Corticosteroids have been linked to various neuropsychiatric adverse effects, including mood disorders. This case study describes a post-surgical manic episode (spinal meningioma ablation D11-D12) in a 57-year-old female patient on corticosteroids. This presentation aims to highlight corticosteroids’ potential psychiatric adverse effects and to emphasize the importance of recognizing and treating such complications. In this case, the management strategy involved discontinuing corticosteroids, initiating mood-stabilizing medications, and closely monitoring the symptoms. A mood stabilizer and a second-generation antipsychotic were administered to the patient to treat transient manic symptoms and prevent relapse. After discontinuing corticosteroids and beginning therapy with mood stabilizers, the patient’s bipolar symptoms improved. Psychoeducation and therapeutic support were provided to aid the patient in managing acute symptoms and encourage adherence to the treatment plan. As anxiety persisted after manic symptoms were controlled, the case management involved a psychotherapy technique facilitated by virtual reality. Relaxation breathing techniques were emulated through a virtual reality Oculus Quest 2 headset, improving patient-physician trust, subjectively relieving correlated anxiety, and ensuring therapeutic compliance during the admission and at home. Healthcare professionals must be vigilant to identify and effectively treat these complications of steroid anti-inflammatory medication. Immediate cessation of corticosteroids, the initiation of mood stabilizers and psychoeducation are essential for managing these cases. By presenting this case report, we hope to increase healthcare professionals’ awareness on the psychiatric consequences of corticosteroid use, the necessity of a multidisciplinary therapeutic approach, and the role of add-on virtual reality as integrated, personalized patient care to alleviate anxiety.
Corticosteroid-induced mania after dorsal meningioma surgery. The role of add‑on immersive virtual reality facilitated psychotherapy for anxiety
Episod maniacal indus prin corticoterapie postalblaţie de meningiom spinal. Rolul realităţii virtuale în psihoterapia anxietăţii postoperatorii
First published: 30 iunie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.73.2.2023.8258
Abstract
Rezumat
Administrarea de antiinflamatoare steroidiene este asociată cu efecte adverse neuropsihiatrice, precum tulburările de afective. Acest studiu de caz descrie un episod maniacal cu debut postchirurgical (ablaţia meningiomului spinal D11-D12) la o pacientă de 57 de ani tratată cu corticosteroizi. Această prezentare de caz îşi propune să evidenţieze potenţialele efecte adverse psihiatrice ale corticosteroizilor şi să sublinieze importanţa recunoaşterii şi tratării unor asemenea complicaţii. În acest caz, strategia de management a implicat întreruperea corticosteroizilor, iniţierea medicaţiei timostabilizatoare şi monitorizarea atentă a simptomelor. Un stabilizator de dispoziţie şi un antipsihotic de a doua generaţie au fost administrate pacientei pentru a trata simptomele maniacale şi pentru a preveni recăderea. După întreruperea corticosteroizilor şi începutul terapiei cu stabilizatori ai dispoziţiei, simptomele maniacale ale pacientei s-au îmbunătăţit. Psihoeducaţia şi sprijinul terapeutic au fost oferite pentru a ajuta pacienta în gestionarea simptomelor acute şi pentru a încuraja aderarea la planul de tratament. Deoarece anxietatea a persistat după ce simptomele maniacale au fost controlate, managementul cazului a inclus tehnici de psihoterapie facilitate de realitatea virtuală. Tehnicile de respiraţie de relaxare au fost emulate printr-o cască de realitate virtuală Oculus Quest 2, având ca efect consolidarea relaţiei medic-pacient, ameliorarea subiectivă a anxietăţii şi asigurarea complianţei terapeutice în timpul internării şi la domiciliu. Profesioniştii din domeniul sănătăţii mintale trebuie să fie vigilenţi pentru a identifica şi trata în mod eficient aceste complicaţii ale medicamentelor antiinflamatoare steroidiene. Oprirea imediată a corticosteroizilor, iniţierea stabilizatorilor de dispoziţie şi psihoeducaţia sunt esenţiale pentru gestionarea acestor cazuri. Prin prezentarea acestui caz, sperăm să creştem nivelul de conştientizare al profesioniştilor din domeniul sănătăţii cu privire la consecinţele psihiatrice ale consumului de corticosteroizi, să subliniem necesitatea unei abordări terapeutice multidisciplinare şi, nu în ultimul rând, rolul realităţii virtuale ca interfaţă de îngrijire personalizată a pacientului pentru atenuarea anxietăţii.
Introduction
Corticosteroids, widely used for their potent anti-inflammatory and immunosuppressive properties, have been linked to neuropsychiatric side effects, including mood disorders. Most patients develop adverse psychiatric symptoms within the first week of corticosteroid administration, and 90% within six weeks. Prednisolone was most often associated with psychiatric disorders, and women were more likely to develop them.
Corticosteroid-induced manic episodes are relatively uncommon but clinically significant. Corticosteroids are commonly prescribed to medical and surgical patients, but the incidence, presentation and treatment of neuropsychiatric manifestations have not been widely studied. Corticosteroids have been used for over 60 years to treat a variety of pathologies, with up to 10% of inpatients receiving corticosteroids and 2-3% of the general population being on long-term glucocorticoid treatment(1). A large study from the United Kingdom found that suicides and suicide attempts were seven times more prevalent in those who were prescribed steroids for a condition than in those who had not received the medication(2). A retrospective descriptive study from April 2023 found that anxiety was the most common psychiatric disorder, followed by psychological, sexual dysfunction, and affective disorders(3). We present a case of corticosteroid-induced mania and psychosis, emphasizing a highly unusual course and resolution. The incidence, risk factors and treatment options are discussed. The case management included a virtual reality-facilitated psychotherapy approach for alleviating concurrent anxiety.
Case report
A 57-year-old patient was admitted for the first time within the “Socola” Institute of Psychiatry, Iaşi, being brought by the family to the psychiatric emergency unit on 1 June 2023, in the context of symptomatology manifested by hyperthymic positive mood with an increase in self-esteem, feelings of grandeur, decreased need for sleep without the association of daytime fatigue for approximately 26 days, the symptomatology being accentuated post-spinal meningioma ablation seven days before current hospitalization. In the guard room, the patient stood out for maneuverability in conversation, flight of ideas, significant distractibility and psychomotor agitation marked with verbal and physical hetero-aggression in the context of affective inversion towards her sons.
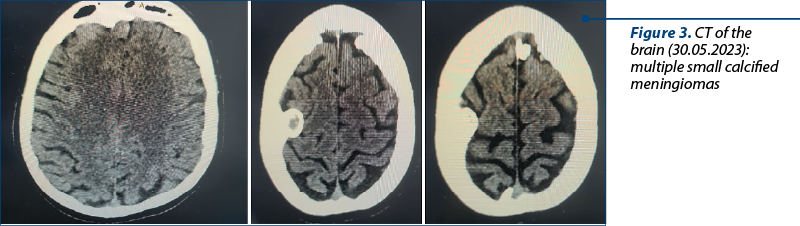
The heredo-collateral antecedents objectified by a short psychogenogram – respectively, the personal pathological ones – did not reveal relevant information concerning the predisposition to a mental disorder. The patient was diagnosed with the following: multiple small calcified cerebral meningiomas (CT of the brain – 30.05.2023), grade I spinal meningioma D11-D12 (diagnosed in March 2023, admitted in the neurosurgical department in 3.05.2023 for surgery), sensitive paraparesis, euthyroid nodular goiter, first-degree obesity, frequent episodic tension-type headache, possible type 2 diabetes, presbyopia.
The treatment at home consisted of omeprazole 40 mg preprandial, dexamethasone two vials of 2 ml in a concentration of 4 mg/ml intramuscularly/day (16 mg/day) – started four weeks ago, during the admission in the neurosurgical department, gabapentin 300 mg every 8 hours, Thiossen® 1 cp./day, Milgamma® 2 cp./day, melatonin 3 mg, 2 cp./day.
The treatment recommended in the emergency was valproic acid, extended release, 1000 mg, diazepam one vial, 2 ml – 10 mg intramuscularly in the superior gluteal muscle, quetiapine prolonged release 300 mg at 19:00, and clonazepam 2 mg, 1 cp., at 20:00.
The follow-up and reevaluation two hours after admission revealed the amplification of psychomotor agitation with the integration into the intrahospital environment, the patient becoming verbally and physically hetero-aggressive towards patients, presenting a flight of ideas and the main activity was represented by tearing leaves from a tree in the garden of the pavilion and collecting them in a net, to use them for cooking.
Later, contact was made with the on-call neurosurgery doctor at the “Prof. Dr. Nicolae Oblu” Clinical Hospital of Neurosurgery, Iaşi, to discuss the possibility of withdrawing the dexamethasone due to possible adverse effects, on the etiological hypothesis of the psychiatric symptomatology.
The second dose of diazepam, one vial of 2 ml (10 mg), was performed intramuscularly, and 14 drops of haloperidol solution 2 mg/ml (1.4 mg haloperidol) were administered.
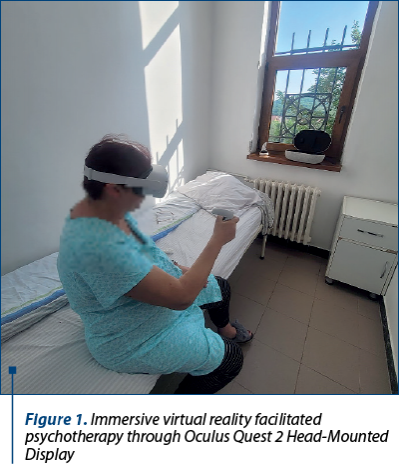
Figure 1. Immersive virtual reality facilitated psychotherapy through Oculus Quest 2 Head-Mounted Display
The reevaluation, four hours after admission, revealed the persistence of agitated symptoms. The patient was administered treatment in the evening (clonazepam 2 mg). The patient fell asleep, maintaining a deep sleep throughout the night. The next day, she was overwhelmed by the reactions that the rest of the patients attribute to her behavior during admission day; the agitation and the logorrhea persisted, although sleep was induced and appropriately maintained under psychotropic medication. As anxiety persisted, relaxation psychotherapy techniques facilitated by virtual reality were discussed, and primary contraindications to virtual reality exposure, such as commemorative seizures, were checked.
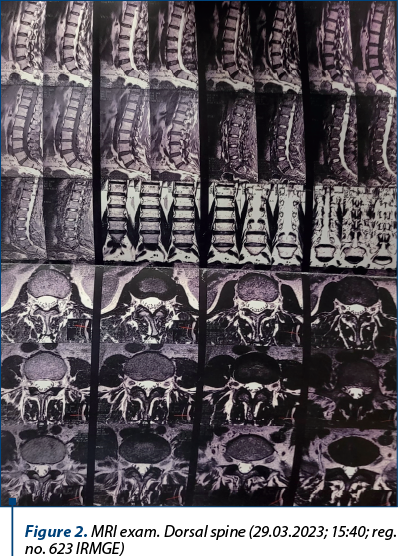
Figure 2. MRI exam. Dorsal spine (29.03.2023; 15:40; reg. no. 623 IRMGE)
The psychotropic treatment during admission was represented by valproic acid, extended release, 1 g every 12 hours, diazepam, one vial of 2 ml, 10 mg in case of psychomotor agitation (discontinued later in the context of the objectification of the paradoxical reaction). Relaxation breathing techniques were emulated through a virtual reality Oculus Quest 2 headset using various software resembling different manners of exploring remote corners of the world, such as Fuji Mountain, remote islands, beaches and mountain landscapes in which the patient could freely walk to find a mental sanctuary. This aspect improved patient-physician trust and ensured optimal therapeutic compliance during the admission. The patient was discharged with the recommendation of continuing the treatment with valproic acid, extended release, 500 mg, every 12 hours, and quetiapine, extended release, 600 mg, at 19:00, and also psychotherapy for the stressful surgical experience to integrate the current outcome or at least continuing the breathing exercises learned during admission until the one-month follow-up.
Interpretation of the MRI: expansive intradural, extramedullary formation, with insertion at the level of the anterior dura, and with the upper limit at the level of a horizontal plane passing through the upper one-fourth of the vertebral body D11 and the lower limit at the level of a horizontal plane passing through the intervertebral disc D11-D12, in iso-signal T1, discrete hypersignal T2, STIR with intense and homogeneous contracture, with discrete dural tail associated in the lower portion with approximate dimensions 13/18.5/24 mm (AP/T/CC). The formation causes a significant mass effect on the cervical medullary cord, which it moves posterolaterally to the left and reduces it to an AP diameter of approximately 5 mm. Slight dextroconcave dorsal scoliotic attitude.
Minimal degenerative arthrosis changes, with the presence of small marginal osteophytes predominantly posterolaterally, hypertrophy of the yellow ligaments, and early disc dehydration.
Abdominal ultrasonography revealed intense meteorism, objectifying a hyperechoic, well-defined image of 26 mm – angiomyolipoma and a fibromatous uterus.
Management algorithm
A mood stabilizer and a second-generation antipsychotic were administered for the patient’s clinical presentation, with medical history and potential drug side effects assessment, helping the patient in treating transient manic symptoms and preventing relapse. The choice of mood stabilizer was based on the patient’s clinical presentation, medical history and potential drug interactions. After discontinuing corticosteroids and beginning therapy with mood stabilizers, the patient’s bipolar symptoms progressively improved.
Psychoeducation and therapeutic support: the patient and her family received psychoeducation regarding manic episodes and the potential association with corticosteroid use. Supportive therapy was instituted to aid the patient in managing acute symptoms and encourage adherence to the treatment plan.
Regular visits were scheduled to monitor the patient’s symptoms, medication response and the adverse effects.
This case exemplifies corticosteroid therapy’s potential adverse psychiatric effects, specifically manic episodes. Healthcare professionals must be vigilant to identify and effectively treat these complications. Immediate cessation of corticosteroids, initiation of mood stabilizers, and psychoeducation were essential for managing this case.
Discussion
The incidence of neuropsychiatric effects of corticosteroids is not entirely understood, with reports ranging from 2% to 60%, and a weighted average of 6%. Most patients will develop symptoms within the first week of treatment and 90% within six weeks. It is estimated that 20% of patients receiving high-dose corticosteroids will develop a psychiatric disorder severe enough to require pharmacotherapy(3).
A retrospective descriptive study published in April 2023 regarding the side effects of corticosteroid medication revealed that anxiety was the most prevalent psychiatric disorder, followed by psychological, sexual dysfunction and affective disorders. Prednisolone was the most frequently drug associated with the development of psychiatric disorders, and females were more likely to develop side effects from corticosteroids(4).
Case novelty
This case is noteworthy because the patient manifested a psychiatric disorder following four weeks of treatment with a dose of dexamethasone of 16 mg daily. The manic symptoms did not subside until the dexamethasone was not discontinued, and we currently question the necessity of continuing dexamethasone after the expansive spinal process was removed, therefore emphasizing iatrogenic implications. The current presentation suggests a possible causal relationship between modest doses and long-term use of dexamethasone and mania. It has been suggested that the onset of psychiatric symptoms correlates with the dose of dexamethasone, but psychiatric symptoms can occur even at modest concentrations. To our knowledge, severe manic episodes following long-term low-dose of dexamethasone administration are uncommon(5). A single case reports that bortezomib and dexamethasone treatment caused psychiatric symptoms such as sleep deprivation, low self-esteem and excessive discourse. Quetiapine was administered to treat these symptoms, and the symptoms of mania gradually improved after treatment(6).
Virtual reality (VR) shows promise as a therapeutic modality for reducing anxiety symptoms in manic patients. Virtual reality’s immersive and interactive nature allows for individualized, immersive and controlled exposure to anxiety-provoking stimuli, while providing relaxation and cognitive restructuring opportunities. The existing evidence suggests that VR interventions have the potential to complement standard treatment approaches and improve outcomes in patients with mania, despite the limited number of studies available. Further studies are needed to determine the efficacy, optimal intervention protocols and long-term effects of virtual reality in this specific population. Integrating VR into routine clinical practice may revolutionize anxiety management in patients with mania, providing a novel and practical treatment approach.
Conclusions
This case exemplifies corticosteroid therapy’s potential adverse psychiatric effects, specifically manic episodes. Healthcare professionals must be vigilant in identifying and treating these complications, including discontinuing corticosteroids, initiating mood stabilizers, and pursuing psychoeducation and psychotherapy facilitated by technologies such as virtual reality.
Funding. The virtual reality equipment in this study was funded through a “Grigore T. Popa” PhD Scholarship.
Consent. The patient mentioned above permitted the authors to publish this case.
Guarantors. The guarantors of this article are: Assist. Prof. Dr. Găină Marcel-Alexandru – the physician who admitted the patient and the patient’s primary physician during admission, and Dr. Florin Anton Petruţ, who was the patient’s psychiatry intern during admission within the “Socola” Institute of Psychiatry, Iaşi.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
- Donihi AC, Raval D, Saul M, Korytkowski MT, DeVita MA. Prevalence and predictors of corticosteroid-related hyperglycemia in hospitalized patients. Endocr Pract. 2006 Jul-Aug;12(4):358-62.
- Bhangle SD, Kramer N, Rosenstein ED. Corticosteroid-induced neuropsychiatric disorders: review and contrast with neuropsychiatric lupus. Rheumatol Int. 2013 Aug;33(8):1923-32.
- Lewis DA, Smith RE. Steroid-induced psychiatric syndromes. A report of 14 cases and a review of the literature. J Affect Disord. 1983;5(4):319-32.
- Alturaymi MA, Almadhi OF, Alageel YS, Bin Dayel M, Alsubayyil MS, Alkhateeb BF. The Association Between Prolonged Use of Oral Corticosteroids and Mental Disorders: Do Steroids Have a Role in Developing Mental Disorders?. Cureus. 2023;15(4):e37627.
- Fujii R, Konishi Y, Furusawa R, Okamoto N, Yoshimura R. Mania after long-term treatment with daily 10 mg prednisolone. Psychiatry Clin Neurosci Rep. 2022;1:e66.
- Geniş B, Coşar B. Bortezomib ve Deksametazon Kullanımına Bağlı Gelişen Mani Olgusu [Mania Associated with the Use of Bortezomib and Dexamethasone]. Turk Psikiyatri Derg. 2018;29(3):209-215.