The distribution by macroregions of human resources and of the institutional treatment capacities for psychiatric disorders is uneven, which led to a very low supply of support services for psychiatric pathology during the study period. The distribution of human resource of psychiatrists in Romania is 11.88/100,000 inhabitants, far behind most European countries. Moreover, in some Romanian macroregions (2 and 4), the number of psychiatrists per 100,000 inhabitants is below the national average. A situation below the average level of distribution of human resources and hospital beds was found in Macroregion 2 and Macroregion 3. The hospitalization indicators were influenced by the conditions imposed by the state of emergency, respectively by the state of alert induced by evolution of the COVID-19 pandemic, throughout the year 2020. Thus, the most obvious changes of the diagnostic related groups (DRG) indicators in 2020 versus 2019 were: the decrease in the number of patients with affective disorders hospitalized in public hospitals; the increase in the duration of hospitalization of patients, as a proof of the severity of hospitalized cases. By the regulations of the Government Ordinance no. 252/20.03.2020, regarding the telemedicine consultations and, implicitly, the telepsychiatric ones, the discrepancy between the increased demand for psychiatric assistance and the much-diminished offer for access to hospitalizations or consultations in Romania was reduced.
Adresabilitatea către serviciile spitaliceşti de psihiatrie în timpul pandemiei de COVID-19 din România
Inpatient psychiatric services use during the COVID-19 pandemic in Romania
First published: 16 aprilie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.64.1.2021.4774
Abstract
Rezumat
Distribuţia în cele patru macroregiuni ale României a resurselor umane şi a capacităţilor instituţionale de internare pentru tratamentul tulburărilor psihiatrice este inegală. Distribuţia resursei umane de psihiatri din România este de 11,88/100000 de locuitori, mult în urma majorităţii ţărilor europene. Mai mult, în unele macroregiuni din România (2 şi 4), numărul psihiatrilor la 100000 de locuitori se situează sub media pe ţară. Această situaţie este şi mai evidentă în Macroregiunea 2 şi Macroregiunea 3, unde se găseşte cel mai scăzut număr mediu de resurse umane şi de paturi de spital la 100000 de locuitori. Indicatorii de spitalizare pe parcursul anului 2020 au fost influenţaţi de condiţiile impuse de starea de urgenţă, urmată de cea de alertă, şi de gradul de evoluţie a pandemiei de COVID-19. Astfel, cele mai evidente schimbări a indicatorilor DRG de spitalizare în 2020 în comparaţie cu cei din 2019 au fost reprezentate de: scăderea numărului de pacienţi cu tulburări afective internaţi în spitalele publice; creşterea duratei de spitalizare a pacienţilor, ca dovadă a severităţii cazurilor internate. Prin reglementările aduse de OUG 252/20.03.2020, în privinţa consultaţiilor de telemedicină, inclusiv de telepsihiatrie, discrepanţele dintre cererea crescută de asistenţă psihiatrică şi oferta mult dimininuată de acces la îngrijirile spitaliceşti şi/sau la consultaţiile în ambulatoriu s-au redus.
It is well known that epidemics can be the basis for new psychiatric pathologies or relapses in patients with an already established psychiatric diagnosis(1).
Thus, during and also after the pandemic, the mental health needs are increasing, which can overload the available resources, the most problematic being the areas where access is limited due to poor medical infrastructure or insufficient specialized medical staff.
Since the beginning of March 2020 (11.03.2020, the date of declaration of COVID-19 as a pandemic, including in the EU and, implicitly, in Romania), there has been an increase in request for medical care from patients in hospital outpatient clinics and emergency receptions. This change corresponded with an increase in presentations related to depressive symptoms.
The declaration of the state of emergency by Decree of the President of Romania no. 195 of March 16, 2020, regarding the establishment of the state of emergency on the Romanian territory(2), opened the possibility of issuing military ordinances. Thus, the Military Ordinance no. 2 of 21.03.2020 provided for the restriction of the movement of persons between 10 p.m. and 6 a.m.
On 23.03.2020, by Order no. 74527 of the Department for Emergency Situations, the Romanian state decided that the activity in the hospital outpatient services be suspended for all consultations and treatments that can be rescheduled. Due to the large number of patients requesting outpatient medical services, consultations in the hospital emergency room had to supplement this type of consultation. Thus, a larger number of patients presented to the emergency rooms which did not require emergency psychiatric care.
At the express request of some professional medical organizations, including that of psychiatrists, represented by the Romanian Association of Psychiatry and Psychotherapy, the Government responded promptly by issuing the Government Ordinance no. 252/30.03.2020, which decided to allow telemedicine consultations (implicitly those of telepsychiatry) in the outpatient network(3).
The Order of the Minister of Health no. 555, in force since 7.04 2020, on the approval of the plan of measures for the preparation of hospitals in the context of the COVID-19 epidemic, of the list of hospitals providing healthcare to patients tested positive for SARS-CoV-2 in phase I and in phase II and the list of support hospitals for patients tested positive or suspected with SARS-CoV-2 infection, imposed the epidemiological triage at hospitalization or consultation at the level of the emergency unit (or emergency room) of each hospital, regardless of specialty(4).
Until Government Ordinance no. 252/30.03.2020, for people returning to the country, the only possibility to care for a psychiatric condition was to call for consultations in the private system or to the emergency room of psychiatric hospitals. In these circumstances, the problem of access to mental healthcare has become acute, which in our country is still limited by some barriers (structural or attitudinal), such as:
-
unequal distribution of hospital beds in different geographical areas;
-
long distances from the hospital or the outpatient clinic;
-
unequal distribution of human resources for the care of mental disorders throughout the country;
-
deficient information regarding the availability of psychiatric outpatient clinics;
-
difficulties in scheduling consultations;
-
problems with the operating hours of outpatient clinics (especially for those over 65 years of age);
-
attitudinal barriers (stigma, opposition to psychiatric consultation, poor relationship with medical staff etc.).
Research methodology
Research typology
This study is retrospective, observational and descriptive.
Study population
The sufficient number of specialists is an important criterion for assessing the degree of access of the population to care for mental disorders. In this regard, the delimitations on the EU territory of the geographical and socioeconomic regions, called macroregions (MR), are helpful. Thus, in Romania there are described geographically four macroregions: Macroregion 1 (MR 1 – 4.879 million inhabitants), Macroregion 2 (MR 2 – 5.620 million inhabitants), Macroregion 3 (MR 3 – 5.256 million inhabitants) and Macroregion 4 (MR 4 – 3.720 million inhabitants), according to the Romanian National Institute of Statistics (NIS)(5). The most relevant socioeconomic indicators are GDP/capita and unemployment rate (Table 1).
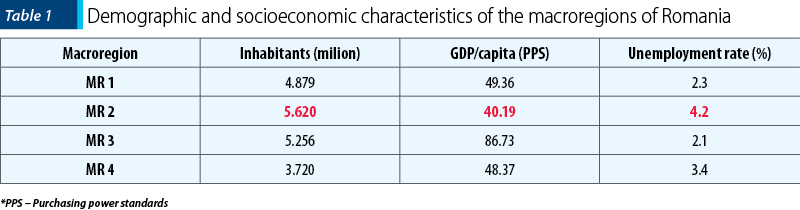
The highest number of inhabitants was found in MR 2 (5.620 million inhabitants). Unfortunately, the same MR 2 is the macroregion with the lowest socioeconomic profile.

Sources of information
Four categories of unclassified national and international sources of public data were used:
a. Demographic data.
b. Epidemiological information on the evolution of the COVID-19 pandemic in Romania.
c. Information about the beds in the public psychiatric care institutions.
d. Information about the human resource, represented by the specialized doctors of adult psychiatry and child psychiatry (the other staff working in the assistance institutions for people with mental issues was not taken into account, due to the lack of official data for this sector).
Demographic data were taken from two sources:
-
National Institute of Statistics, for the total population of Romania and the population of the counties(5);
-
for the geographical delimitation of the four territorial units – macroregions (MR) of Romania located in the EC nomenclature, we used the data published in EUROSTAT(6)
For the information about the evolution of the COVID-19 pandemic in Romania, we used the data published daily by the National Institute of Public Health (NIPH)(7).
The absolute number of beds in psychiatric institutions in the public system (acute psychiatry, chronic psychiatry, child psychiatry, drug addiction departments) in each county was provided by the National Center for Mental Health and Anti-Drug Control (NCMHA)(8).
The human resource available for providing psychiatric treatment, represented by the number of psychiatrists in public hospitals, doctors in specialized clinics (public and private), was taken from the National Health Insurance House (NHIH) and NCMHA(8).
Statistical analysis
The statistical calculations were performed using Microsoft Office Excel, version 2019.
Thus, we calculated the distribution of the population by macroregions, the epidemiological indicators of COVID-19 infection per 100,000 inhabitants, the number of doctors working in hospitals and those working in outpatient clinics, in both situations the reporting being done per 100,000 inhabitants, and the number of beds in psychiatric institutions, both public and private, reported per 100,000 inhabitants.
The average of the hospitalization indicators was calculated according to the quarters (Q). These indicators include: the number of hospitalizations, the average duration of hospitalization, and the total number of days of hospitalization associated with the major diagnostic group.
Results
A. Distribution by macroregions of psychiatrists in Romania
The coverage of mental healthcare services, represented by the mean number of psychiatrists working in hospitals and outpatient clinics, is 11.88 per 100,000 inhabitants (EUROSTAT, 2018). This number is larger than 10 years ago, which was of 10 psychiatrists per 100,000 inhabitants.
But this number is different in the four macroregions of Romania. The number of psychiatrists in each macroregion and their distribution per 100,000 inhabitants in 2018 are presented in Table 2 and Figure 2.
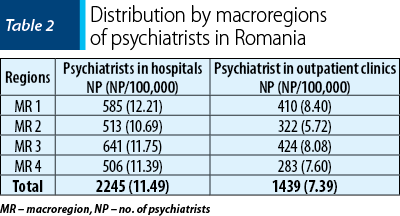
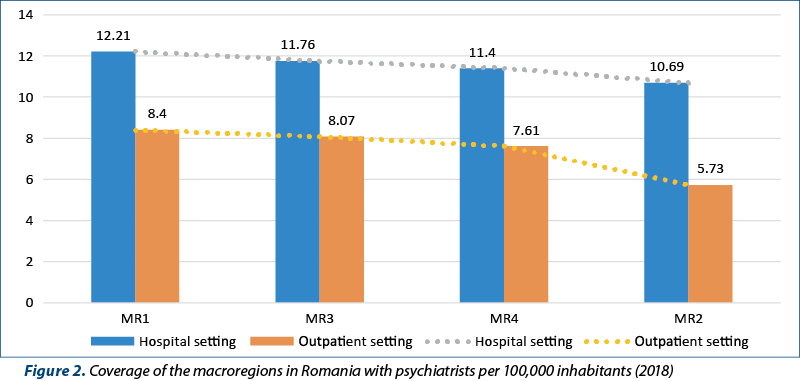
We found that in MR 1, an optimal number of psychiatrists is ensured, both in the hospital services and in the coverage with norms of the NHIH affiliated outpatient clinics. On the other hand, there is a shortage of human resources for psychiatric care (hospital/outpatient) in MR 2.
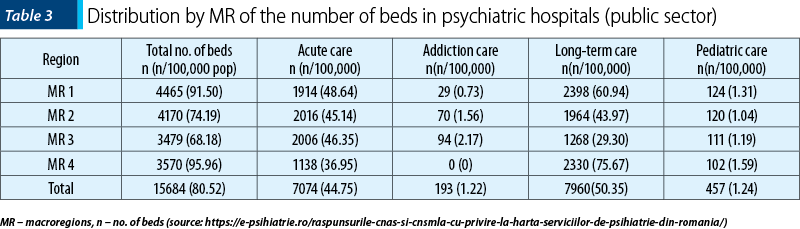
B. Distribution by macroregions of the number of psychiatric beds in the public system, by categories of care
The number of beds in the acute wards is almost equal in MR 2 (2016) and MR 3 (2006), but with a significant decrease in MR 4 (1138). On the other hand, MR 4 has the highest number of beds in the long-term wards (2330), while MR 3 (1268) has the fewest in this category. A disadvantageous situation is the insufficient number of beds for the treatment of addiction pathology, with a total number in the whole country of only 193 beds. Also, the beds for child psychiatry are poorly represented in the country (457) – Table 3(8).
C. Psychiatric care during the restrictions imposed by the emergency/alert state declared due to the COVID-19 pandemic (2020)
The impact of the pandemic on psychiatric care in Romania can be assessed by the dynamics of hospitalization indicators of one of the most common mental disorders of modern times, namely major affective disorder.
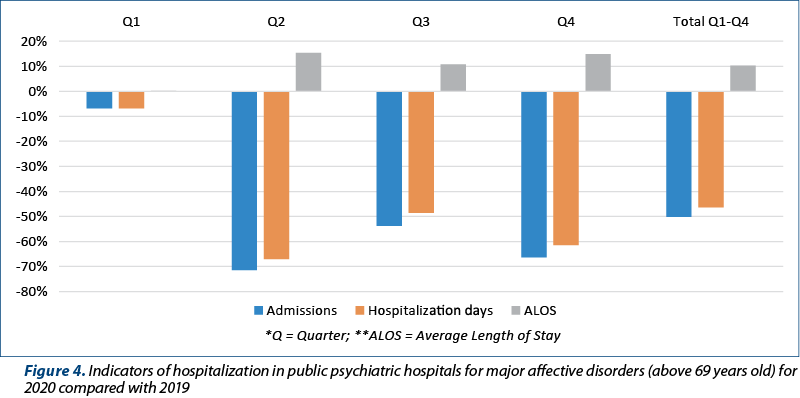
In this respect, the year 2020 was taken into account, during which it was possible to notice a change in all hospitalization indicators, regarding the hospitalizations in public psychiatric hospitals compared to the same data from 2019 (Figure 3 and Figure 4). The indicators taken into account were: number of hospitalizations, average length of hospitalization, total number of hospitalization days. The hospitalization indicators for affective disorders in public hospitals (2020 versus 2019) were calculated by age groups: patients under 70 years old, respectively patients over 69 years old.
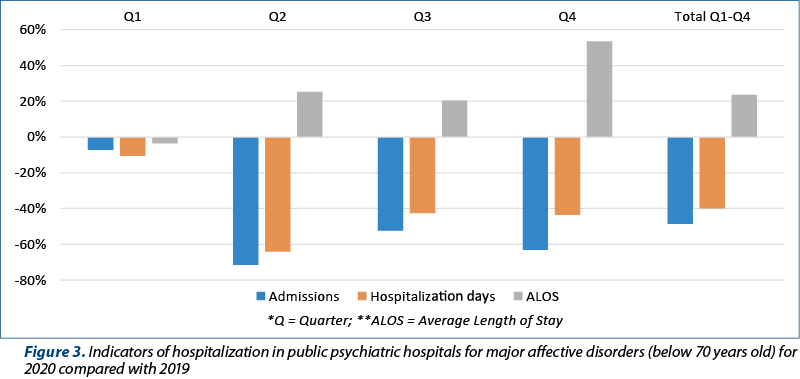
In the age group below 70 years old, there was a drastic decrease in the number of hospitalizations and in the total number of hospitalization days, but the average duration of hospitalizations increased, especially in Q4 (by 50%).
In the age group above 69 years old, an even more drastic decrease was observed in the number of hospitalizations (more than 70%), followed closely by the decrease in the number of days of hospitalization. The length of hospitalization increased on average by 15% throughout 2020.
Discussion
The distribution by macroregions of human resources and institutional treatment capacities for psychiatric disorders is uneven, both in terms of human resources (psychiatrists for adults and children) and in terms of the logistical resource of coverage with psychiatric beds, differentiated in hospitals on different categories of pathology (acute or chronic psychiatric disorders, addictions) or age (child psychiatry, psychogeriatrics).
A. The distribution by macroregions of psychiatrists in Romania shows that MR 1 is the one that offers the best coverage in terms of psychiatrists, both in hospitals (12.21 psychiatrists per 100,000 inhabitants) and outpatient clinics (8.4 psychiatrists per 100,000 inhabitants), followed by MR 2 (12.21 psychiatrists in hospitals per 100,000 inhabitants and 8.07 psychiatrists in outpatient clinics) and MR 4 (11.40 psychiatrists in hospitals per 100,000 inhabitants and 7.61 in outpatient facilities). Macroregion 2 is the one that offers the lowest coverage of psychiatrists both in hospitals (10.69 psychiatrists per 100,000 inhabitants) and in outpatient clinics (5.73 psychiatrists per 100,000 inhabitants). We also refer to the precarious economic conditions of the Macroregion 2.
However, the number of psychiatrists in Romania (11.88/100,000 inhabitants) compared to countries such as Switzerland (53.1/100,000), Germany (27.75/100,000), The Netherlands (24.15/100,000) or Greece (25.79/100,000), is much lower.
B. The distribution of the number of beds within psychiatric institutions varies in the macroregions of Romania, MR 4 having the highest number of beds per 100,000 inhabitants (95.96/100,000 inhabitants), followed by MR 1 (91.5 beds per 100,000 inhabitants) and MR 2 (74.19/100,000 inhabitants). MR 3 has the lowest total number of beds (68.18/100,000 inhabitants). We could not correlate this low number of beds in MR 3 with the economic conditions of Macroregion 3. Probably, most psychiatric institutes are concentrated in the capital of Romania and the neighboring county (Ilfov).
The same ranking is maintained in terms of the total number of psychiatric beds in chronic wards per 100,000 inhabitants. It should be noted, however, that there are very large inequalities between the number of beds per 100,000 inhabitants between MR 4 (75.6/100,000 inhabitants) and MR 1 (60.94/100.000 inhabitants), on the one hand, and MR 2 (43.97/100,000 inhabitants) and MR 3 (29.3/100.000 inhabitants), on the other hand.
MR 1 has the highest total number of psychiatric beds in acute wards, 48.64/100,000 inhabitants, followed by MR 3 (46.35/100,000 inhabitants), MR 2 (45.14/100,000 inhabitants) and MR 4 (36.95/100,000 inhabitants).
All macroregions have an almost similar number of total child psychiatry beds per 100,000 inhabitants.
Regarding the total number of beds in addiction wards per 100,000 inhabitants, in MR 4 there are none and in the other macroregions the number is very small (MR 1: 0.73/100,000 inhabitants; MR 2: 1.56/100,000 inhabitants; MR 3: 2.17/100.000 inhabitants).
Regarding the ratio between the number of psychiatric beds per 100,000 inhabitants in acute wards and that of beds in chronic wards, it can be noticed that in MR 4 the ratio of the number of beds in chronic wards is more than twice as high as in that of the beds in the acute wards, while in MR 3 the number of beds in the acute wards (46.35/100,000 inhabitants) is much higher than that of the beds in the chronic wards (29.3/100,000 inhabitants).
C. Hospitalization indicators regarding affective major disorders highlighted the impact of the pandemic on the psychiatric care in Romania.
This impact was evaluated in the present study only on a very common psychiatric pathology, namely major affective disorders.
We notice that, if at the beginning of 2020, when the COVID-19 pandemic had just started in Romania, the indicators did not change significantly compared to the same period (Quarter 1) of 2019, in the next three quarters the DRG indicators changed drastically. The measure of the transformation of some psychiatric hospitals in Romania into COVID-19 support hospitals was reflected in a differentiation regarding two DRG indicators, compared to 2019: the number of hospitalized patients, and the number of hospitalization days. The largest differences for the population below 70 years old were found in Quarter 2 and Quarter 4, coinciding with the first and second waves of the COVID-19 pandemic, respectively.
For the population above 69 years old, there were accentuated the differences of the hospitalization indicators, especially regarding the number of hospitalizations, with decreases between 50% and 70%, starting with Quarter 2.
The Average Length of Stay (ALOS) also increased during Q2-Q4, especially regarding the patients admitted to chronic wards.
Study limits
Since we used demographic data (total and regional number of the Romanian population) and data regarding staff resources (from hospitals, outpatient clinics, mental health centers) in the statistics for 2018, there may be some differences from the statistical data for 2020. Unfortunately, these data have not been communicated so far, both in national and international statistics.
Conclusions
The distribution by macroregions of human resources and institutional treatment capacities for psychiatric disorders is uneven, which led to a very low supply of support services for psychiatric pathology during the study period.
The human resource of psychiatrists in Romania is 11.88/100,000, far behind most European countries. Moreover, in some macroregions (MR 2 and MR 4), the number of psychiatrists at 100,000 inhabitants is below the national average.
A situation below the average level of distribution of human resources and hospital beds was found in MR 2 and MR 3.
The hospitalization indicators were influenced by the conditions induced by the state of emergency, respectively by the alert state imposed by the evolution of the COVID-19 pandemic, throughout the year 2020. Thus, the most obvious changes of the diagnostic related groups (DRG) indicators in 2020 versus 2019 were:
-
the decrease in the number of patients with affective disorders hospitalized in public hospitals;
-
the increase in the duration of hospitalization of patients, as a proof of the severity of hospitalized cases.
This change in DRG indicators in 2020 can be also explained by the reduced possibility of the population in areas with low socioeconomic indicators, for using private services. The Government Ordinance no. 252/20.03.2020 regulated the telemedicine consultations – and, implicitly, the telepsychiatric ones –, and the discrepancy between the increased demand for psychiatric assistance and the much-diminished offer for access to hospitalizations or consultations in Romania was reduced.
Bibliografie
- Tucci V, Moukaddam N, Meadows J, Shah S, Galwankar SC, Kapur GB. The forgotten plague: psychiatric manifestations of Ebola, Zika, and emerging infectious diseases. J Glob Infect Dis. 2017;9:151–6.
- http://legislatie.just.ro/Public/DetaliiDocumentAfis/223831
- http://www.cnas.ro/national-page/hg-nr-252.html
- http://www.cnas.ro/cjastm/media/postFiles/Ordin%20555_2020.pdf
- http://statistici.insse.ro:8077/tempo-online/
- https://ec.europa.eu/eurostat/web/regions-and-cities/overview
- https://www.cnscbt.ro/index.php/analiza-cazuri-confirmate-covid19/1539- analiza-cazuri-confirmate-261-pana-la-18-03-2020/file
- https://e-psihiatrie.ro/raspunsurile-cnas-si-cnsmla-cu-privire-la-harta-serviciilor-de-psihiatrie-din-romania/
Articole din ediţiile anterioare
Accesul populaţiei din România la îngrijiri de sănătate mintală în timpul pandemiei de COVID-19
Contextul nou apărut atât în România, cât şi pe plan mondial – pandemia de COVID-19 – a pus la încercare sistemul medical la nivelul tuturor ţărilo...
Este secolul 21 pregătit pentru o schimbare în practica psihiatriei? Locul telepsihiatriei în cadrul telemedicinei europene şi globale
Telemedicina are multe definiții, dar aceasta înseamnă, în principal, „medicină la distanţă“. De fapt, constă în furnizarea de servicii de asistenț...
Comportamentul suicidar în perioada prepandemică şi intrapandemică în România (I)
Pandemia este deopotrivă o problematică acută de sănătate publică la nivel mondial, din punctul de vedere al patologiei infecţioase, dar şi al impa...