Introduction. Hydatidiform mole, also known as molar pregnancy, represents a gestational trophoblastic disease that originates in the placental tissue and has the capacity of producing metastasis. Hydatidiform mole can be divided into two specific types: complete and partial mole. Complete hydatidiform mole is characterized by high levels of beta-HCG and in 90% of cases it has a 46XX karyotype, while the other 10% is represented by a 46XY karyotype. Partial hydatidiform moles usually have a 69XXX or 69XXY karyotype. Materials and method. A 20-year-old female patient presented to the “Elena Doamna” Clinical Hospital of Obstetrics and Gynecology, Iaşi, by transfer from another medical care unit, in April 2023, with the diagnosis of molar pregnancy, hemorrhage, severe anemia, and with two caesareans in her medical history. The clinical examination revealed an enlarged uterus surpassing the umbilicus, and at abdominal palpation, a large, ovoidal, smooth mass could be felt, with its longitudinal axis surpassing the umbilicus with 2-3 cm. Pelvic ultrasound examination suggested the diagnosis of complete hydatidiform mole. The evacuation of the pregnancy was performed by aspiration of the uterine cavity under ultrasound guidance, and with continuous intravenous administration of oxitocine. Results. The patient had a favorable evolution, the post-surgery pelvic ultrasound showing an empty uterus, accompanied by an ovarian hyperstimulation syndrome. The results from the pathological anatomy examination confirmed our diagnosis. Conclusions. This case had a favorable evolution, but the patient’s follow-up was difficult. The particularity of this case consists in its prolonged evolution without symptoms, this being the first medical consultation throughout patient’s entire pregnancy.
A rare case of complete hydatidiform mole with prolonged evolution – clinical case
Un caz rar de molă hidatiformă completă cu evoluţie îndelungată – prezentare clinică
First published: 30 septembrie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.41.3.2023.8735
Abstract
Rezumat
Introducere. Mola hidatiformă, cunoscută drept sarcină molară, reprezintă o boală gestaţională trofoblastică cu punct de plecare placentar şi capacitate de metastazare. În cazul molelor complete, nivelul de beta-HCG este mult crescut, iar cariotipul este reprezentat în 90% din cazuri de 46XX şi în 10% din cazuri de 46XY. Molele parţiale au de obicei un cariotip triploid, de tipul 69XXX sau 69XXY. Materiale şi metodă. O pacientă în vârstă de 20 de ani, din mediul rural, s-a internat prin transfer în cadrul Spitalului Clinic de Obstetrică şi Ginecologie „Elena Doamna”, Iaşi, în aprilie 2023, cu diagnosticul de sarcină molară, hemoragie, anemie severă şi uter dublu cicatricial. La examinarea clinică se observă uterul mărit de volum până în etajul supraombilical, iar la palpare abdomenul este ocupat de o formaţiune ovoidală, netedă, regulată, cu axul mare longitudinal ce se întinde până la 2-3 cm supraombilical. Examenul ecografic a completat diagnosticul de molă hidatiformă completă. S-a practicat evacuarea sarcinii prin aspiraţia cavităţii uterine sub ghidaj ecografic şi perfuzie ocitocică. Rezultate. Evoluţia pacientei a fost favorabilă, ecografia postintervenţională punând diagnosticul de uter gol şi sindrom de hiperstimulare ovariană. Rezultatul anatomopatologic a confirmat diagnosticul. Concluzii. Cazul a avut o evoluţie favorabilă, însă urmărirea pacientei pe termen lung a fost dificilă. Particularitatea cazului constă în evoluţia îndelungată a acestui tip de sarcină fără simptomatologie, până la momentul primei prezentări la unitatea de primiri urgenţe, pentru sângerare pe căile genitale externe.
Introduction
Hydatidiform mole, also known as molar pregnancy, represents a subcategory of trophoblastic gestational disease which originates in the placental tissue and has the capacity of producing metastasis. Other forms of gestational trophoblastic disease are represented by the gestational choriocarcinoma, with high potential of metastasizing and mostly malignant, or the placental site trophoblastic tumor. Hydatidiform mole can be divided into two types: complete or partial mole(1,2). The complete form is more frequently encountered; they are typically diploid forms and are accompanied by higher levels of beta-HCG. Karyotype is in 90% of cases 46XX, and in 10% of cases, 46XY. This type of pregnancy appears when an oocyte without genetic material is fertilized by two spermatozoa or by haploid spermatozoa that doubles its own genetic material. When it comes to partial mole, the karyotype is in 90% of cases triploid, type 69XXX or 69XXY, this type appearing when a haploid oocyte is fertilized by a spermatozoa that doubles its own genetic material or by two spermatozoa(3,4). The risk factors identified for this pathology are related to the extreme ages of the patient, ethnic factors or a medical history of molar pregnancies. One study performed by Kohorn et al. compared the risk of developing gestational trophoblastic disease among patients with ages from 21 to 35 years old and in patients older than 35 years of age or younger than 21 years old, and concluded that patients with ages between 21 and 35 years old have lower chances of developing this disease. Among conclusions, the authors stated that, for patients older than 40, the risk is 7.5 times higher(5).
Epidemiological studies reported a high variability for molar pregnancy. The highest incidences were identified in Japan and South-East Asia, reporting two cases at 1000 pregnancies. In the United States of America, an incidence of 1 in 600 therapeutic interruption of pregnancies and an incidence of 1 in 1500 pregnancies have been reported. Approximately 20% of these patients will show a progression towards malignancy, needing chemotherapy after the evacuation of the molar pregnancy. In USA, choriocarcinoma develops in 1 of 20,000-40,000 pregnancies, of which half appear after pregnancies that developed to term. A quarter appear after molar pregnancies, and another quarter appear after other trophoblastic maladies(5).
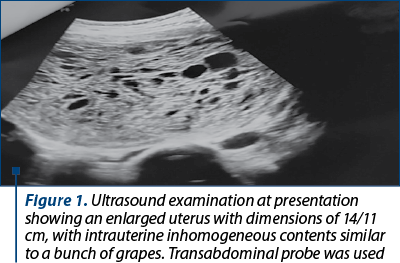
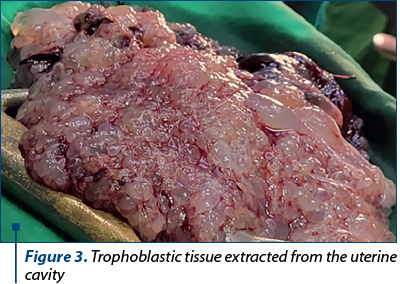
Hydatidiform mole is characterized by an excessive development of the villous trophoblastic tissue. The macroscopic aspect of this tissue can be differentiated starting with the second trimester, due to its multiple cystic aspect similar to a cluster of grapes. In partial molar pregnancy, the diagnosis is confirmed by the fetal or embryo presence or just tissues of this origin, in comparison with complete molar pregnancy where fetal or embryonic tissue is absent(6).
With the development of the ultrasound examination, molar pregnancy diagnosis began to be suspected with the early stages of pregnancy, from the first trimester. The most frequent symptom is represented by bleeding through external genital tract in the first trimester, followed by hyperemesis gravidarum due to high levels of beta-HCG. Patients who perform their first obstetrical consultation later in pregnancy can even present the elimination of trophoblastic tissue through the inferior genital tract, looking like a bunch of grapes. Between 14 and 16 weeks of pregnancy, signs of hyperthyroidism such as tremor or tachycardia can be frequently observed, due to the molecular similarity between HCG and thyroid hormones. At 20 weeks of pregnancy and even later, specific signs of preeclampsia can appear and they can be associated with respiratory distress due to embolism of the trophoblastic tissue.
An important feature observed in more than 50% of complete molar pregnancy is the discrepancy between the high uterine volume compared with the lower gestational age, contrary to partial molar pregnancy that shows a smaller uterine volume compared with the approximated gestational age(7,8).
Pelvic ultrasound represents the gold standard, being a noninvasive technique of diagnosis. The specific image we expect to encounter is one of a bunch of grapes, but sometimes it can be difficult to assess such an image during the first trimester. Contrary to the accessibility given by ultrasound examination, most molar pregnancies that end up in spontaneous abortion during the first trimester have their diagnosis confirmed only by results from the anatomical pathology examination of the intrauterine obtained tissue(8-11).
The first line of treatment consists in dilatation and evacuation of the uterine cavity with the help of ultrasound guidance and with intravenous perfusion with oxytocin. When it comes to patients who no longer desire pregnancies, hysterectomy represents an option. Medical treatment is still controversial and too little studied to be implemented. Intravenous perfusion with oxytocin during evacuation of pregnancy is constantly used, but the risk of positively influencing the rates of metastasizing should be taken in consideration(12-14).
All patients with molar pregnancies need a thorough checkup for beta-HCG values after the surgical intervention, in order to early identify the development of post-molar gestational trophoblastic neoplasia. According to the American College of Obstetrics and Gynecology, beta-HCG values monitoring consists in weekly dosage until undetectable values and which remain so for three weeks. Afterwards, beta-HCG should be checked monthly for six months; if it remains undetectable, the patient can try to obtain a new pregnancy.
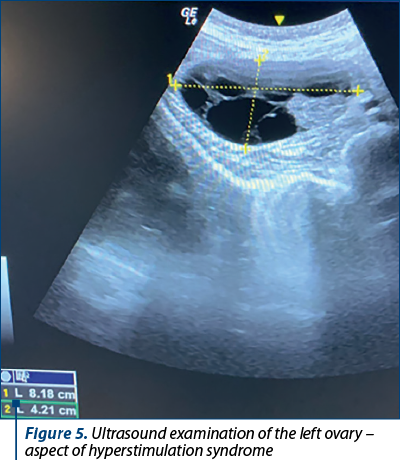
If after the evacuation the beta-HCG values remain high or increase through a period of a couple of weeks, then the diagnosis of gestational trophoblastic neoplasia is imposed. The diagnosis is assessed with the help of FIGO criteria, as it follows: beta-HCG values remain high with a variability marge of 10%, beta-HCG values increase with more than 10% through three dosages in two weeks or beta-HCG values remain detectable after six months post-uterine evacuation(5). Considering that patients with molar pregnancies have a high risk of developing gestational trophoblastic disease, certain risk factors should be taken in consideration, such as: values of beta-HCG higher than 100,000 mUI/mL, the presence of ovarian luteal cysts with a diameter higher than 6 cm, or patient’s age above 35 years old. In accordance with the internal protocol of each medical unit, patients could receive prophylactic chemotherapy. All patients with gestational trophoblastic disease require a thoracic X-ray evaluation in order to infirm or confirm the presence of metastasis(15).
Materials and method
In April 2023, a 20-year-old patient from rural area was sent to the “Elena Doamna” Clinical Hospital of Obstetrics and Gynecology, Iaşi, through transfer from another medical care unit, with the diagnosis of molar pregnancy, genital hemorrhage, severe anemia, and two cesareans in her medical history.
At presentation, the communication with the patient seemed difficult, this consult at the emergency department being her first obstetrical consultation during the present pregnancy. Her presentation to the emergency department was determined by the bleeding through external genital tract and by uterine contractions. From her medical history, we noted two anterior caesarean interventions, in 2016 and 2020, without any complications, with no spontaneous or by request abortions. The patient was unable to provide the date of her last menstrual cycle or any other information referring to her obstetrical and gynecological history. During the general clinical examination, we noticed an influenced general state, difficult cooperation, no fever, but with pale teguments and mucosa. Blood pressure was 140/90 mmHG, the heart rate was 140 beats per minute, the respiratory frequency was 20 per minute, O2 saturation was 100% with oxygen supply, with present intestinal transit, bladder catheter installed before transfer in our unit that showed present diuresis of 600 ml with concentrated urine aspect (urinary catheter was installed 4 hours previous of our consultation). Before the transfer to our hospital, she had three compresses applied intravaginally and an intravenous perfusion with one unit of a volemic substitute of plasma (500 ml) and one ampoule of etamsylate.
Local examination showed specific changes in accordance with the pregnancy status, such as enlarged breasts, enlarged abdomen surpassing the umbilicus with the presence of linea nigra and the presence of Pfannenstiel scar due to her two anterior caesarean interventions. Abdominal palpation allowed the medical team to feel an enlarged abdomen occupied by an ovoid mass, with smooth consistency, with its longitudinal axis surpassing the umbilicus with 2-3 cm.
Vaginal examination with valves was performed and, after the removal of the three compresses soaked with blood, it was observed the elimination of trophoblastic tissue, red blood and blood clots. The laboratory exams showed a hemoglobin level of 5.5 g/dL, hematocrit of 15.1%, coagulation blood tests within normal parameters, and a beta-HCG level of 202.1 mUI/ml.
Ultrasound examination revealed a uterus of 14/11 cm, with intrauterine inhomogeneous content similar to a bunch of grapes (Figure 1), right ovary with dimensions of 80/60 mm with polycystic aspect, and a left ovary with dimensions of 70/60 ml, also with polycystic aspect; no aspect of liquid was observed in the posterior cul de sac.
Fluid therapy measures with crystalloid and colloid solutions were started, and blood transfusion was initiated, with one unit of red blood cells concentrate and one unit of plasma. Hemostatic therapy was performed with two ampoules of etamsylate, one ampoule of vitamin K, and one ampoule of tranexamic acid. Prophylactic antibiotherapy and antihypertensive treatments were initiated.
The first maneuver consisted in the removal of all the trophoblastic tissue accumulated in the vaginal area (Figures 2 and 3); afterwards, with ultrasound guidance and intravenous infusion of oxytocin (5 U of oxytocin diluted in 500 ml of sodium chloride), the uterine cavity was evacuated through aspiration.

Results
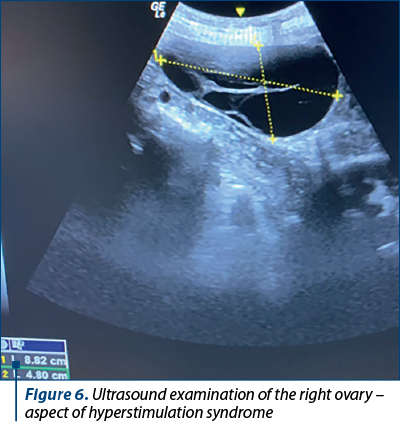
After the surgical intervention, a favorable evolution was noted, with significantly diminished genital bleeding, stable hemodynamic status, and the abdominal palpation confirmed the presence of a smaller, tonic and contractile uterus. Ultrasound examination certified the uterine evacuation (Figure 4) and the maintenance of enlarged right and left ovaries due to hyperstimulation syndrome (Figures 5 and 6).
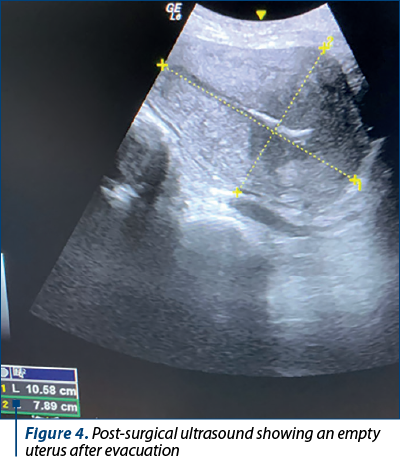
Through the entire period spent in our unit, the patient showed a good evolution: 24 hours after the intervention, the genital bleeding was unsignificant, she had a tonic uterus with blood pressure values in normal parameters under antihypertensive treatment, with a hemoglobin level of 8.1 g/dL and a hematocrit level of 25%; the coagulation parameters remained within normal values.
The anatomical pathology examination of the samples confirmed our diagnosis, and the microscopic examination of the tissular fragments showed numerous enlarged chorionic villi with significant hydropic alterations, presence of cisterna-like elements and marked trophoblastic hyperplasia with a tendency for circumferential array and frequent atypia cells. There was also noted the presence of large fibrinoid necrosis areas. Thoracic X-ray was performed after the uterine evacuation and revealed no sign of pulmonary metastasis. Abdominal ultrasound was also performed, with no particular signs to be noted.
A dose of 40 mg/m2 methotrexate was administered intramuscularly, but the medical follow-up in our unit was not possible. The patient required to be discharged against medical advice and desired to continue her medical follow-up within another local hospital. At discharge, she was strongly advised and counseled to continue the dosage of beta-HCG until nondetectable values, to perform another pelvic ultrasound in seven days, and to use a contraception method until negative beta-HCG values.
Although our patient tested positive for the infection with SARS-CoV-2, she showed no respiratory signs, no fever, no coughing, and the X-ray performed in search for metastasis showed no lesions specific for COVID-19.
Discussion
Molar pregnancies continue to pose a challenge for all obstetricians and the post-therapeutic follow-up of patients can sometimes be difficult. The management of such cases requires multidisciplinary teams. Our case had multiple features specific to this rare pathology, such as hypertension and ovarian hyperstimulation syndrome, features that are rarely encountered in this medical field due to early diagnosis. When considering her age of only 20 years old, we can consider it a risk factor, and we rememorize the Kohorn et al. study which brought strong evidence that patients younger than 21 years old have a higher risk for developing molar pregnancies. Offering medical education in rural areas should be a continuous effort, and advising pregnant patients to attend obstetrical consultations and prenatal checkups should represent a medical target, since diagnosing early could be life-saving in these cases. Since our patient had no obstetrical checkups, it was impossible to have a diagnosis, therefore this case had a prolonged evolution until diagnosis and treatment. Complications associated with this pathology, such as preeclampsia, hyperthyroid disease and large ovarian cysts, usually subside alongside uterine evacuation. The treatment with beta-adrenergics is sometimes necessary previous to surgical intervention in patients with induced hyperthyroid disease. For patients with nonmetastatic disease, usually a good prognostic is expected(5).
Conclusions
It is not the first, nor the last time obstetrical medical teams will have to manage such complicated cases, even though at first sight the management might seem easily applicable, the difficulty arises in fact from the complications of this pathology that might be life-threatening. Interdisciplinary management is needed in most cases, and transferring such cases in medical units that are able to offer the correct management should not be delayed.
Conflict of interest: none declared.
financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.

Bibliografie
-
Sarmadi S, Izadi-Mood N, Sanii S, Motevalli D. Inter-observer variability in the histologic criteria of diagnosis of hydatidiform moles. Malays J Pathol. 2019;41(1):15-24.
-
Chawla T, Bouchard-Fortier G, Turashvili G, Osborne R, Hack K, Glanc P. Gestational trophoblastic disease: an update. Abdom Radiol (NY). 2023;48(5):1793-815.
-
Braga A, Mora P, de Melo AC, Nogueira-Rodrigues A, Amim-Junior J, Rezende-Filho J, Seckl MJ. Challenges in the diagnosis and treatment of gestational trophoblastic neoplasia worldwide. World J Clin Oncol. 2019;10(2):28-37.
-
Yuk JS, Baek JC, Park JE, Jo HC, Park JK, Cho IA. Incidence of gestational trophoblastic disease in South Korea: a longitudinal, population-based study. Peer J. 2019;7:e6490.
-
Kohorn E. Practice Bulletin No. 53. Diagnosis and treatment of gestational trophoblastic disease. Obstet Gynecol. 2004;104(6):1422; author reply 1422-3.
-
Giacometti C, Bellan E, Ambrosi A, Dei Tos AP, Cassaro M, Ludwig K. “While there is p57, there is hope.” The past and the present of diagnosis in first trimester abortions: Diagnostic dilemmas and algorithmic approaches. A review. Placenta. 2021;116:31-7.
-
Ghassemzadeh S, Farci F, Kang M. Hydatidiform Mole. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2023 Jan. https://www.ncbi.nlm.nih.gov/books/NBK459155/
-
Benson CB, Genest DR, Bernstein MR, Soto-Wright V, Goldstein DP, Berkowitz RS. Sonographic appearance of first trimester complete hydatidiform moles. Ultrasound Obstet Gynecol. 2000;16(2):188-91.
-
Gadducci A, Carinelli S, Guerrieri ME, Aletti GD. Placental site trophoblastic tumor and epithelioid trophoblastic tumor: Clinical and pathological features, prognostic variables and treatment strategy. Gynecol Oncol. 2019;153(3):684-93.
-
Ning F, Hou H, Morse AN, Lash GE. Understanding and management of gestational trophoblastic disease. F1000Res. 2019;8:F1000 Faculty Rev-428.
-
Gerstl B, Sullivan E, Vallejo M, Koch J, Johnson M, Wand H, Webber K, Ives A, Anazodo A. Reproductive outcomes following treatment for a gynecological cancer diagnosis: a systematic review. J Cancer Surviv.2019;13(2):269-81.
-
Tidy JA, Gillespie AM, Bright N, Radstone CR, Coleman RE, Hancock BW. Gestational trophoblastic disease: a study of mode of evacuation and subsequent need for treatment with chemotherapy. Gynecol Oncol. 2000;78(3 Pt 1):309-12.
-
Albrecht C, Chamley L, Charnock-Jones DS, et al. IFPA meeting 2018 workshop report II: Abnormally invasive placenta; inflammation and infection; preeclampsia; gestational trophoblastic disease and drug delivery. Placenta. 2019;84:9-13.
-
Wreczycka-Cegielny P, Cegielny T, Oplawski M, Sawicki W, Kojs Z. Current treatment options for advanced choriocarcinoma on the basis of own case and review of the literature. Ginekol Pol. 2018;89(12):711-5.
-
Lurain JR. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol. 2010;203(6):531-9.
Articole din ediţiile anterioare
Principii de tratament cu metotrexat al sarcinii extrauterine necomplicate
Sarcina extrauterină reprezintă o urgenţă ginecologică severă care, în lipsa unui diagnostic stabilit corect şi rapid, precum şi a unei intervenţii...
Embolizarea în sarcina ectopică cervicală
Embolizarea arterelor uterine este o metodă minim invazivă, ce aparţine radiologiei intervenţionale, prin care se poate trata cu succes sarcina ect...