Aspecte ale episoadelor depresive şi impactul depresiei la vârstnici
Aspects of depressive episodes and the impact of depression in the elderly
Abstract
Depression syndrome in older people can manifest by sadness, considered more common in older adults, withdrawal, apathy and lack of vigor. Depressive disorders are debilitating health problems, being the leading cause of disability worldwide. Women are more likely to have symptoms of depression than men, and less than half of people with depression reported contacting a doctor or healthcare professional. We present a review about the main causes and symptoms of depression in older people. The elderly are usually neglected and have more difficult medical consultations, especially when they lose their autonomy. Depression in older people remains a significant social problem regarding its diagnosis and treatment.Keywords
depressionolder adultsmoodsadnessRezumat
Sindromul depresiv la vârstnici se poate manifesta prin tristeţe, considerată mai frecventă la adulţii în vârstă, sevraj, apatie şi lipsă de vigoare. Tulburările depresive sunt probleme de sănătate debilitante, reprezentând principala cauză a dizabilităţii la nivel mondial. Femeile au mai multe şanse de a avea simptome de depresie decât bărbaţii şi mai puţin de jumătate dintre persoanele cu depresie au raportat că au contactat un medic sau un profesionist din domeniul sănătăţii. Prezentăm un review despre principalele cauze şi simptome ale depresiei la vârstnici. Bătrânii sunt de obicei neglijaţi şi au consultaţii medicale mai dificile, în special atunci când îşi pierd autonomia. Depresia la vârstnici rămâne o problemă socială semnificativă în privinţa diagnosticului şi a tratamentului.Cuvinte Cheie
depresievârstnicistare de spirittristeţeIntroduction
Depression is a mood disorder that affects how a person feels, thinks or behaves, impairing the social or occupational functioning(1). Depressive disorders are debilitating health problems which are the leading cause of disability worldwide(2). These disorders are characterized by loss of interest in activities, weight changes, and sleep disorders, fatigue, feelings of guilt and worthlessness. Depression can lead to deficiencies in functioning socially, decreasing significantly the quality of life and increasing the risk of comorbidities. It is one of the most common chronic diseases in the general population(3).
Between 2005 and 2006, the National Health and Nutrition Survey (NHANES) reported that more than 5% of the people in the United States of America suffered from depression.
These rates varies according to age, gender, race/ethnicity and socioeconomic status(4); based on the 2006 and 2008 Behavioral Risk Factor (BRFSS) surveillance system, 9.1% of the US population met the criteria for depression(5). In both reports, depression increased with age, women were more likely to have symptoms of depression than men, and less than half of people with depression reported contacting a doctor or a healthcare professional.
Aspects of depressive episodes
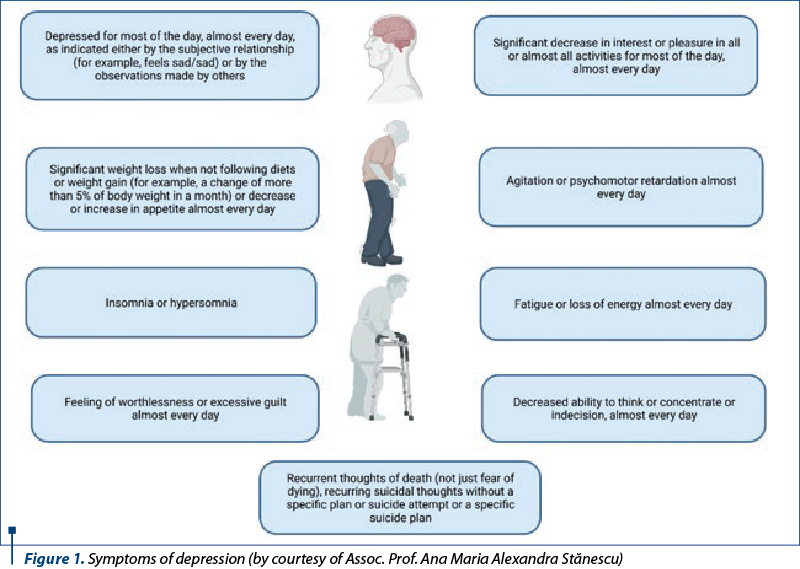
A major depressive episode according to DSM-5 (Diagnostic and Statistical Manual, Fifth Edition, of the American Psychiatric Association) criteria is defined by the occurrence of five or more of the following important symptoms of depression in at least two weeks, almost every day, and most of the day (Figure 1). Depression and anhedonia are the mandatory symptoms(6).
Minor depression – included in the DSM-5 at “Other specific and non-specific disorders” – is the depressive state involving two to four associated symptoms, lasting at least two weeks, but less than two years(7).
Dysthymic disorder is a chronic mood disorder less severe than major depression that lasts two years or more. It rarely begins towards the end of life, but can persist from adulthood to old age. To diagnose an elderly adult, he or she must have been depressed for at least two years, along with two of the following symptoms: eating disorders, sleep disorders, low energy or fatigue, low self-esteem, poor concentration, or difficulty decision making and feelings of hopelessness(8).
It has also been described a depression syndrome without sadness, considered more common in older adults, or a syndrome of exhaustion manifested by withdrawal, apathy and lack of vigor(9).
The impact of depression in the elderly
In 2014, approximately 7.1% of people aged 55-64 years old in the European Union had depressive symptoms in the 12 months prior to the survey, being less frequent (6.5%) among people aged between 65 and 74 years old (when most older people were already retired), but more frequent (13.1%) among people aged 75 or over (when there is an increased risk of living alone, along with the loss of personal independence and with mobility problems)(10).
Among the US population aged 65 and over, 4.1% reported major depression, 5.1% reported other depressions, and 9.1% reported any depression in 2006, according to NHANES(5).
According to NHANES data from 2005 to 2010, 61.72% of people aged 65 and over reported having at least one symptom of depression in the two weeks prior to the survey. The most common symptoms reported in this age group included “apathy in doing things”, “lack in energy or flagging”, “insomnia” and “feeling down, depressed or useless”. Among those with at least one symptom of depression, 23.72% reported that their symptoms caused them extreme difficulties in their daily life(11).
A potential biological cause of depression is the imbalance of neurotransmitters involved in disposition regulation. Different neurotransmitters, including norepinephrine, serotonin and dopamine, play an essential role in mood regulation(12). Although this statement is often mentioned as a significant cause of depression, it remains unproven. Many experts in the field believe it does not fully explain the clinical manifestations and the different factors that are supposed to contribute to depression.
The causes of depression are presented in Figure 2.
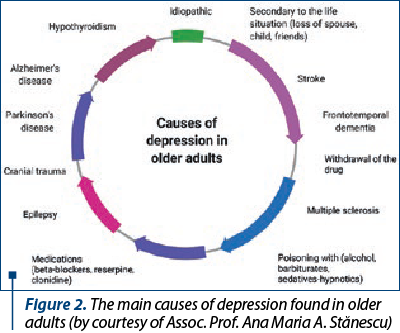
Chronic illness, sleep disorders or thyroid disorders predispose to depressive symptoms. Depression rates also tend to be higher among sick people suffering from cancer, diabetes, chronic pain or multiple sclerosis. Diseases are related to depression in the following way: on one hand, the stress of suffering from a chronic illness can trigger an episode of major depression and, on the other hand, certain diseases, such as liver pathologies, thyroid disorders or Addison’s disease, along with medication, can induce various symptoms of depression(13).
The probability ratios for major depressive episode disorder increase linearly with medical comorbidity, as calculated in a study of patients with acute myocardial infarction(14).
Also, a meta-analysis comparing the elderly without chronic diseases with those with chronic diseases found that chronic diseases represent a predictor factor for the occurrence of depression in patients with chronic diseases(15,16).
Hormonal factors are also found to play a role in depression. Women present major depression about twice as often as men, most likely due to hormones and to depressive disorders during the reproductive periods(17), such as mood disorders during menstruation, depression in pregnancy and postpartum period or in perimenopause and menopause.
A family history of parents with depression is another high-risk factor. Depressive symptoms may occur in a person with other family members who suffer from depression or another type of mood disorder. It is believed that depression is genetically determined in approximately 40% of cases(17).
Regarding cognitive disorders, depression is associated with mild cognitive impairment and dementia(18,19); the reported prevalence of depression in people with cognitive impairments is between 20% and 50%(20,21).
Studies have suggested that depression is triggered by the transformations of glucocorticoids that damage the hippocampus, resulting in subsequent cognitive decline(22).
Several lifestyle factors may have a determining role in causing depression. Harmful habits, such as drinking alcohol in excess, tobacco, obesity and low physical activity, are found among people with depression(23).
A particular type of depression – seasonal affective disorder (officially diagnosed as a major seasonal depressive disorder) – is thought to be caused by a disorder of the circadian rhythm(24).
Some studies have found the relationship between diet and depression; depression is associated with high-sugar diets, low intake of omega-3 fatty acids or with an unbalanced ratio of omega-6 to omega-3(25,26).
Stressful life events, which affect a person’s capacity to cope, can also cause depression(24). After losing a beloved one, extremely inadaptable grieving people have many of the same symptoms of depression. Insomnia and sleep disorders, poor appetite and loss of feelings and of pleasure, or losing interest in activities are normal responses for a period of time(27).
Drugs and alcohol can contribute to depressive disorders. However, even some prescription drugs have been linked to depression. Some medications that are associated with depression include benzodiazepines, anticonvulsants, statins, corticosteroids, stimulants and beta-blockers(28).
In conclusion, depression in older people remains a significant social problem regarding diagnosis and treatment. Different aspects of depressive episodes have an impact on the quality of life in the elderly.
Bibliografie
The Human Face of Mental Health and Mental Illness in Canada, 2006. Accessed: July 24, 2021. Available at: www.phac-aspc.gc.ca.
Marcus M, Yasamy MT, Ommeren M, Chisholm D, Saxena S, Van Ommeren M. Depression: a global public health concern. World Health Organization Paper on Depression. 2012;6-8.
Wang PS, Simon G, Kessler RC. The economic burden of depression and the cost-effectiveness of treatment. Int J Methods Psychiatr Res. 2003;12(1):22-33. doi:10.1002/mpr.139.
Pratt LA, Brody DJ. Depression in the United States household population, 2005-2006. NCHS Data Brief. 2008 Sep;(7):1-8. PMID: 19389321.
Current Depression Among Adults – United States, 2006 and 2008. Accessed: July 24, 2021. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5938a2.htm
Depression Definition and DSM-5 Diagnostic Criteria. Accessed July 25, 2021. Available at: https://www.psycom.net/depression-definition-dsm-5-diagnostic-criteria/
Thomas E, Sedat S. The diagnosis and management of depression in the era of the DSM-5. South African Family Practice. 2018;60(1):22-28.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed., 2000.
Gallo JJ, Rabins PV, Lyketsos KG, Tien AY, Anthony JC. Depression without sadness: Functional outcomes of nondysphoric depression in later life. J Am Geriatr Soc. 1997;45(5):570-578. doi:10.1111/j.1532-5415.1997.tb03089.x
Ageing Europe – Looking at the Lives of Older People in the Eu – 2020 edition. Available at: https://ec.europa.eu/eurostat/web/products-statistical-books/-/ks-02-20-655
Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: US Department of Health and Human Services, CDC, 2005-2010. Available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
Weissman MM, Berry OO, Warner V, et al. A 30-year study of 3 generations at high risk and low risk for depression. JAMA Psychiatry. 2016;73(9):970-977. doi:10.1001/jamapsychiatry.2016.1586
Ng E, Browne CJ, Samsom JN, Wong AHC. Depression and substance use comorbidity: What we have learned from animal studies. Am J Drug Alcohol Abuse. 2017;43(4):456-474. doi:10.1080/00952990.2016.1183020
Watkins LL, Schneiderman N, Blumenthal JA, et al. Cognitive and somatic symptoms of depression are associated with medical comorbidity in patients after acute myocardial infarction. Am Heart J. 2003;146(1):48-54. doi:10.1016/S0002-8703(03)00083-8
Chang-Quan H, Xue-Mei Z, Bi-Rong D, Zhen-Chan L, Ji-Rong Y, Qing-Xiu L. Health status and risk for depression among the elderly: A meta-analysis of published literature. Age Ageing. 2009;39(1):23-30. doi:10.1093/ageing/afp187
Blazer DG, Sachs-Ericsson N, Hybels CF. Perception of unmet basic needs as a predictor of depressive symptoms among community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2007;62(2):191-195. doi:10.1093/gerona/62.2.191
Lohoff FW. Overview of the genetics of major depressive disorder. Curr Psychiatry Rep. 2010;12(6):539-546. doi:10.1007/s11920-010-0150-6
Sachs-Ericsson N, Blazer DG. Depression and anxiety associated with dementia. In: Lippincott Williams & Wilkins; 2006, 591–603.
Lopez OL, Jagust WJ, Dulberg C, et al. Risk factors for mild cognitive impairment in the cardiovascular health study cognition study. Arch Neurol. 2003;60(10):1394-1399. doi:10.1001/archneur.60.10.1394.
Zubenko GS, Zubenko WN, McPherson S, et al. A collaborative study of the emergence and clinical features of the major depressive syndrome of Alzheimer’s disease. Am J Psychiatry. 2003;160(5):857-866. doi:10.1176/appi.ajp.160.5.857.
Olin JT, Schneider LS, Katz IR, et al. Provisional diagnostic criteria for depression of Alzheimer’s disease: description and review. Expert Rev Neurother. 2003;3(1):99-106. doi:10.1586/14737175.3.1.99.
Sachs-Ericsson N. The Influence of Depression on Cognitive Decline in Community-Dwelling Elderly Persons. Am J Geriatr Psychiatry. 2005;13(5):402-408. doi:10.1176/appi.ajgp.13.5.402.
Strine TW, Mokdad AH, Dube SR, et al. The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. Gen Hosp Psychiatry. 2008;30(2):127-137. doi:10.1016/j.genhosppsych.2007.12.008
Yang L, Zhao Y, Wang Y, et al. The Effects of Psychological Stress on Depression. Curr Neuropharmacol. 2015;13(4):494-504. doi:10.2174/1570159x1304150831150507.
Larrieu T, Layé S. Food for mood: Relevance of nutritional omega-3 fatty acids for depression and anxiety. Front Physiol. 2018 Aug 6;9:1047. doi:10.3389/fphys.2018.01047.
Knüppel A, Shipley MJ, Llewellyn CH, Brunner EJ. Sugar intake from sweet food and beverages, common mental disorder and depression: Prospective findings from the Whitehall II study. Sci Rep. 2017;7(1):6287. doi:10.1038/s41598-017-05649-7.
Zisook S, Shear K. Grief and bereavement: What psychiatrists need to know. World Psychiatry. 2009;8(2):67-74. doi:10.1002/j.2051-5545.2009.tb00217.x.
Qato DM, Ozenberger K, Olfson M. Prevalence of prescription medications with depression as a potential adverse effect among adults in the United States. JAMA. 2018;319(22):2289-2298. doi:10.1001/jama.2018.6741





