Dialectical behavioral therapy (DBT) is a principle-based therapy derived from behavioral therapy and developed by Marsha Linehan in 1980 for suicidal patients and for those with substance use disorders. At present, DBT is the recommended therapy for borderline personality disorder, but it can also be used for other disorders that involve emotional dysregulation. The introduction of DBT in Romania, in Hope Clinic, in 2016, made this important approach available for Romanian patients. Developing comprehensive DBT in Romania is a very important next step, with scientific research being started to validate its benefits for this population.
Introducerea terapiei dialectic-comportamentale în România
Introduction of dialectical behavioral therapy in Romania
First published: 30 noiembrie 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.71.4.2022.7330
Abstract
Rezumat
Terapia dialectic-comportamentală (DBT) este o terapie bazată pe principii, derivată din terapia comportamentală şi dezvoltată de Marsha Linehan în 1980 pentru pacienţii suicidari şi cu tulburări ale uzului de substanţe. În prezent, DBT este terapia recomandată pentru tulburarea de personalitate borderline, dar poate fi, de asemenea, utilizată pentru alte tulburări care implică dereglare emoţională. Introducerea DBT în România, în Clinica Hope, în anul 2016, a făcut ca această abordare importantă să fie disponibilă şi pentru pacienţii români. Dezvoltarea DBT comprehensive în România este un pas următor foarte important, cercetarea ştiinţifică fiind demarată pentru a valida beneficiile terapiei pentru această populaţie.
The borderline personality disorder is a complex and severe condition characterized by emotional instability, serious dysfunctions and frequent suicidal and parasuicidal behaviors. Psychotherapy is the main line of intervention, and the methods with efficiency studies are: dialectical behavioral therapy (DBT), mentalization-based therapy, schema-focused therapy, transference-based therapy, and psychodynamic therapy(5). DBT is the most studied and with experimental proven efficacy method, being the first recommendation in all international guidelines(6).
None of these therapies was available in Romania as a comprehensive application and this is the reason why we made the effort to implement the first complete DBT program at Hope Clinic, in Romania.
Dialectical behavioral therapy is a therapy method that is based on behavioral therapy whose purpose is to create a life worth living(1). It is based on cognitive-behavioral therapy frame to which there have been added multiple philosophical and humanist concepts that emphasize acceptance, validation, relationship and synthesis. Many concepts come from Zen-Buddhist philosophy, but they have been adapted to Western culture, without religious connotations. Mindfulness constitutes an essential part of dialectical behavioral therapy(1).
DBT was developed by Marsha Linehan, between 1970 and 1980, as a scientific method to improve the outcome for severely suicidal patients. It was initially developed for people with suicidal attempts and self-harming behaviors (NNSI), diagnosed with borderline personality disorder (BPD)(1).
Marsha Linehan observed some difficulties clients had with the current therapies available at that time:
-
the emphasis on change invalidated the emotions, thoughts and behaviors of BPD people, and the clients easily gave up therapy or became angry with the therapist;
-
the clients had an extremely difficult relationship with the therapist, conflicts in the relationship often strengthening the destructive behaviors and making the work towards change impossible;
-
the CBT format was inappropriate and insufficient to treat numerous problems – suicide attempts, self-harm behaviors, quitting therapy, refusing to do homework between sessions, depression, anxiety, eating disorders etc.
What Marsha added was to introduce strategies such as mindfulness, dialectical vision, validation, irreverent communication techniques, and to build therapy around a biosocial theory of borderline disorder.
This theory states that borderline disorder is built on an emotional structure with difficulties related to the regulation of emotions that is exposed repeatedly in childhood to various forms of emotional invalidation (from instability to abuse). The lack of an acceptable and supportive environment has led to a lack of learning of emotional and interpersonal regulation and self-regulation skills. That is why teaching these skills becomes an essential part in the first part of the treatment.
Emotional dysregulation, with intense emotions, is seen at the root of the disturbances determining all areas affected in BPD. Problem behaviors are seen as a solution found by the patients to regulate difficult emotions or reactions directly linked to intense emotions. They appear as an attempt to reduce suffering, and cognitive schemas alterations are also a consequence of this emotional sensitivity(1).
The biosocial theory in DBT states that epigenetic emotional vulnerability is in a transactional relation with the invalidating environment. Emotional vulnerability is a biological predisposition to high sensitivity to emotional stimuli, as well as to more extreme and long-lasting emotional reactions. The invalidating environment did not provide skills for managing intense emotional responses and increased emotionality through trauma, neglect, abuse or invalidation.
The word dialectic means the synthesis or integration of opposite parts. A lower capacity for integration and a dichotomous, black and white vision of life are a defining feature of many people with marked emotional instability. The main dialectic in DBT is acceptance versus change. It requires that the therapist accepts the client as he is and, at the same time, takes into account that he needs to change in order to achieve his goals of change. Also, the client needs to accept who he is, what he does, what he feels without judgment, guilt or shame and, at the same time, find ways to change.
Principles of the dialectical perspective
The principle of interconnection and totality: the parts of a system are known and defined in relation to the whole; everything is interconnected at the level of cosmos, nature, society, family, life and intrapsychic dynamics.
The principle of polarity: reality is not static and is made up of opposite forces that give rise to a synthesis. The obtained synthesis determines the emergence of other opposing forces that create a synthesis, and so on. “Opposing truths do not contradict each other and do not dominate each other, but stand next to each other, inviting participation and experimentation”(7).
The principle of continuous change: change is an inevitable process. Everything is changing, it’s constantly evolving. “Change is the essential nature of life.”(1)
DBT method invites to stand with the opposing forces at the same time, without rejecting or modifying them, which leads to an internal tension. This tension is the instrument of change and creates the conditions for synthesis, integration and balance.
Currently, DBT is also used to treat substance use disorders, bipolar disorder, post-traumatic stress disorder (PTSD), depression, anxiety with emotional dysregulation traits, and eating disorders. It is also used successfully in case of therapy for adolescents with emotional problems, self-harm, substance use and/or suicidality.
It is the reference therapy (gold standard) worldwide in case of people with BPD, being the main recommendation in case of interventions for these people.
Dialectical behavioral therapy is also one of the most verified methods of therapy, with over 40 RCT studies in multiple countries that have repeatedly proven its effectiveness and ability to bring about change. “In sum, DBT and the related treatments provide the most solid… evidence of efficacy relative to all treatments [for BPD] that have been investigated in RCTs so far.”(8)
DBT is the main form of treatment recommended by the treatment guidelines for borderline personality disorder:
-
American Psychiatric Association, 2010. Practice Guideline for the Treatment of Patients with Borderline Personality Disorder(9).
-
NICE – Borderline Personality Disorder: Recognition and Management Clinical Guideline, 2009(10).
-
Clinical Practice Guideline for the Management of Borderline Personality Disorder, 2012, NHMRC, Australia(11).
-
DBT has the most published efficacy studies, becoming officially evidence-based therapy
-
DBT is designated as having “strong research support” for BPD by the American Psychological Association – Clinical Psychology Division(12).
-
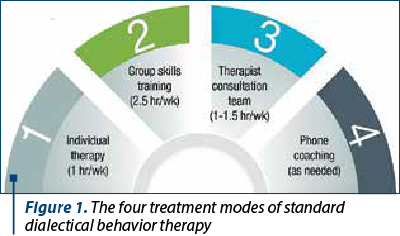
The major difference lies in the structure of the treatment. Comprehensive DBT has four modes, most of the studies on the effectiveness of this therapy being with all four modes:
-
Weekly individual therapy, with unique aspects of therapy related to the order of priorities, diary, validation versus change etc.
-
Skills training (four modules: mindfulness, tolerance to suffering, emotional regulation, and interpersonal efficacy) – mandatory in the first year of therapy.
-
Coaching on the phone with the therapist, when needed, to generalize the use of skills in the necessary moments.
-
Therapeutic team (consultation team) to support the motivation of therapists and to provide support in working with people with BPD. It is a well-known fact that therapy with people who suffer from borderline disorder is difficult, long, with very little progress over many years that can put pressure on the therapeutic relationship. They exhaust the therapists and affect their ability to notice/prevent polarization in therapy and the slip towards conflict and premature termination. This is why the consultation team is a strong support system for the therapists, helping them stay away from burnout.
Stages of treatment in DBT
Stage 1: the goal of the first stages is to obtain the control of destructive behaviors (suicidal attempts, self-learning, drug and alcohol use, frequent sexual relations with unknown partners, gambling addiction etc.). It is considered that the priority is for the patient/client to remain alive and in therapy in order to be able to build together with the therapist “a life that deserves to be lived”.
Stage 2: the goal in stage 2 is to move from despair to emotional experience – that is, to treat emotional suffering and traumatic history, which is part of the BPD diagnosis.
Stage 3: the goal at this stage is to teach the client to live an ordinary life with pleasant and less pleasant things, to define what he wants in life, to build self-respect, to build personal relationships or at work, to find peace and happiness.
Stage 4: this stage is necessary only for some clients, those for whom it is important to find a spiritual meaning for their existence, which also need the spiritual side of life. The goal here is to move from a feeling of incompleteness to a life that permanently involves experiencing joy and freedom.
The main changes brought by the DBT practice:
-
Decreases self-harming behaviors.
-
Decreases the rate of quitting therapy (by over 34%) compared to regular treatment.
-
Decreases the number of hospitalizations and the number of days of hospitalization.
-
Increases the overall adaptation of the person.
-
Anxiety ruminations and angry outbursts decrease.
Individual therapy
Individual therapy includes the completion by the client of a self-monitoring journal of impulses, behaviors, drug use and skills learned in the course and practiced weekly. It is built according to the four stages of treatment described before.
There are three priorities in the individual therapy that are discussed during the sessions:
-
Suicide, self-harming.
-
Behaviors that interfere with the therapeutic relationship (failure to complete the self-monitoring journal, delays in sessions, canceled sessions, verbally aggressive behavior towards the therapist etc.).
-
Behaviors that alter the quality of life.
Dialectical behavioral therapy starts from the assumption that there are truth and meaning in any action or reaction of the client and that the formation of a therapeutic relationship is the basis of the success of the therapy. From a dialectical point of view, DBT synthesizes the relational therapeutic approach with the behavioral one.
The average duration of therapy with a person diagnosed with BPD is 5-7 years and, in the first year of therapy, it is expected the reduction of suicidal and self-harming behaviors.
Skills training(2)
Dialectical behavioral therapy assumes that the invalidating environment and the emotional vulnerability explain the lack of emotion regulation skills. Learning and mastering emotional regulation skills are mandatory for these clients. Teaching them and ensuring support for their generalization in daily life are an essential part of a comprehensive DBT program. The DBT skills training proved to be effective in many disorders beside the ones with severe emotional dysregulation, like in older adults, in depression and anxiety disorder, in autism, ADHD, bipolar disorder, or antisocial personality disorder. Also, it is proven to be effective as general skills for adolescents and children with impulse control and emotional dysregulation.
The main characteristics of the skills trainings are:
-
It lasts 6-8 months, and the frequency is once a week (two hours or two and a half hours).
-
It is recommended to follow the course two times, successively.
-
Individual therapy in parallel is mandatory throughout the course.
It has four modules:
-
Mindfulness – the client learns to be in the here-and-now deliberately, without judgment.
-
Tolerance to suffering – the client learns how to go through situations of emotional crisis without resorting to destructive or impulsive behaviors that he can regret later.
-
Interpersonal effectiveness – the client learns to get what he wants in relationships with others, while keeping relationships and self-respect.
-
Emotional regulation – the client learns to define emotions and decreases his sensitivity, vulnerability and intensity of emotions.
Module 1. Mindfulness
Mindfulness means deliberately consciously living the present moment, without judgment and without attaching yourself to what appears in the present moment (thoughts, emotions, past, future).
Skills focused on acceptance are taught, and these are:
-
Wise mind.
-
“What” skills: Observe, Describe, Participate.
-
“How” skills: No judgment, One thing at a time, Effective.
Module 2. Tolerance to suffering
The skills taught in this module are aimed at finding strategies for crisis situations that we can apply so as not to worsen (even more) the situation. They are skills centered on acceptance and are of two types:
-
Crisis survival skills (short-term use skills for tolerating painful events and emotions, when things cannot be straightened out immediately).
-
Skills for accepting reality as it is.
-
Survival skills in crisis:
-
STOP – momentary blocking of impulsive behavior.
-
TIPP – changing the chemistry of the body (for quick calming of extreme emotions).
-
ACCEPTS distraction (activities, comparisons, contributions, avoidance etc.).
-
Sensory self-soothing (through sight, hearing, touch, taste).
-
Improving the IMPROVE moment (through reverie, meaning, prayer, relaxation etc.).
-
Pros and Cons of crisis impulses.
-
Skills for accepting reality as it is:
-
Radical acceptance (versus change).
-
Benevolence (versus stubbornness).
-
Half smile.
Module 3. Interpersonal efficacy
The skills of this module are aimed at changing the client and are oriented towards what is effective in relationships – that is, towards what works in helping us get what we want.
Types of skills:
-
Techniques to increase assertiveness.
-
Efficient and relational communication.
-
Improving present relationships through validation.
-
Maintaining relationships and self-esteem.
-
Decreased isolation.
Examples of skills: DEAR MAN, GIVE, FAST. Do we decide what skill we apply based on what is important to us in a given situation: the objective (DEAR MAN), keeping the relationship (GIVE), maintaining self-respect (FAST)?
Module 4. Emotional regulation
In this module, oriented towards change, there are taught:
-
To define emotions.
-
To decrease sensitivity to emotions.
-
To decrease vulnerability to negative emotions.
-
To decrease the intensity.
Defining emotions: primary emotions versus secondary emotions, justified emotions versus emotions unjustified to a situation.
Decreased vulnerability
Examples of skills: ABC PLEASE
ABC
- Accumulating positive emotions.
- Build your mastery.
- Cope ahead.
PLEASE
-
Treats physical illnesses (treat physical illness).
-
Balance eating.
-
Avoid mood altering drugs.
-
Balance sleep.
-
Get exercise.
Decreased intensity: mindfulness of current emotions.
Romanian DBT program
“Find your balance” is the only complete program for the implementation of dialectical behavioral therapy in Romania, and it is implemented today in all the five outpatient clinics of the Hope Clinic chain. It includes all the necessary aspects: consultation team, individual therapy, skills training and phone coaching, being the only comprehensive DBT program in Romania. It arose from the need to implement effective and scientifically validated therapies in this field, the long-standing interest of team members in this field, but also at the request of patients. Training of specialists was done in 2016 and in September 2016 the program “Find your balance!” was launched. The beginnings were difficult, as we had to translate all the materials in Romanian and construct all the elements for the comprehensive DBT.
Since then, we have held more than 15 skills training rounds for adults and eight for adolescents, helping more than 400 borderline clients.
Dialectical behavioral therapy is also implemented for adolescents, in a comprehensive program called INSPIR-A.
We also started a training and professional DBT Association called Romanian Dialectical Behavioral Therapy Association, that is organizing official training in DBT with the help of internationally certified trainers from Dialexis and Behavioral Tech. So far, 38 therapists went through the first intensive training organized in 2019 and held by Wies van den Bosch and Dialexis team. At present, 65 therapists are going through the extensive training organized by Behavioral Tech in the most comprehensive training format ever held in the world.
Today, DBT programs are applied in Bucharest, Iaşi and Cluj, for the needs of clients with borderline personality disorder and other related disorders.
The implementation of dialectical behavioral therapy in Romania is necessary and favorable for alleviating the suffering of borderline patients. Generalizing the use of DBT therapy can provide access to treatment for a higher number of affected people. In-depth studies are needed for more results.
Bibliografie
-
Linehan MM. Cognitive Behavioral Treatment of Borderline Personality Disorder, The Guilford Press, 1993.
-
Linehan MM. Skills Training Manual, Second Edition, The Guilford Press, 2015.
-
Linehan MM. Skills Training Handouts and Worksheets, Second Edition, The Guilford Press, 2015.
-
https://behavioraltech.org/
-
Zanarini MC. Psychotherapy of borderline personality disorder. Acta Psychiatr Scand. 2009 Nov;120(5):373-7. doi: 10.1111/j.1600-0447.2009.01448.x.
-
May JM, Richardi TM, Barth KS. Dialectical behavior therapy as treatment for borderline personality disorder. Ment Health Clin. 2016 Mar 8;6(2):62-67. doi: 10.9740/mhc.2016.03.62.
-
Goldberg C. The human circle: An existential approach to the new group therapies. Burnham Incorporated Pub, 1973.
-
Storebø OJ, Stoffers-Winterling JM, Völlm BA, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2020;5(5):CD012955. doi:10.1002/14651858.CD012955.pub2.
-
American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association. Am J Psychiatry. 2001;158(10 Suppl):1-52.
-
Kendall T, Hollis C, Stafford M, Taylor C; Guideline Development Group. Recognition and management of psychosis and schizophrenia in children and young people: summary of NICE guidance. BMJ. 2013;346:f150. doi:10.1136/bmj.f150.
-
Grenyer BF. Improved prognosis for borderline personality disorder. Med J Aust. 2013;198(9):464-465. doi:10.5694/mja13.10470.
-
Van den Bosch LM, Sinnaeve R, Hakkaart-van Roijen L, van Furth EF. Efficacy and cost-effectiveness of an experimental short-term inpatient Dialectical Behavior Therapy (DBT) program: study protocol for a randomized controlled trial. Trials. 2014;15:152. doi: 10.1186/1745-6215-15-152.