the late congenital syphilis manifestations, with sensorineural deafness, being the most common(29). Rigorous follow-up appointments conducted by a multidisciplinary team, including a pediatric neurologist and otolaryngologist, will be able to detect any hearing impairment, so that appropriate measures can be taken at the right moment.
WHO recommends that all pregnant women perform Treponema infection screening by the end of the first trimester. Those patients with a positive diagnosis should receive treatment with an adequate penicillin regimen(7). Romania is following international trends, screening evaluation in the first trimester, and frequent serological follow-ups for the treated positive cases or for high-risk patients(30).
Conclusions
We aimed to raise awareness about the possibility of congenital syphilis in every newborn or infant presenting with sepsis without an apparent cause. With all efforts to reduce the incidence of syphilis, it is still a reality in our times. Adequate pregnancy screening and perinatal care must identify the congenital syphilis cases before they become symptomatic or during the early stage, when the treatment can start before the infection’s systemic damage. In some cases, that “escape” the screening tests, the physician should be alert to the possibility and perform at least a non-treponemal test on the suspected patients. Given that the treatment with penicillin is highly effective when administered in the early phase, the long-term sequelae can be avoided or diminished, giving these patients a better prognosis regarding future morbidity and social involvement.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Centrul Naţional de Supraveghere şi Control al Bolilor Transmisibile. Analiza evoluţiei bolilor transmisibile aflate în supraveghere. Raport pentru anul 2018 [Internet]. Bucureşti: CNSCBT; 2019 [updated 2019 Dec 04; cited 2020 Dec 10]. Available at: https://www.cnscbt.ro/index.php/rapoarte-anuale/1302-analiza-bolilor-transmisibile-aflate-in-supraveghere-raport-pentru-anul-2018/file
- European Centre for Disease Prevention and Control. Antenatal screening for HIV, hepatitis B, syphilis and rubella susceptibility in the EU/EEA [Internet]. Stockholm: ECDC; 2016 [updated 2016 Mar; cited 2020 Dec]. Available at: https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/antenatal-screening-HIV-hepatitis-B-syphilis-rubella-EU.pdf
- American Academy of Pediatrics. Syphilis. In: Kimberlin DW, Brady MT, Jackson MA, et al. eds. Red Book, 30th Edition (2015): 2015 report of the Committee on Infectious Diseases, 30th Edition. 2015: 755–68. Available at: https://ebooks.aappublications.org/content/red-book-30th-edition-2015.tab-info (accessed 2020 Dec).
- World Health Organisation. Global Health Sector Strategy on Sexually Transmitted Infections 2016-2021 [Internet]. Geneva (Switzerland): WHO; 2016 [updated 2016 Jul; cited 2020 Dec]. Available at: https://apps.who.int/iris/bitstream/handle/10665/246296/WHO-RHR-16.09-eng.pdf;jsessionid=1FCABB702F5275646390C24B06E831BC?sequence=1
- Korenromp EL, Rowley J, Alonso M, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes – Estimates for 2016 and progress since 2012. PLoS ONE. 2019;14(2):e0211720.
- European Centre for Disease Prevention and Control. Syphilis and congenital syphilis in Europe – A review of epidemiological trends (2007-2018) and options for response [Internet]. Stockholm: ECDC; 2019 [updated 2019 Jul 19; cited 2020 Dec 10]. Available at: https://www.ecdc.europa.eu/sites/default/files/documents/syphilis-and-congenital-syphilis-in-Europe.pdf
- World Health Organisation. WHO guide on syphilis screening and treatment for pregnant women [Internet]. Geneva: WHO; 2017 [updated 2017; cited 2020 Dec]. Available at: https://apps.who.int/iris/bitstream/handle/10665/259003/9789241550093-eng.pdf?sequence=1
- Milanez H. Syphilis in Pregnancy and Congenital Syphilis: Why Can We not yet Face this Problem? Rev Bras Ginecol Obstet. 2016;38(9):425-427.
- Woods CR. Syphilis in Children: Congenital and Acquired. Semin Pediatr Infect Dis. 2005;16:245-57.
- Arnold SR, Ford-Jones EL. Congenital syphilis: A guide to diagnosis and management. Paediatr Child Health. 2000;5(8):463-69.
- Toohey JS. Skeletal Presentation of Congenital Syphilis: Case Report and Review of the Literature. Journal of Pediatric Orthopedics. 1985;5:104-106.
- Cooper JM, Sanchez PJ. Congenital syphilis. Seminars in Perinatology. 2018;42:176-84.
- Armangil D, Canpolat FE, Ygit S, et al. Early congenital syphilis with isolated bone involvement: a case report. Turk J Pediatr. 2009;51(2):169-71.
- Al-Faris L, Al-Humood S. Congenital syphilis mimicking haematological or oncological disorders. Paediatrics and International Child Health. 2012;32(2):111-115.
- Sartain P. The anemia of congenital syphilis. South Med J. 1965;58:27-31.
- Freiman I, Super M. Thrombocytopenia and congenital syphilis in South African Bantu infants. Arch Dis Child. 1966;41:87-90.
- Dhawan A, Mieli-Vergani G. Acute liver failure in neonates. Early Human Development. 2005;81:1005-1010.
- Hollier LM, Harstad TW, Sanchez PJ, et al. Fetal syphilis: clinical and laboratory characteristics. Obstet Gynaecol. 2001;97:947-53.
- Hira SK, Bhat GJ, Patel JB, et al. Early congenital syphilis: clinico-radiologic features in 202 patients. Sex Transm Dis. 1985;12(4):177-83.
- Pieper CH, Gelderen WF, Smith J, et al. Chest radiographs of neonates with respiratory failure caused by congenital syphilis. Pediatr Radiol. 1995;25(3):198-200.
- Kim YH, Song JH, Kim CJ, et al. Congenital Syphilis Presenting with Only Nephrotic Syndrome: Reemergence of a Forgotten Disease. J Korean Med Sci. 2017;32:1374-1376.
- Pandey S. Nonviral myocarditis [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 (updated: 2020 Jun 03; cited: 2021 Jan 21). Available at: https://www.statpearls.com/ArticleLibrary/viewarticle/25469
- Celik M, Bulbul A, Uslu S. Congenital Syphilis Presenting with Prenatal Bowel Hyperechogenity and Necrotizing. Sisli Etfal Hastan Tip Bul. 2020;54(1):113-116.
- Galvis AE, Arrieta A. Congenital Syphilis: A U.S. Perspective. Children. 2020;7(11):203.
- Frieden TR, Jaffe HW, Cono J, et al. Congenital Syphilis – 2015 STD Treatment Guidelines. MMWR Recomm Rep. 2015;64(3):34-49.
- Heston S, Arnold S. Syphilis in Children. Infect Dis Clin N Am. 2018;32:129-44.
- Herremans T, Kortbeek L, Nortemans DW. A review of diagnostic tests for congenital syphilis in newborns. Eur J Clin Microbiol Infect Dis. 2010;29:495-501.
- Janier M, Hegyi V, Dupin N, et al. 2014 European guideline on the management of syphilis. JEADV. 2014;28:1581-1593.
- Arnold SR, Ford-Jones EL. Congenital syphilis: A guide to diagnosis and management. Paediatr Child Health. 2000;5(8):463-69.
- Ionescu D, Ionescu G, Bancescu A. Sifilisul congenital – ghid de management [Internet]. Bucuresti: INCDMI “Cantacuzino”; Available at: http://www.dspcluj.ro/HTML/anunturi/ITS/Ghid_Sifilis_Cong_.pdf [Accessed 2020 Dec].